Abstract
The main aim of this article is to establish the actual prevalence of renal vein variations (circumaortic renal vein, retroaortic renal vein, double renal vein), and to increase awareness about them. To this purpose, we have performed a meta-analysis of prevalence, using the MetaXL package, We included 105 articles in the final analysis of prevalence, of which 88 contained data about retroaortic renal vein, 84 – about circumaortic renal vein, and 51 - about multiple renal veins. The overall prevalence for retroaortic renal vein was 3% (CI:2.4–3.6%), for circumaortic renal vein − 3.5% (CI:2.8–4.4%), and for multiple renal veins - 16.7% (14.3–19.2%), much higher on the right 16.6 (14.2–19.1%) than on the left side 2.1 (1.3–3.2%). The results were relatively homogenous between studies, with only a minor publication bias overall.
Similar content being viewed by others
Introduction
The anatomy of the renal veins was studied by many authors, due to its major implications in abdominal surgery (e.g. nephrectomy, in kidney transplantation). Knowledge regarding the morphology and prevalence of vascular abnormalities is also of an uttermost importance in laparoscopic surgery when entering the paraaortic region, as the repair of renal vessels is much more difficult compared to open surgery, often causing hemorrhage, a need for transfusion, or conversion to laparotomy1. Various anatomical variants of the renal veins were associated with varicocele2, nutcracker syndrome3, pelvic congestion syndrome3, hematuria, low-back pain4, or renal ectopy5. There are three main types of anatomical variants of renal veins: multiple renal veins, in which are identifiable two or more renal veins, either uni or bilaterally; retroaortic left renal vein (RLRV), in which the renal vein has a retroaortic course before entering the inferior vena cava; and circumaortic left renal vein (CLRV), in which there are two or more renal veins forming a ring around the aorta. The anatomy and surgery manuals often overlook these anatomical variants, increasing the risk for less experienced surgeons to damage them during surgery. The prevalence of the main anatomical variants of the renal vessels is variable in the scientific literature. For the RLRV the prevalence varies in different studies between under 1%6, and close to 10%7,8. For the CLRV, the quoted prevalence ranges from below 1%3,9,10 to over 15%11. Multiple renal veins (MRVs), have a prevalence ranging from 2%12 to over 40%13. The main aim of this article is to establish the actual prevalence of these anatomical variants (RLRV, CLRV, MRVs).
Materials and Methods
We performed the study according to the PRISMA guidelines for reporting systematic reviews and meta-analyzes of observational studies in epidemiology14.
Selection criteria
Inclusion criteria: studies that contained data from which could estimate the prevalence of the main renal vein variations: retroaortic left renal vein, circumaortic renal vein (renal vein collar), multiple renal veins, on various population groups. We used as exclusion criteria: (1) no relevant information to reconstruct the data needed for analysis; (2) studies made on less than 20 subjects; (3) case series/case reports. For articles not found in online databases, but for which we could obtain numerical data from secondary sources, we used the secondary source-based information.
Search method
We analyzed the results from three databases: Web of Science, Scopus, and Pubmed, by using the following keywords: “renal collar”, “Circumaortic renal vein”, “double renal vein” “retroaortic renal vein”, with a timeframe that ranged from the beginning of each database to May 2018. We preferred not to use additional, restrictive criteria (e.g. article type) as other assortments (letters, case presentations, reviews) might have added relevant data to the meta-analysis (discussions, finding other appropriate articles). The reference list of each relevant one was scrutinized for other relevant studies to be included in the meta-analysis. We imported the references, abstract and full text (if available) into the Mendeley Desktop software.
Data collection and analysis
For each study, two reviewers, working independently, performed the database research, extracted the data and included it in Excel Datasheets. If discrepancies were found, the articles into question were reviewed by a third reviewer. We summarized the following information: study, name of the authors, year, total number of cases, country, the general inclusion and exclusion criteria, the number of cases with various renal vein variations, including subtypes for RLRV, the gender for RLRV and CLRV, the detection method, the risk of bias, and the quality score. If the data was obtained from secondary sources, we only used the data that was available in these secondary sources and the risk of bias and the quality score were not computed.
Risk of bias
Two reviewers assessed separately the risk of bias qualitatively, based on a methods we have previously used in another meta-analyses of prevalence15. When the opinions of the two reviewers diverged, regarding the risk of bias of a specific study, a third reviewer reassessed the article, and decided the final risk of bias, used in our analysis. We analyzed selection bias (the presence of inclusion and exclusion criteria, type of study), multiple publication bias, measurement bias (method used, with autopsy and high-resolution CT imaging being considered having a lower bias compared to venography), statistical reporting bias (statistical analysis performed with the data, complete description of the data). Based on these elements, we separated the studies in three subgroups: high risk of bias, moderate risk of bias and low risk of bias. A high risk of bias was considered when the inclusion and exclusion criteria were undefined/improperly defined, authors have published more than one article on similar populations, the reviewers being unable to properly assess the clear separation of the study groups in different articles, the use of venography or low-resolution CT, the study was not performed specifically to assess the presence of venous structures, the data was very scarcely presented, the number of cases was low. A low risk of bias was assessed when the inclusion and exclusion criteria were properly defined, the variants were detected through high-resolution CT, anatomy or surgery, during studies aimed specifically for the detection of venous variants, the number of subjects was high. A moderate risk was assessed in studies with intermediate characteristics.
Quality assessment
We performed the quality assessment using four scales from the Quality in Prognostic Studies Tool16 (participants, outcome measurement, confounding, statistical analysis and reporting). For each remained subscale (study participation, prognostic factor measurement, outcome measurement, study confounding, statistical analysis and reporting), we graded each study as low quality (0 points), intermediate quality (1 point) or high quality (2 points). This method was previously used by the authors in meta-analyses of prevalence16.
Statistical analysis
We determined the effect size using a random effects model computed in Microsoft Excel 2016 with the MetaXL add-on version 5.3. For each group and subgroup, we performed a forest plot. For the analysis of publication bias, we used the funnel plot and the LFK index. For the prevalence analysis we performed the double arcsin prevalence transformation, we used a continuity correction of 0.5 and 95% confidence intervals. Forest plots were done using Microsoft Excel 2016 with the MetaXL add-on 5.3. The actual prevalence can be obtained by multiplying with 100 the results from the meta-analysis of prevalence.
Results
Search synthesis
During the initial database research, we obtained 2586 (Table 1) articles from which, after deleting duplicates and irrelevant studies we selected 132 to be further scrutinized (128 by the first reviewer, 123 by the second, 119 being common). By analyzing their references, we found another 32 potentially relevant articles that were also downloaded (30 and 32 articles, by reviewer 1 and 2, respectively). From the 164 articles, 105 were included in the final analysis of prevalence, of which 88 contained data about RLRV, 84 – about CLRV, and 51 about multiple RVs. Details about the search synthesis are presented in Fig. 1. We detailed the papers contained in the meta-analysis in Table 2.
Search synthesis. PRISMA flow diagram. The PRISMA Statement and the PRISMA Explanation and Elaboration document are distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Quality and risk of bias
Based on the inclusion criteria, we obtained a total number of 105 studies, of which of a high quality (between 6 and 8 points) were considered 28 articles, of a medium quality (between 3 and 5 points) – 39 articles, of a low quality (between 0 and 2 points) – 21 articles, and for 17 we could not obtain a full electronic text of the manuscript, and therefore the quality score could not be computed. A low bias was assessed in 19 articles, a moderate bias in 53, and a high bias in 17. The number of studies included for each sub-analysis is presented in the respective subheading.
Retroaortic left renal vein
A total number of 88 studies allowed us to estimate the prevalence of RLRV, containing 47461 subjects, of which 1287 were positive. The overall prevalence for RLRV was 0.030 (CI:0.024–0.036) (Fig. 2). The publication bias was minor, with an LFK index of 1.87. See also Fig. 3 (funnel plot). By comparing the prevalence depending on the method, we found very similar results, with a prevalence of 0.031 (0.022–0.041) for autopsy, 0.035 (0.024–0.046) for CT, and 0.02 (0.013–0.28) for surgery. Nineteen studies separated the cases based on gender. For men, the overall prevalence was 0.036 (0.026–0.048), while for women – 0.031 (0.019–0.046).
Circumaortic renal vein
A total number of 84 studies allowed us to estimate the prevalence of CLRV, containing 46256 subjects, of which 980 were positive. The overall prevalence for CLRV was 0.035 (CI:0.028–0.044) (Fig. 4). The publication bias was important, with a high number of studies being to the right of the funnel (Fig. 5), and having an LFK index of 4.24, suggesting major asymmetry. By comparing the prevalence depending on the method, we found for the autopsy group, a prevalence twice as high compared to CT and surgery, namely a prevalence of 0.05 (0.035–0.066) for autopsy, 0.026 (0.018–0.035) for CT, and 0.021 (0.005–0.040) for surgery. Fourteen studies separated the cases based on gender. For men, the overall prevalence was 0.036 (0.024–0.049), while for women −0.027 (0.014–0.042).
Multiple renal veins
A total number of 51 articles allowed us to estimate the prevalence of double renal veins, containing 12773 subjects. Multiple renal veins were identified in 2241 cases, of which 1762 on the right side (RRV) and 221 on the left side (LRV). Double renal veins were encountered in 1450 cases (1317 on the right and 133 on the left side), and triple renal veins in 247 (170 on the right and 77 on the left). The overall prevalence of multiple renal veins was 0.167 (0.143–0.192) (Fig. 6). The publication bias was minor (Fig. 7), and an LFK Index of −1.04, suggesting minor asymmetry. Forty-two studies had data about multiple left renal veins. The overall prevalence was 0.021 (0.013–0.032) (Fig. 8), and publication bias was absent (LFK Index = 0.67, suggesting no asymmetry). Forty-four studies had data about multiple right renal veins. The overall prevalence was 0.166 (0.142–0.191) (Figs 9 and 10), and publication bias was −0.26, suggesting no asymmetry. The prevalence of double and triple renal veins is presented in Table 3.
Discussions
Our study is the first one to properly assess, using a statistical method, the prevalence of three main anatomical variants of the renal veins, namely RLRV, CLRV and MRVs.
These anatomical variants are important for surgeons, as their presence can alter the surgery protocol, and for clinicians, as they might lead to unforeseen clinical manifestations of various disorders (see Table 4 for details). In kidney donation, the morphology and size of the renal vessels is extremely important, as short vessels could increase the difficulty of vascular anastomosis and increase the warm ischemia time during the intervention17.
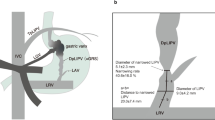
RRV is usually located anterior or inferior from the right renal artery18. RRV has less often an extrahilar origin (77.9%), compared to LRV (82.7%)18. It has an average length of 3.2cm19. Various studies showed RRV to be more often multiple, compared to the LRV; the main reason postulated for the increased prevalence of double RRV compared to LRV is the complex embryogenesis on the left side, discouraging the retention of additional left-sided renal veins20. Our study showed an overall prevalence of 16.7% for multiple renal veins, which were about eight times more frequent on the right compared to the left side. In kidney donors, the left one is preferable to be donated, due to a longer vascular pedicle. However, if the left kidney has a more complex vascular anatomy, the right one should be harvested. If the donor has one or both kidneys abnormal, the most normal remains to the donor, and the more abnormal one is given to the recipient21. Before donation, a complete imaging characterization of the kidneys and the vasculature should be performed, ideally through CT angiography, which yields data about the anatomy and variations of the renal vessels21. Some authors consider double right renal veins are a contraindication for donor nephrectomy, due to a higher risk of graft renal vein thrombosis22.
LRV can have either an intra or an extrarenal origin, with two or three main tributaries17,23, and is located anterior, or inferior of the renal artery, or it may run obliquely towards the IVC18,24. It has an average length of 8.4cm19, being much larger compared to the RRV, due to the abdominal topography of the IVC. The scientific literature has shown LRV to be less often double, but to present other variants, such as CLRV or RLRV.
According to Gillot, there are three main types of CLRV: (1) CLRV with partial distal bifidity, in which the retroaortic branch receives the root of the hemiazygos; (2) CLRV with partial proximal bifidity, a more common variant, in which the origin is separated, and the two branches join together in front of the aorta; (3) complete CLRV, in which we have two thick venous trunks that are leaving the hilum, and they remain separated until their ending in the IVC. This type has two subtypes: (a) inferior polar, in which the main vein, the superior one is preaortic, and the inferior polar vein is retroaortic; (b) superior polar, in which the main trunk is horizontal, preaortic; it receives the adrenal and sometimes the gonadal gland. The superior polar vein is retroaortic, and usually has an oblique, inferior course toward the IVC25. The actual prevalence of the CLRV depends on the attention with which the LRV is analyzed; if we were to consider all small retroaortic vessels draining into the IVC or LRV, the prevalence can be as high as 16%26,27. Other authors only included in the CLRV large, persistent collars, importantly decreasing the overall prevalence27. Our study confirmed a high variability regarding the reported prevalence of the CLRV and showed its actual prevalence to be around 3.5%.
RLRV can be classified in: RLRV Type 1, caused by the persistence of the left subsupracardinal anastomosis, the intersupracardinal anastomosis and the left dorsal renal vein, associated with the obliteration of the ventral left renal vein, leading to a retroaortic, orthotopic course for the LRV; RLRV Type 2, caused by the persistence of the subsupracardinal anastomosis on the left side, and of the left supracardinal vein, associated with the obliteration of the intersubcardinal and intersupracardinal anastomoses, leading to the appearance of a single retroaortic left renal vein lying at the L4-L5 level, where it joins the gonadal and ascending lumbar veins10; RLRV type III (CLRV); RLRV Type 4, in which the RLRV joins the left common iliac vein9, due to an obliteration of the ventral preaortic limb of the left renal vein28. The number of studies separating RLRVs into subtypes was small (five); additionally, some authors only scrutinized the first two subtypes, while other analyzed all four subtypes, and therefore we could not do a proper analysis of the prevalence on subtypes of RLRV.
Besides MRVs, RLRV, and CLRV, some authors described other variants, such as the presence of a plexiform left renal vein, with division after emerging from the renal hilum, followed by a redivision and a distal unification in a single terminal renal vein29.
The clinical consequences of renal vein abnormalities have been intensely studied; however, for many of them the scientific proofs are not definite. Their presence is however extremely important in the surgery of the abdomen, where they can be associated with significant complications, or the need to change the surgical approach. The main implications of these abnormalities are presented in Table 4.
The most important factor causing heterogeneity of the results regarding the prevalence of these variants is, most likely, represented by a variable number of false negative results, the variants being more easily overlooked when not specifically searched for.
Limitations
Some studies did not specified number of cases, but rather a prevalence in percentage17; our reconstruction of primary data was done strictly arithmetical, by multiplying the total number of subjects with the percentage/100, with rounding to the superior value in the obtained number was above 0.5 and to the inferior value if the obtained number was below 0.5. The definition of various anatomical variants, and their classification, differed from study to study, and often there was no detailed description of the variant; therefore, our interpretation might not be exact (e.g. some studies included CLRV in the RLRV category), some studies included all CLRVs in their analysis while other included only those CLRV with both trunks of increased size, etc. Small retroaortic renal veins can be obscured due to volume averaging or limited resolution of the imaging techniques30. Many included studies were not designed specifically for the detection of caval abnormalities; many were retrospective, and included patients that were referred for abdominal or pelvic symptoms/disorders.
Conclusions
The overall prevalence for RLRV is 3%, for CLRV −3.5%, and for MRVs −16.7%, much higher for the right (16.6%), compared to the left renal vein (2.1%).
References
Klemm, P., Fröber, R., Köhler, C. & Schneider, A. Vascular anomalies in the paraaortic region diagnosed by laparoscopy in patients with gynaecologic malignancies. Gynecol. Oncol. 96, 278–282 (2005).
Arslan, H. et al. Incidence of retro-aortic left renal vein and its relationship with varicocele. Eur. Radiol. 15, 1717–1720 (2005).
Atalar, M. H., Kosar, M. I., Salk, I. & Isleyen, M. Left renal vein abnormalities detected during routine abdominal computed tomography imaging: Clinico-radiological significance. Folia Morphol. 71, 168–172 (2012).
Gibo, M. & Onitsuka, H. Retroaortic left renal vein with renal vein hypertension causing hematuria. Clin. Imaging 22, 422–424 (1998).
Macchi, V., Parenti, A. & De Caro, R. Draining of a retroaortic left renal vein via the ‘subcentral veins’ into the inferior vena cava. J. Anat. 199, 621–623 (2001).
Satyapal, K. S. et al. Left renal vein variations. Surg. Radiol. Anat. 21, 77–81 (1999).
Schmidt, G. P. & Loeweneck, H. Über die Häufigkeit der linken retroaortären Nierenvene bei Erwachsenen. Urol. Int. 30, 332–340 (1975).
Casadiego Duran, J. T. & Ferreira Arquez, H. Anatomical Study of Retro-Aortic Left Renal Vein. J. Chem. Pharm. Res. 8, 1011–1018 (2016).
Karaman, B. et al. Retroaortic left renal vein: Multidetector computed tomography angiography findings and its clinical importance. Acta radiol. 48, 355–360 (2007).
Hoeltl, W., Hruby, W. & Aharinejad, S. Renal vein anatomy and its implications for retroperitoneal surgery. J. Urol. 143, 1108–1114 (1990).
Pick, J. W. & Anson, B. J. The Renal Vascular Pedicle: An Anatomical Study of 430 Body-Halves. J. Urol. 40, 411–434 (1940).
Shaheen, R. & Jamil, M. N. Anatomical pattern and variations of left renal vein. Med. Forum Mon. 29, 17–21 (2018).
Eisendrath, D. N. The relation of variations in the renal vessels to pyelotomy and nephrectomy. Ann. Surg. 71, 726 (1920).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, T. P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLOS Med. 6, e1000097 (2009).
Hayden, J. A., van der Windt, D. A., Cartwright, J. L., Côté, P. & Bombardier, C. Assessing Bias in Studies of Prognostic Factors. Ann. Intern. Med. 158, 280 (2013).
Hostiuc, S., Negoi, I., Rusu, M. C. & Hostiuc, M. Myocardial Bridging: A Meta-Analysis of Prevalence. J. Forensic Sci. 63, 1176–1185 (2018).
Janschek, E. C. S. et al. Anatomic basis of right renal vein extension for cadaveric kidney transplantation. Urology 63, 660–664 (2004).
Ballesteros, L. E., Saldarriaga, V. & Ramirez, L. M. Morphologic evaluation of the renal veins: A study with autopsy material from Colombian subjects. Rom. J. Morphol. Embryol. 55, 77–81 (2014).
Anson, B. J. & Daseler, E. H. Common variations in renal anatomy, affecting blood supply, form, and topography. Surg. Gynecol. Obstet. 112, 439 (1961).
Mankhause, W. S. & Khalique, A. The adrenal and renal mass and their connection with Azygos and lumber vein. J Anat 146, 105–115 (1986).
Apisarnthanarak, P., Suvannarerg, V., Muangsomboon, K., Taweemonkongsap, T. & Hargrove, N. S. Renal vascular variants in living related renal donors: Evaluation with CT angiography. J. Med. Assoc. Thail. 95, 941–948 (2012).
Mandal, A. K., Cohen, C., Montgomery, R. A., Kavoussi, L. R. & Ratner, L. E. Should the indications for laparascopic live donor nephrectomy of the right kidney be the same as for the open procedure? Anomalous left renal vasculature is not a contraindiction to laparoscopic left donor nephrectomy. Transplantation 71, 660–4 (2001).
Duques, P., Rodrigues, J. R., Neto da Silva, F. B., Neto, E. M. V. S. & de Toledo, E. S. Estudo anatômico da veia renal esquerda de cadáveres humanos brasileiros. 184–191 (2002).
Satyapal, K. S. & Africa, S. Classification of the drainage patterns of the renal veins. 329–333 (1995).
Gillot, C. La veine renale gauche. Anat. Clin. 1, 135–155 (1978).
Thomas, T. V. Surgical implications of retroaortic left renal vein. Arch. Surg. 100, 738–740 (1970).
Brener, B. J., Darling, R. C., Frederick, P. L. & Linton, R. R. Major Venous Anomalies Complicating Abdominal Aortic Surgery. Arch. Surg. 108, 159–165 (1974).
Brancatelli, G. et al. Case report Retroaortic left renal vein joining the left common iliac vein. Eur. Radiol. 1725, 1724–1725 (2000).
Gupta, A., Gupta, R. & Singal, R. Congenital variations of renal veins: Embryological Background and clinical implications. J. Clin. Diagnostic Res. 5, 1140–1143 (2012).
Kaufman, J. A., Waltman, A. C., Rivitz, S. M. & Geller, S. C. Anatomical observations on the renal veins and inferior vena cava at magnetic resonance angiography. Cardiovasc. Intervent. Radiol. 18, 153–157 (1995).
Alexander, E. S., Clark, R. A., Gross, B. H. & Colley, D. P. CT of congenital anomalies of the inferior vena cava. Comput. Radiol. 6, 219–226 (1982).
Aljabri, B. et al. Incidence of major venous and renal anomalies relevant to aortoiliac surgery as demonstrated by computed tomography. Ann. Vasc. Surg. 15, 615–618 (2001).
Anson, B. J. & Cauldwell, E. W. The pararenal vascular system a study of 425 anatomical specimens. Q. Bull. Northwest. Univ. Med. Sch. 21, 320–8 (1947).
Ayaz, S. & Ayaz, U. Y. Detection of retroaortic left renal vein and circumaortic left renal vein by PET/CT images to avoid misdiagnosis and support possible surgical procedures. Hell. J. Nucl. Med. 19, 135–139 (2016).
Baptista-Silva, J. C. C., Veríssimo, M. J., Castro, M. J., Câmara Guimarães, L. A. & Pestana Medina, J. O. Anatomical study of the renal veins observed during 342 living-donor nephrectomies. Sao Paulo Med. Journall 115, 1456–1459 (1997).
Beckmann, C. F. & Abrams, H. L. Renal venography: Anatomy, technique, applications, analysis of 132 venograms, and a review of the literature. Cardiovasc. Intervent. Radiol. 3, 45–70 (1980).
Benedetti-Panici, P., Maneschi, F., Scambia, G., Greggi, S. & Mancuso, S. Anatomic abnormalities of the retroperitoneum encountered during aortic and pelvic lymphadenectomy. Am. J. Obstet. Gynecol. 170, 111–116 (1994).
Bouali, O. et al. Anatomic variations of the renal vessels: Focus on the precaval right renal artery. Surg. Radiol. Anat. 34, 441–446 (2012).
Boyaci, N., Karakas, E., Dokumacı, D. S., Yildiz, S. & Cece, H. Evaluation of left renal vein and inferior vena cava variations through routine abdominal multi-slice computed tomography. Folia Morphol. (Warsz). 73, 159–163 (2014).
Çlnar, C. & Türkvatan, A. Prevalence of renal vascular variations: Evaluation with MDCT angiography. Diagn. Interv. Imaging 97, 891–897 (2016).
Costa, H. C. et al. Anatomic variations in vascular and collecting systems of kidneys from deceased donors. Transplant. Proc. 43, 61–63 (2011).
Davis, R. A., Milloy, J. F. J. & Anson, B. J. Lumbar, renal, and associated parietal and visceral veins based upon a study of 100 specimens. Surg. Gynecol. Obstet. 107, 1–22 (1958).
Davis, C. J. & Lundberg, G. D. Retroaortic Left Renal Vein. A relatively frequent anomaly. Am. J. Clin. Pathol. 50, 700–703 (1968).
Dilli, A., Ayaz, U. Y., Karabacak, O. R., Tatar, I. G. & Hekimoglu, B. Study of the left renal variations by means of magnetic resonance imaging. Surg. Radiol. Anat. 34, 267–270 (2012).
Dilli, A., Ayaz, U. Y., Kaplanoǧlu, H., Saltas, H. & Hekimoglu, B. Evaluation of the left renal vein variations and inferior vena cava variations by means of helical computed tomography. Clin. Imaging 37, 530–535 (2013).
Ellis, J. H., Denham, J. S., Bies, J. R., Olson, E. W. & Cory, D. A. Magnetic resonance imaging of systemic venous anomalies. Comput. Radiol. 10, 15–22 (1986).
Fagarasanu, I. Recherches anatomiques sur la veine renale gauche et ses collaterales; leurs rapports avec la pathogenie du varicocele essential et des varices du ligament large. Demonstr. Exp. Ann Anat Pathol 15, 9–52 (1938).
Froriep, A. & Froriep, L. Über eine verhältnismäßig häufige Varietät im Bereich der unteren Hohlvene. Anat. Anz 10, 574–583 (1895).
Gérard, G. Mention d’une anastomose veineuse réno-cave rétroaortique obliquement descendante. CR Soc. Biol.(Paris) 83, 185–186 (1920).
Gillaspie, C., Miller, L. I. & Baskin, M. Anomalous renal vessels and their surgical significance. Anat. Rec. 11, 77–86 (1916).
Hassan, S. S., El-Shaarawy, E. A., Johnson, J. C., Youakim, M. F. & Ettarh, R. Incidence of variations in human cadaveric renal vessels. Folia Morphol. 76, 394–407 (2017).
Heidler, S. et al. Prevalence and incidence of clinical symptoms of the retroaortic left renal vein. Urol. Int. 94, 173–176 (2015).
Hicks, M. E., Malden, E. S., Vesely, T. M., Picus, D. & Darcy, M. D. Prospective Anatomic Study of the Inferior Vena Cava and Renal Veins: Comparison of Selective Renal Venography with Cavography and Relevance in Filter Placement. J. Vasc. Interv. Radiol. 6, 721–729 (1995).
Holden, A., Smith, A., Dukes, P., Pilmore, H. & Yasutomi, M. Assessment of 100 Live Potential Renal Donors for Laparoscopic Nephrectomy with Multi–Detector Row Helical CT. Radiology 237, 973–980 (2005).
Holt, P. J., Adshead, J. M., Filiadis, I. & Christmas, T. J. Retroperitoneal anomalies in men with testicular germ cell tumours. BJU Int. 99, 344–346 (2007).
Karazincir, S., Balci, A., Görür, S., Sumbas, H. & Kiper, A. N. Incidence of the retroaortic left renal vein in patients with varicocele. J. Ultrasound Med. 26, 601–604 (2007).
Kawamoto, S., Lawler, L. P. & Fishman, E. K. Evaluation of the renal venous system on late arterial and venous phase images with MDCT angiography in potential living laparoscopic renal donors. Am. J. Roentgenol. 184, 539–545 (2005).
Koc, Z., Ulusan, S., Oguzkurt, L. & Tokmak, N. Venous variants and anomalies on routine abdominal multi-detector row CT. Eur. J. Radiol. 61, 267–278 (2007).
Kramer, B. The incidence of the renal venous collar in South African blacks. South African Med. journal = Suid-Afrikaanse Tydskr. vir Geneeskd. 57, 875–876 (1980).
Kulkarni, S. et al. Multidetector CT angiography in living donor renal transplantation: Accuracy and discrepancies in right venous anatomy. Clin. Transplant. 25, 77–82 (2011).
Kumaresan, M., Pk, S., Gunapriya, R., Karthikeyan, G. & Priyadarshini, A. Morphometric study of renal vein and its variations using CT. Indian J. Med. Res. Pharm. Sci. 3, 41–49 (2016).
Lien, H. H. & Kolbenstvedt, A. Phlebographic appearances of the left renal and left testicular veins. Acta radiol. 18, 321–332 (1977).
Lin, C. H. et al. Laparoscopic live donor nephrectomy in the presence of circumaortic or retroaortic left renal vein. J. Urol. 171, 44–46 (2004).
Martinez-Almagro, A., Almenar Garcia, V., Martinez Sanjuan, V., Hernandez Gil de Tejada, T. & Lorente Montalvo, P. Retroaortic left renal vein: a report of six cases. Surg. Radiol. Anat. 14, 361–6 (1992).
Mayo, J. et al. Anomalies of the inferior vena cava. Am. J. Roentgenol. 140, 339–345 (1983).
Satyapal, K. S., Rambiritch, V. & Pillai, G. Additional renal veins: Incidence and morphometry. Clin. Anat. 8, 51–55 (1995).
Monkhouse, W. & Khalique, A. The adrenal and renal veins of man and their connections with azygos and lumbar veins. J. Anat. 25, 105–115 (1986).
Mosnier, H., Frantz, P., Calmat, A. & Cabrol, A. L. C. Etude des anastomoses entre la veine renale gauche et les plexus intra-rachidiens. 324, 9–12 (1979).
Namasivayam, S., Kalra, M. K., Waldrop, S. M., Mittal, P. K. & Small, W. C. Multidetector row CT angiography of living related renal donors: Is there a need for venous phase imaging? Eur. J. Radiol. 59, 442–452 (2006).
Namburu, P. S. B. A study of renal veins. Int. J. Anat. Res. 5, 4463–4468 (2017).
Natsis, K. et al. Proposal for classification of the circumaortic renal collar’s morphology. Am. Surg. 74, 1190–1194 (2008).
Nishimura, Y. et al. Left renal vein hypertension in patients with left renal bleeding of unknown origin. Radiology 160, 663–667 (1986).
Okamoto, K. The Posterior Renal Vein (New Definition), together with its Morphological Significance. Okajimas Folia Anat. Jpn. 67, 203–218 (1990).
Ortmann, R. Ü. B. Häufigkeit und Variationsbild der linken retro-aortären Nierenvene. Z. Anat. Entwicklungsgesch. 127, 346–358 (1968).
Pandya, V., Patel, A., Sutariya, H. & Gandhi, S. Evaluation of renal vascular anatomy in live renal donors: Role of multi detector computed tomography. Urol. Ann. 8, 270 (2016).
Pollak, R., Prusak, B. F. & Mozes, M. F. Anatomic abnormalities of cadaver kidneys procured for purposes of transplantation. Am. Surg. 52, 233 (1986).
Poyraz, A. K., Firdolas, F., Onur, M. R. & Kocakoc, E. Evaluation of left renal vein entrapment using multidetector computed tomography. Acta radiol. 54, 144–148 (2013).
Pozniak, M. A. et al. CT angiography of potential renal transplant donors. Radiographics 18, 565–587 (1998).
Raman, S. S. et al. Surgically relevant normal and variant renal parenchymal and vascular anatomy in preoperative 16-MDCT evaluation of potential laparoscopic renal donors. Am. J. Roentgenol. 188, 105–114 (2007).
Rashid, R. J. et al. Diagnostic accuracy of 64-MDCT angiography in the preoperative evaluation of renal vessels and compared with laparotomy findings in living donor kidney. Ren. Fail. 36, 327–331 (2014).
Reed, M. D., Friedman, A. C. & Nealey, P. Anomalies of the left renal vein: analysis of 433 CT scans. J. Comput. Assist. Tomogr. 6, 1124–1126 (1982).
Reginelli, A. et al. Renovascular anatomic variants at CT angiography. Int. Angiol. 34, 36–42 (2015).
Reis, R. H. & Esenther, G. Variations in the pattern of renal vessels and their relation to the type of posterior vena cava in man. Dev. Dyn. 104, 295–318 (1959).
Resorlu, M. et al. Association of congenital left renal vein anomalies and unexplained hematuria: Multidetector computed tomography findings. Urol. Int. 94, 177–180 (2015).
Ross, J. A., Samuel, E. & Millar, D. R. Variations in the renal vascular pedicle: (An Anatomical and Radiological Study with Particular Reference to Renal Transplantation). Br. J. Urol. 33, 478–485 (1961).
Royster, T. S., Lacey, L. & Marks, R. A. Abdominal aortic surgery and the left renal vein. Am. J. Surg. 127, 552–554 (1974).
Rydberg, J. et al. Evaluation of Prospective Living Renal Donors for Laparoscopic Nephrectomy with Multisection CT: The Marriage of Minimally Invasive Imaging with Minimally Invasive Surgery. RadioGraphics 21, S223–S236 (2001).
Sahani, D. V. et al. Multi–Detector Row CT in Evaluation of 94 Living Renal Donors by Readers with Varied Experience. Radiology 235, 905–910 (2005).
Sasaki, T. M. et al. Is laparoscopic donor nephrectomy the new criterion standard? Arch. Surg. 135, 943–7 (2000).
Seib, G. A. The azygos system of veins in American whites and American negroes, including observations on the inferior caval venous system. Am. J. Phys. Anthropol. 19, 39–163 (1934).
Shindo, S. et al. Anomalies of inferior vena cava and left renal vein: risks in aortic surgery. Ann Vasc Surg 14, 393–396 (2000).
Soloweitschick. Zur Frage über die Anomalien der Nierenvenen. In Congr Int Med 1355–1358 (1899).
Sośnik, H. & Sośnik, K. Renal vascularization anomalies in the Polish population. Congenital anomalies of the renal veins. Pol. Przegl. Chir. 89, 26–30 (2017).
Srinivasan, R. The left renal vein. Mt. Sinai J. Med. 46, 559–63 (1979).
Yi, S. Q., Ueno, Y., Naito, M., Ozaki, N. & Itoh, M. The three most common variations of the left renal vein: A review and meta-analysis. Surg. Radiol. Anat. 34, 799–804 (2012).
Staśkiewicz, G. et al. Supernumerary renal vessels: Analysis of frequency and configuration in 996 computed tomography studies. Folia Morphol. 75, 245–250 (2016).
Șahin, C., Kaçira, O. K. & Tüney, D. The retroaortic left renal vein abnormalities in cross-sectional imaging. Folia Med. (Plovdiv). 56, 38–42 (2014).
Tao, X.-F. et al. Dual-energy computed tomography angiography for evaluating the renal vascular variants. Chin. Med. J. (Engl). 126, 650–654 (2013).
Tombul, S. T. et al. Preoperative Evaluation of Hilar Vessel Anatomy With 3-D Computerized Tomography in Living Kidney Donors. Transplant. Proc. 40, 47–49 (2008).
Trigaux, J.-P., Vandroogenbroek, S., de Wispelaere, J.-F., Lacrosse, M. & Jamart, J. Congenital Anomalies of the Inferior Vena Cava and Left Renal Vein: Evaluation with Spiral CT. J. Vasc. Interv. Radiol. 9, 339–345 (1998).
Türkvatan, A., Akinci, S., Yildiz, S., Olçer, T. & Cumhur, T. Multidetector computed tomography for preoperative evaluation of vascular anatomy in living renal donors. Surg. Radiol. Anat. 31, 227–35 (2009).
Weinstein, B. B., Countiss, E. H. & Derbes, V. J. The renal vessels in 203 cadavers. Urol. Cutan. Rev 44, 137–139 (1940).
Yagci, A. B., Tavasli, B., Karabulut, N. & Kiroglu, Y. Clinical significance and renal haemodynamics of incidentally detected retroaortic left renal vein: Assessment with venous Doppler sonography. Br. J. Radiol. 81, 187–191 (2008).
Yeh, B. M., Coakley, F. V., Meng, M. V., Breiman, R. S. & Stoller, M. L. Precaval Right Renal Arteries: Prevalence and Morphologic Associations at Spiral CT. Radiology 230, 429–433 (2004).
Yeşildağ, A. et al. Rutin abdomen BT’de sol renal ven anomalilerinin görülme sıklığı. Tanısal ve Girişimsel Radyoloji 10, 140–143 (2004).
Yoshinaga, K., Kawai, K. & Kodama, K. An anatomical study of the retroaortic left renal vein. Okajimas Folia Anat. Jpn. 77, 47–52 (2000).
Zamboni, G. A., Romero, J. Y. & Raptopoulos, V. D. Combined vascular-excretory phase MDCT angiography in the preoperative evaluation of renal donors. Am. J. Roentgenol. 194, 145–150 (2010).
Zhu, J., Zhang, L., Yang, Z., Zhou, H. & Tang, G. Classification of the renal vein variations: a study with multidetector computed tomography. Surg. Radiol. Anat. 37, 667–675 (2015).
Zumstein, J. Zur Anatomie und Entwickelung des Venensystems des Menschen. Anat. Hefte 6, 572–608 (1896).
Anson, B. J., Richardson, G. A. & Minear, W. L. Variations in the Number and Arrangement of the Renal Vessels: A Study of the Blood Supply of Four Hundred Kidneys1. J. Urol. 36, 211–219 (1936).
Lord, J. W., Vigorita, J. & Florio, J. Fistula Between Abdominal Aortic Aneurysm and Anomalous Renal Vein. JAMA J. Am. Med. Assoc. 187, 535–536 (1964).
Horan, D. P. & Sharp, J. H. Spontaneous fistula between the aorta and left renal vein. Am. J. Surg. 113, 802–806 (1967).
Cuéllar i Calàbria, H. et al. Nutcracker or left renal vein compression phenomenon: Multidetector computed tomography findings and clinical significance. Eur. Radiol. 15, 1745–1751 (2005).
Chuang, V. P., Mena, C. E. & Hoskins, P. A. Congenital anomalies of the inferior vena cava. Review of embryogenesis and presentation of a simplified classification. Br. J. Radiol. 47, 206–213 (1974).
Author information
Authors and Affiliations
Contributions
All authors participated equally in the design of the study, drafting the manuscript and researching relevant information, and agreeing with the final version.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hostiuc, S., Rusu, M.C., Negoi, I. et al. Anatomical variants of renal veins: A meta-analysis of prevalence. Sci Rep 9, 10802 (2019). https://doi.org/10.1038/s41598-019-47280-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-47280-8
This article is cited by
-
The anterior communicating artery variants: a meta-analysis with a proposed classification system
Surgical and Radiologic Anatomy (2024)
-
A Practical Guide for Left Adrenal Vein Sampling in Patients with Left Renal Vein Variants
CardioVascular and Interventional Radiology (2023)
-
Left renal vein graft and in situ hepatic perfusion in hepatectomy for complete tumor invasion of hepatic veins: hemodynamic optimization and surgical technique
Langenbeck's Archives of Surgery (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.