Abstract
Our study aimed to estimate the prevalence of total free flap failure following free flap reconstruction for mandibular osteoradionecrosis (mORN) and assess the impact of potential moderators on this outcome. A comprehensive systematic literature search was independently conducted by two reviewers using the Medline, Scopus, Web of Science and Cochrane Library databases. Quality assessment of the selected studies was performed, and prevalence estimates with 95% confidence intervals (CI) were calculated. Outlier and influential analyses were conducted, and meta-regression analyses was employed to investigate the effects of continuous variables on the estimated prevalence. Ultimately, forty-six eligible studies (involving 1292 participants and 1344 free flaps) were included in our meta-analysis. The findings of our study revealed a prevalence of 3.1% (95% CI 1.3–5.4%) for total free flap failure after reconstruction for mORN. No study was identified as critically influential, and meta-regression analysis did not pinpoint any potential sources of heterogeneity. These findings provide valuable insights for researchers and serve as a foundation for future investigations into the management of mandibular osteoradionecrosis and the prevention of free flap failure in this context.
Similar content being viewed by others
Introduction
Head and neck cancer constitutes a heterogeneous group of malignancies, derived from the lips and oral cavity, the salivary glands, the nasopharynx, the oropharynx, the hypopharynx and the larynx with an estimation of 377.713, 53.583, 133.354, 98.412, 84.254 and 184.615 new cases in 2020, respectively1,2. Early or advanced stages of oral and oropharyngeal cancers could be benefited from definite or adjunctive ionizing radiation therapy3. Under not specified timeframe, mandibular osteoradionecrosis (mORN) may occur, consisting of a serious complication which can adversely affect the patients’ quality of life, functionality and both personal and healthcare expenditure4,5. Osteoradionecrosis (ORN) of the jaws is characterized by the presence of exposed bone that has been subjected to radiation and does not show signs of healing for at least three months, in the absence of any ongoing or recurring cancer. When ORN is diagnosed, the bone damage may be either superficial or extensive, and the condition can either progress gradually or rapidly advance, potentially resulting in a pathological fracture6. The prevalence of ORN varies considerably in the scientific literature, ranging from 0.4 to 56% and it can manifest spontaneously or induced by a mechanical injury (e.g. tooth extraction)6. Regarding the pathophysiological mechanism involved, Marx suggests that the radiation exposure could lead to mandible’s microvascular thrombosis, endothelial death and surrounding tissue fibrosis, causing tissue breakdown and eventually non healing wound formation7. Many risk factors that could contribute to its demonstration have been identified throughout the years such as high dose of ionizing irradiation, pre radiotherapy surgical treatment, primary tumor site, trauma (dental extraction), smoking status, male sex, older age, alcohol consumption and poor dental hygiene5,8,9 Among the great variety of signs and symptoms of mORN that may occur, an unhealed painful oral lesion is the predominant one. Others include dysaesthesia, odynophagia, malocclusion, trismus, pathological fractures, infections and orocutaneous fistula formation6. The main diagnostic procedure used, is a combination of patient’s medical history and clinical examination, therefore the physician should be able to identify all the relevant clinical findings. Radiographic imaging (panographic radiographs, computed tomography of the mandible) as well as biopsy of the wound, could only be used as methods in establishing the diagnosis. Regarding the treatment of mORN, conservative treatment, surgical intervention (minor or major) and hyperbaric oxygen (HBO) are the available options5. Resection of the affected tissue and microvascular free flap reconstruction comprise the standard of care for severely affected cases of mORN. Mainly, the free tissue could be harvested through the fibula, iliac crest, scapula and the forearm. However, as with any surgical intervention many complications could arise such as total free flap failure, partial free flap failure and recurrence of mORN. To gain an accurate and reliable estimation regarding the prevalence of the free flap failure after free flap reconstruction for mORN, we conduct a systematic review and meta-analysis using previous data from published studies.
Materials and methods
Search strategy
The Medline (PubMed search engine), Scopus, Web of Science and Cochrane Library database were comprehensively searched following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines to ensure a rigorous approach10. The PRISMA checklist, available in Supplementary materials (Supplementary Table 1), was utilized to facilitate the systematic review process. We have collected articles that were published up until February 27th, 2024. Two reviewers independently conducted the literature search, employing a combination of the following keywords: “osteoradionecrosis”, “mandible”, “mandibular”, “free flap”, “microvascular flap”, “free tissue” and “reconstruction” The complete search algorithm for each database can be found in the supplementary materials (Supplementary Table 2). In conjunction with the primary search, a thorough examination of the reference lists from the identified studies was conducted to identify any additional articles that may have been overlooked. The collected studies were meticulously organized and stored using the Zotero reference management software (version 6.0.18)11. We ensured the credibility of our dataset by diligently removing any duplicate references. Following the initial search, two independent investigators thoroughly examined the remaining articles. The study selection process consisted of two distinct stages. Initially, we meticulously reviewed the titles and abstracts of the articles, eliminating those that did not meet our predetermined criteria for inclusion. In the second stage, we obtained the full texts of the remaining articles and conducted a comprehensive evaluation. Any disagreements during the study selection were resolved through consensus among the team members, ensuring a consistent and unified decision-making process. By employing this systematic approach, our goal was to obtain a comprehensive and dependable collection of studies for our analysis.
Criteria for study selection and data extraction
Following our systematic and comprehensive search across multiple databases, we meticulously defined our eligibility criteria using the PECOS framework to ensure clarity and precision in our systematic review and meta-analysis focusing on the prevalence of free flap failure in mandibular osteoradionecrosis reconstruction. Our review includes:
Population (P) Adult patients suffering from mandibular osteoradionecrosis who underwent reconstruction using free flap techniques. This population was chosen to assess the efficacy of free flap reconstruction in patients affected by osteoradionecrosis.
Exposure (E) The exposure of interest for our study was the utilization of free flap surgical techniques for the reconstruction of the mandible in patients with osteoradionecrosis. This included a variety of flap types, with a specific focus on the prevalence of flap failure post-surgery.
Comparison (C) Given that our objective was to quantify the prevalence of free flap failure, a direct comparison component does not apply to our study's framework.
Outcomes (O) The main outcome of interest was the prevalence of free flap failure, which was assessed through complete flap losses as reported in the literature. Additionally, we sought to identify risk factors contributing to flap failure to inform better clinical decisions.
Study Types (S) Our inclusion criteria encompassed solely observational studies, including cohort, case–control, and cross-sectional studies.
Exclusion criteria We opted to omit certain categories of articles from consideration. These exclusions comprised case reports, case series involving fewer than five participants, review articles, randomized and non-randomized clinical trials, systematic reviews, meta-analyses, animal studies, letters to the editor, books, expert opinions, conference abstracts, studies not written in English, articles lacking an adequate follow-up period, studies involving reconstruction using pedicled flaps, studies involving patients with medication-related osteonecrosis, studies that did not specify the patients from whom the free flaps failed75,76, studies using populations with multiple pathologies requiring free flap reconstruction without specifying who received a second free flap77, and articles that did not clearly mention the failure78, studies lacking full-text accessibility and articles containing data sourced from surveillance databases. In situations where articles had overlapping populations, preference was given to the most recent or comprehensive publication for inclusion.
Data Extraction For each included study, we gathered the following information: the primary author's name, publication year, study design, continent of origin, country, study duration, number of patients, number of free flaps utilized, proportion of male participants, mean age, mean time to diagnosis (following completion of radiotherapy), and the count of free flap failures.
Quality assessment
The Quality Assessment Tools provided by the collaboration between the Universities of Newcastle, Australia, and Ottawa, Canada, were utilized by two researchers who independently conducted a meticulous evaluation of each study. The Newcastle–Ottawa Scale (NOS) and the adapted NOS for Cohort and Cross-Sectional Studies were employed, respectively. The objective of this assessment was to scrutinize each research study for potential methodological or survey implementation issues that could compromise its internal validity. The assessment involved a 'star system' in which a study was judged on three broad perspectives: the selection of the study groups, the comparability of the groups, and the ascertainment of either the exposure or outcome of interest for case–control or cohort studies (or for cross-sectional studies with the adapted tool), respectively. A study with a score ranging from 7 to 9 was considered to have low risk of bias (high quality), while a score of 4–6 indicated moderate quality, and a score of 0–3 signified high risk of bias (low quality)12 (Supplementary Figs. 1 and 2). The Joanna Briggs Institute (JBI) Critical Appraisal tools have been utilized for case-series. The outcomes of this appraisal are then instrumental in guiding the synthesis and interpretation of the study's results. Developed by the JBI and its collaborators, the JBI Critical Appraisal tools have been sanctioned by the JBI Scientific Committee after thorough peer review. This tool includes 10 distinct questions for the appraisal of case-series74.
Statistical analysis
Model Use: The statistical analysis was carried out using the RStudio software (version: 2022.12.0 + 353) provided by RStudio Team13. In this analysis, the metafor package was utilized for the meta-analysis, enabling the estimation of the pooled prevalence and its corresponding 95% confidence intervals (CI) through the implementation of the DerSimonian and Laird random-effects model14. To calculate the prevalence, the Freeman-Tukey double arcsine transformation was employed as a part of the methodology15.
Heterogeneity and Analyses To evaluate heterogeneity across studies, a visual inspection of the forest plot and the utilization of the Cochran's Q statistic and its associated p-value were conducted. The magnitude of true heterogeneity in effect sizes was quantified using the Higgins I2 statistic and its respective 95% CI. The categorization of heterogeneity levels was as follows: 0–40% (not important), 30–60% (moderate), 50–90% (substantial), and 75–100% (considerable heterogeneity). In order to identify any influential outlying effect sizes (as initially observed in the forest plot), screening for externally studentized residuals with absolute z-values greater than two was performed, along with leave-one-out diagnostics16. Given the persistent moderate level of heterogeneity in this analysis, meta-regression analyses was conducted. In the performed meta-regression analysis with continuous variables, the year of publication, the proportion of males, the mean age and the mean time to diagnosis were assessed as moderators on effect sizes. However, due to limited data availability (less than ten studies for each covariate), variables such as smoking status and other factors including duration of surgery, comorbidities, alcohol consumption, obesity, and surgeon level were not included in this analysis17. Unless otherwise specified, a significance level of p = 0.05 (two-tailed) was considered to indicate statistical significance.
Publication Bias To assess the existence of publication bias, various techniques have been developed, including examinations such as Egger's test18, Begg's test19, and the analysis of funnel plots. It is worth highlighting that the tests mentioned above were originally designed to assess data from comparative studies, assuming a bias towards publishing studies with positive outcomes over those with negative results. However, in the context of a meta-analysis focusing on proportions, there is no universally agreed-upon definition of what constitutes a positive result20. Therefore, a qualitative evaluation was conducted to examine the potential presence of publication bias in this specific meta-analysis.
Results and analysis
Search results and characteristics of the included studies
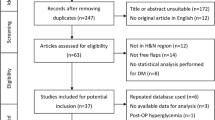
From a total of 1424 articles, forty-six eligible studies (n = 46) involving 1292 participants and 1344 free flaps were ultimately included in this analysis. The PRISMA flowchart is depicted in Fig. 1, providing a visual representation of the systematic review and meta-analysis process.The descriptive characteristics as well as the main complications of the incorporated research are presented in Table 1. All articles were published between 1994 and 2024, with research conducted from 1982 to 2022. Five of them were identified as case series, five as cohort studies, and 36 as cross-sectional studies. The majority of the studies were conducted in North America (USA and Brazil, n = 16), followed by Europe (Belgium, Norway, Italy, Sweden, The Netherlands, France, Germany, and the UK, n = 15), Asia (Japan, Taiwan, South Korea, and China, n = 12), Australia (n = 2), and South America (Brazil, n = 1). The average percent of males was 69.1% while the mean age of participants ranged from 43 to 68.5 years (median = 54.3 years). The mean time from completion of radiotherapy to diagnosis was 39.3 months. Eight of the whole number of articles were estimated as high quality (low risk of bias)22,24,27,31,40,42,51,54 and the remaining ones as moderate quality (moderate risk of bias) (Supplementary Fig. 1).
Prevalence of total free flap failure after free flap reconstruction for mORN
A random-effects model analysis yielded an initial overall total free flap failure (among 1328 free flaps) prevalence of 3.1% (95% CI 1.3–5.4%) with moderate heterogeneity I2 = 63% (95% CI 26–65%) (p < 0.001) (Fig. 2). Further exploration of the data through influence diagnostics, alongside a detailed forest plot representation of the leave-one-out analysis outcomes, are made available in the Supplementary materials (Supplementary Figs. 2 and 3). According to these analyses, none of the studies were identified as having a significant influence on the overall results.
Meta-regression analysis
The meta-regression analysis, which factored in continuous variables like the year of publication, the proportion of male participants, the mean age, and the mean time to diagnosis, ultimately revealed no statistically significant alterations, either positive or negative, as detailed in the Supplementary materials (refer to Supplementary Table 3).
Discussion
Osteoradionecrosis of the jaw is defined as an exposed, nonhealing bone over a period of three months without evidence of existing malignancy. Many staging systems have been developed throughout the years in order the affected cases to be classified and treated properly. They use parameters such as the response to the therapy (HBO), clinical findings, radiological findings or combinations of them6. During the evolution of mORN, complications such as fractures, infection and orocutaneous fistula may occur, resulting to the patient’s declined functionality. Microvascular free flap reconstruction is the treatment of choice for severe cases. Among the free flaps used for reconstruction, free fibula flap is the most common one, while other choices include iliac crest, radial forearm flap, anterolateral thigh flap and scapular flap67.
Free flap failure after reconstruction for mandibular osteoradionecrosis is influenced by a myriad of factors that pose complex challenges for healthcare providers and patients. Compromised vascularity, radiation-induced tissue damage, lengthy operative times, and patient-specific factors such as malnutrition significantly affect the outcome, leading to poor tissue healing, compromised immune response, and reduced flap viability. Conditions like coagulopathies and low skeletal muscle mass further complicate recovery, underscoring the need for tailored medical strategies and highlighting their roles as predictors of surgical complications and overall survival. Additionally, gender, prior radiation therapy, poor oral hygiene, and lack of regular follow-up visits have been associated with higher rates of implant failure and complications, emphasizing the importance of comprehensive patient care. The presence of osteoradionecrosis, infection risks, and lifestyle choices such as smoking and diabetes also critically impact the success of flap reconstructions, pointing towards a complex interplay of biological, lifestyle, and treatment-related factors that determine the long-term success of mandibular reconstructions68.
It is crucial to identify and optimize these factors preoperatively to minimize the risk of flap failure. A thorough evaluation of the patient's overall health status, including nutritional assessment and smoking cessation counseling, should be conducted to improve outcomes. To mitigate the risk of free flap failure, a multidisciplinary approach is crucial. Preoperative evaluation and optimization of patients' medical conditions, including glycemic control and smoking cessation, are vital. Proper patient selection, based on an assessment of individual risk factors, can help identify those who are more likely to benefit from free flap reconstruction. Intraoperatively, meticulous surgical technique and anastomosis are essential. Surgeons must carefully assess the recipient vessels' quality and perform the microvascular anastomosis with precision. Monitoring of flap perfusion postoperatively through clinical examination, or microvascular imaging techniques can aid in early detection of compromised vascularity and allow for prompt intervention. Close postoperative follow-up is essential to identify any signs of flap compromise or infection. Timely management of complications, such as wound dehiscence, hematoma, or infection, is crucial to salvage the flap's viability. In cases of free flap failure, alternative reconstructive options, such as local flaps or bone grafts, should be considered to restore form and function69,70,71,72.
Our study provides evidence for 3.1% (95% CI 1.3–5.4%) prevalence of total free flap failure after free flap reconstruction for mORN. To the best of our knowledge, there is only a sole meta-analysis to date related to this issue in the scientific literature. Lee et al.73, using data from 15 studies estimate a prevalence of free flap failures (among 368 free flaps) requiring revision operations at 9.8% (95% CI 9–16%) with low heterogeneity I2 = 0% (p = 0.56) between studies. Our estimation based on 46 studies is lower 3.1% (95% CI 1.3–5.4%). Potential reasons for this discrepancy could be the larger number of studies used, different inclusion/exclusion criteria, quality assessment performed and the transformation of the data used in order to calculate the prevalence. Specific transformation was required since included studies in both systematic reviews (such as the study conducted from Suh et al.52) observed zero events of total free flap failure. More studies should be conducted in order to explore the association between the aforementioned outcomes after free flap reconstruction for mORN and potential risk factors such as high dose of ionizing irradiation, pre radiotherapy surgical treatment, primary tumor site, trauma (dental extraction), smoking status, gender, age, alcohol consumption and poor dental hygiene. In conclusion, our study provides evidence for prevalence of 3.1% (95% CI 1.3–5.4%) total free flap failure after free flap reconstruction for mORN. Our findings point to several directions for future research. Therefore, both prospective and retrospective studies need to be conducted in order this issue to be fully investigated.
Study’s strengths and limitations
The robustness of this study lies in its rigorous methodology, which included a comprehensive exploration of the literature, meticulous selection of studies, specific criteria for inclusion and exclusion, thorough screening of eligibility, quality assessment, and systematic analysis of prevalence data from twenty-four studies. Nonetheless, several limitations were identified during the course of the study. It is crucial to acknowledge that, inherent to proportional meta-analysis, efforts were made to obtain as homogeneous a population as possible, despite the inherent challenges. Consequently, several assumptions had to be made. The analysis included studies even when they did not explicitly mention the definition of ORN used to identify cases. In such instances, a thorough examination of the entire manuscript was undertaken to ascertain its suitability. Moreover, this meta-analysis amalgamated results from studies employing varying reconstruction techniques, and encompassed a broad spectrum of ages, genders, and comorbidities. However, studies focused on assessing prevalence in specific populations, such as those exclusively comprising individuals with diabetes, were intentionally excluded. Additionally, only studies that explicitly defined and identified cases of free flap failure (designating as failures those instances where salvage efforts failed, leading to non-viable tissue (flap necrosis)) were considered. Notably, there was a moderate level of unexplained heterogeneity observed in relation to the prevalence of total free flap failure. The diversity of outcomes across the studies included in this meta-analysis can largely be attributed to the inherent nature of such studies. Additionally, various conceivable risk factors, including but not limited to diabetes, impaired immune response, prolonged operative duration, obesity, patient age, gender, additional surgical interventions, as well as tobacco and alcohol consumption habits, may introduce bias in the prevalence of free flap failure following mandibular reconstruction. Furthermore, the analysis faced limitations due to a lack of detailed information, making it impossible to categorize complications by free flap type. Due to the scant number of studies addressing each of these factors (fewer than ten for each) they were excluded from the meta-regression analysis. Additionally, the study's inclusion criteria were restricted to observational studies published in English, potentially skewing the evidence base and excluding comprehensive representation of studies conducted in non-English speaking countries or in locales with limited resources.
Data availability
Literature and Rstudio data are available from the corresponding author on reasonable request.
References
Owens, D., Paleri, V. & Jones, A. V. Head and neck cancer explained: An overview of management pathways. Br. Dent. J. 233(9), 721–725. https://doi.org/10.1038/s41415-022-5199-1 (2022).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 Countries. CA Cancer J. Clin. 71(3), 209–249. https://doi.org/10.3322/caac.21660 (2021).
Zehr, L. J. & Cooper, J. S. Mandible Osteoradionecrosis. [online] PubMed. (Accessed 9 January 2023) https://www.ncbi.nlm.nih.gov/books/NBK430917/?report=classic (2022)
Chieng, C. Y., Davies, A., Aziz, A., Lowe, D. & Rogers, S. N. Health related quality of life and patient concerns in patients with osteoradionecrosis. Br. J. Oral Maxillofac. Surg. 59(9), 1061–1066. https://doi.org/10.1016/j.bjoms.2021.02.011 (2021).
Md, J. B. M., Md, E. Z., Md, M. A. F. & Md, P. J. C. Overview and emerging trends in the treatment of osteoradionecrosis. Curr. Treat. Options Oncol. 22(12), 115. https://doi.org/10.1007/s11864-021-00915-3 (2021).
Chronopoulos, A., Zarra, T., Ehrenfeld, M. & Otto, S. Osteoradionecrosis of the jaws: Definition, epidemiology, staging and clinical and radiological findings. A concise review. Int. Dent. J. 68(1), 22–30. https://doi.org/10.1111/idj.12318 (2018).
Marx, R. E. Osteoradionecrosis: A new concept of its pathophysiology. J. Oral Maxillofac. Surg. 41(5), 283–288. https://doi.org/10.1016/0278-2391(83)90294-X (1983).
Kubota, H. et al. Risk factors for osteoradionecrosis of the jaw in patients with head and neck squamous cell carcinoma. Radiat. Oncol. 16(1), 1. https://doi.org/10.1186/s13014-020-01701-5 (2021).
Aarup-Kristensen, S. et al. Osteoradionecrosis of the mandible after radiotherapy for head and neck cancer: Risk factors and dose-volume correlations. Acta Oncol. 58(10), 1373–1377. https://doi.org/10.1080/0284186X.2019.1643037 (2019).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ https://doi.org/10.1136/bmj.n71 (2021).
www.zotero.org. (n.d.). Zotero | Your personal research assistant. [online] (Accessed 15 December 2022) Available at: https://www.zotero.org
A NEWCASTLE -OTTAWA QUALITY ASSESSMENT SCALE (adapted for cross sectional studies). Available at: https://cdn-links.lww.com/permalink/ejgh/a/ejgh_31_9_2019_07_18_nguyen_15743_sdc1.pdf.
RStudio Desktop. Available at: https://posit.co/download/rstudio-desktop/ (2022)
Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. https://doi.org/10.18637/jss.v036.i03 (2010).
Miller, J. J. The inverse of the Freeman – Tukey double arcsine transformation. Am. Stat. 32(4), 138–138. https://doi.org/10.1080/00031305.1978.10479283 (1978).
Viechtbauer, W. & Cheung, M.W.-L. Outlier and influence diagnostics for meta-analysis. Res. Synth. Methods 1(2), 112–125. https://doi.org/10.1002/jrsm.11 (2010).
Handbook-5-1.cochrane.org. (n.d.). 9.6.5.1 Ensure that there are adequate studies. [online] (Accessed 27 December 2022). Available at: https://handbook-5-1.cochrane.org/chapter_9/9_6_5_1_ensure_that_there_are_adequate_studies_to_justify.htm.
Egger, M., Smith, G. D., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109), 629–634. https://doi.org/10.1136/bmj.315.7109.629 (1997).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4), 1088–1101 (1994).
Barker, T. H. et al. Conducting proportional meta-analysis in different types of systematic reviews: A guide for synthesisers of evidence. BMC Med. Res. Methodol. 21(1), 189. https://doi.org/10.1186/s12874-021-01381-z (2021).
Liu, S. et al. Fibular free flap necrosis after mandibular reconstruction surgery with osteoradionecrosis: Establishment and verification of an early warning model. J. Stomatol. Oral Maxillofac. Surg. 125(3), 101730. https://doi.org/10.1016/j.jormas.2023.101730 (2024).
Van Den Heuvel, S. C. M. et al. Free vascularized flap reconstruction for osteoradionecrosis of the mandible: A 25-year retrospective cohort study. Eur. J. Plast. Surg. 46(1), 59–65. https://doi.org/10.1007/s00238-022-01980-z (2022).
Prevost, A., Poulet, V., Delanoe, F. & Lauwers, F. Merits of the free periosteal femoral condyle flap in the management of advanced mandibular osteoradionecrosis. Int. J. Oral Maxillofac. Surg. 52(2), 175–180. https://doi.org/10.1016/j.ijom.2022.05.006 (2023).
Hurrell, M. J. L. et al. Fascio-cutaneous and fascio-periosteal free flaps for treatment of intermediate stage osteoradionecrosis of the jaws. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 136(2), 128–135. https://doi.org/10.1016/j.oooo.2022.12.002 (2023).
Van Baar, G. J. C. et al. A novel treatment concept for advanced stage mandibular osteoradionecrosis combining isodose curve visualization and nerve preservation: A prospective pilot study. Front. Oncol. 11, 630123. https://doi.org/10.3389/fonc.2021.630123 (2021).
Meleca, J. B. et al. Anterolateral thigh fascia lata rescue flap: A new weapon in the battle against OSTEORADIONECROSIS. Laryngoscope 131(12), 2688–2693. https://doi.org/10.1002/lary.29709 (2021).
Brady, G. et al. Speech and swallowing outcomes following surgical resection with immediate free tissue transfer reconstruction for advanced osteoradionecrosis of the mandible following radiation treatment for head and neck cancer. Dysphagia 37(5), 1137–1141. https://doi.org/10.1007/s00455-021-10375-4 (2022).
O’Connell, J. E. et al. Outcomes of microvascular composite reconstruction for mandibular osteoradionecrosis. Br. J. Oral Maxillofac. Surg. 59(9), 1031–1035. https://doi.org/10.1016/j.bjoms.2020.11.013 (2021).
Yamashita, J. et al. Occurrence and treatment outcome of late complications after free fibula flap reconstruction for mandibular osteoradionecrosis. Cureus https://doi.org/10.7759/cureus.13833 (2021).
Jenkins, G. W. et al. Dosimetry-guided virtual surgical planning in the reconstruction of mandibular osteoradionecrosis. Br. J. Oral Maxillofac. Surg. 59(8), 947–951. https://doi.org/10.1016/j.bjoms.2021.02.010 (2021).
Jin, T. et al. Preoperative status and treatment of osteoradionecrosis of the jaw: A retrospective study of 252 cases. Br. J. Oral Maxillofac. Surg. 58(10), e276–e282. https://doi.org/10.1016/j.bjoms.2020.07.031 (2020).
Danielsson, D. et al. Quality of life after microvascular mandibular reconstruction for osteoradionecrosis—A prospective study. Head Neck 41(7), 2225–2230. https://doi.org/10.1002/hed.25681 (2019).
Haffey, T., Winters, R., Kerr, R. & Fritz, M. Mandibular rescue: Application of the ALT fascia free flap to arrest osteoradionecrosis of the mandible. Am. J. Otolaryngol. 40(6), 102262. https://doi.org/10.1016/j.amjoto.2019.07.006 (2019).
Bettoni, J. et al. The value of reconstructive surgery in the management of refractory jaw osteoradionecrosis: A single-center 10-year experience. Int. J. Oral Maxillofac. Surg. 48(11), 1398–1404. https://doi.org/10.1016/j.ijom.2019.06.007 (2019).
Rommel, N., Kesting, M. R., Rohleder, N. H., Wolff, K.-D. & Weitz, J. Surgical management of severe osteoradionecrosis of the mandibular bone by using double free flap reconstruction. J. Cranio-Maxillofac. Surg. 46(1), 148–154. https://doi.org/10.1016/j.jcms.2017.09.025 (2018).
Löfstrand, J. et al. Quality of life after free fibula flap reconstruction of segmental mandibular defects. J. Reconstr. Microsurg. 34(02), 108–120. https://doi.org/10.1055/s-0037-1606537 (2018).
Akashi, M. et al. Heterogeneity of necrotic changes between cortical and cancellous bone in mandibular osteoradionecrosis: A histopathological analysis of resection margin after segmental mandibulectomy. BioMed Res. Inte. 2017, 1–11. https://doi.org/10.1155/2017/3125842 (2017).
Barry, C. P. et al. Tailored approach to oromandibular reconstruction in patients with compromised lower limb vessels. Head Neck 39(5), 916–920. https://doi.org/10.1002/hed.24709 (2017).
Chang, E. I. & Yu, P. Prospective series of reconstruction of complex composite mandibulectomy defects with double island free fibula flap. J. Surg. Oncol. 116(2), 258–262. https://doi.org/10.1002/jso.24647 (2017).
Baron, S. et al. Fibula free flap in the treatment of mandibular osteoradionecrosis. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 133(1), 7–11. https://doi.org/10.1016/j.anorl.2015.09.010 (2016).
Kim, J.-W., Hwang, J.-H. & Ahn, K.-M. Fibular flap for mandible reconstruction in osteoradionecrosis of the jaw: Selection criteria of fibula flap. Maxillofac. Plast. Reconstr. Surg. 38(1), 46. https://doi.org/10.1186/s40902-016-0093-x (2016).
Fan, S. et al. Synchronous reconstruction of bilateral osteoradionecrosis of the mandible using a single fibular osteocutaneous flap in patients with nasopharyngeal carcinoma. Head Neck https://doi.org/10.1002/hed.24049 (2016).
Kim, M. G., Lee, S. T., Park, J. Y. & Choi, S. W. Reconstruction with fibular osteocutaneous free flap in patients with mandibular osteoradionecrosis. Maxillofac. Plast. Reconstr. Surg. 37(1), 7. https://doi.org/10.1186/s40902-015-0007-3 (2015).
Shan, X.-F. et al. Fibular free flap reconstruction for the management of advanced bilateral mandibular osteoradionecrosis. J. Craniofac. Surg. 26(2), e172–e175. https://doi.org/10.1097/SCS.0000000000001391 (2015).
Moubayed, S. P. et al. Microvascular reconstruction of segmental mandibular defects without tracheostomy. Otolaryngol. Head Neck Surg. 152(2), 250–254. https://doi.org/10.1177/0194599814556625 (2015).
Chen, S.-H. et al. Reconstruction for osteoradionecrosis of the mandible: Superiority of free iliac bone flap to fibula flap in postoperative infection and healing. Ann. Plast. Surg. 73(Supplement 1), S18–S26. https://doi.org/10.1097/SAP.0000000000000270 (2014).
Zaghi, S. et al. Changing indications for maxillomandibular reconstruction with osseous free flaps: A 17-year experience with 620 consecutive cases at UCLA and the impact of osteoradionecrosis. Laryngoscope 124(6), 1329–1335. https://doi.org/10.1002/lary.24383 (2014).
Chandarana, S. et al. Osteocutaneous free tissue transplantation for mandibular osteoradionecrosis. J. Reconstr. Microsurg. 29(01), 005–014. https://doi.org/10.1055/s-0032-1326731 (2012).
Sawhney, R. & Ducic, Y. Management of pathologic fractures of the mandible secondary to osteoradionecrosis. Otolaryngol. Head Neck Surg. 148(1), 54–58. https://doi.org/10.1177/0194599812463186 (2013).
Hoffman, G., Islam, S. & Eisenberg, R. Microvascular reconstruction of the mouth, face and jaws. Oromandibular reconstruction – free fibula flap. Aust. Dent. J. 57(3), 379–387. https://doi.org/10.1111/j.1834-7819.2012.01709.x (2012).
Baumann, D. P. et al. Free flap reconstruction of osteoradionecrosis of the mandible: A 10-year review and defect classification. Head Neck 33(6), 800–807. https://doi.org/10.1002/hed.21537 (2011).
Suh, J. D. et al. Disease relapse after segmental resection and free flap reconstruction for mandibular osteoradionecrosis. Otolaryngol. Head Neck Surg. 142(4), 586–591. https://doi.org/10.1016/j.otohns.2009.12.008 (2010).
Alam, D. S., Nuara, M. & Christian, J. Analysis of outcomes of vascularized flap reconstruction in patients with advanced mandibular osteoradionecrosis. Otolaryngol. Head Neck Surg. 141(2), 196–201. https://doi.org/10.1016/j.otohns.2009.03.013 (2009).
Hirsch, D. L., Bell, R. B., Dierks, E. J., Potter, J. K. & Potter, B. E. Analysis of microvascular free flaps for reconstruction of advanced mandibular osteoradionecrosis: A retrospective cohort study. J. Oral Maxillofac. Surg. 66(12), 2545–2556. https://doi.org/10.1016/j.joms.2007.08.041 (2008).
Curi, M. M. et al. Management of extensive osteoradionecrosis of the mandible with radical resection and immediate microvascular reconstruction. J. Oral Maxillofac. Surg. 65(3), 434–438. https://doi.org/10.1016/j.joms.2005.12.068 (2007).
Chiapasco, M. et al. Clinical outcome of dental implants placed in fibula-free flaps used for the reconstruction of maxillo-mandibular defects following ablation for tumors or osteoradionecrosis. Clin. Oral Implants Res. 17(2), 220–228. https://doi.org/10.1111/j.1600-0501.2005.01212.x (2006).
Militsakh, O. N., Wallace, D. I., Kriet, J. D., Tsue, T. T. & Girod, D. A. The role of the osteocutaneous radial forearm free flap in the treatment of mandibular osteoradionecrosis. Otolaryngol. Head Neck Surg. 133(1), 80–83. https://doi.org/10.1016/j.otohns.2005.03.018 (2005).
Gal, T. J., Yueh, B. & Futran, N. D. Influence of prior hyperbaric oxygen therapy in complications following microvascular reconstruction for advanced osteoradionecrosis. Arch. Otolaryngol. Head Neck Surg. 129(1), 72. https://doi.org/10.1001/archotol.129.1.72 (2003).
Ang, E. et al. Reconstructive options in the treatment of osteoradionecrosis of the craniomaxillofacial skeleton. Br. J. Plast. Surg. 56(2), 92–99. https://doi.org/10.1016/S0007-1226(03)00085-7 (2003).
Store, G., Boysen, M. & Skjelbred, P. Mandibular osteoradionecrosis: Reconstructive surgery. Clin. Otolaryngol. Allied Sci. 27(3), 197–203. https://doi.org/10.1046/j.1365-2273.2002.00564.x (2002).
Celik, N. et al. Osteoradionecrosis of the mandible after oromandibular cancer surgery. Plast. Reconstr. Surg. 109(6), 1875–1881. https://doi.org/10.1097/00006534-200205000-00014 (2002).
Chang, D. W., Oh, H., Robb, G. L. & Miller, M. J. Management of advanced mandibular osteoradionecrosis with free flap reconstruction. Head Neck 23(10), 830–835. https://doi.org/10.1002/hed.1121 (2001).
Shaha, A. R. et al. Resection and immediate microvascular reconstruction in the management of osteoradionecrosis of the mandible. Head Neck 19(5), 406–411. https://doi.org/10.1002/(SICI)1097-0347(199708)19:5%3c406::AID-HED7%3e3.0.CO;2-3 (1997).
Santamaria, E., Wei, F.-C. & Chen, H.-C. Fibula osteoseptocutaneous flap for reconstruction of osteoradionecrosis of the mandible. Plast. Reconstr. Surg. 101(4), 921–929. https://doi.org/10.1097/00006534-199804040-00006 (1998).
Nakatsuka, T. et al. Surgical treatment of mandibular osteoradionecrosis: Versatility of the scapular osteocutaneous flap. Scand. J. Plast. Reconstr. Surg. Hand Surg. 30(4), 291–298. https://doi.org/10.3109/02844319609056407 (1996).
Ioannides, C., Fossion, E., Boeckx, W., Hermans, B. & Jacobs, D. Surgical management of the osteoradionecrotic mandible with free vascularised composite flaps. J. Cranio-Maxillofac. Surg. 22(6), 330–334. https://doi.org/10.1016/S1010-5182(05)80113-1 (1994).
Yadav, S. K. & Shrestha, S. Microvascular free flaps in oral and maxillofacial reconstruction following cancer ablation. J. Nepal Health Res. Counc. 15(2), 88–95. https://doi.org/10.3126/jnhrc.v15i2.18157 (2017).
Sanati-Mehrizy, P. et al. Risk factors leading to free flap failure. J. Craniofac. Surg. 27(8), 1956–1964. https://doi.org/10.1097/scs.0000000000003026 (2016).
Zhou, W. et al. Risk factors for free flap failure: a retrospective analysis of 881 free flaps for head and neck defect reconstruction. Int. J. Oral Maxillofac. Surg. 46(8), 941–945. https://doi.org/10.1016/j.ijom.2017.03.023 (2017).
Daveau, C. et al. 190. Osteomyelitis following mandibular reconstruction with free fibula flap: A cohort study of an emerging and complex bone and joint infection. Open Forum Infect. Dis. 7, 223–224. https://doi.org/10.1093/ofid/ofaa439.500 (2020).
Salgado, C., Chim, H., Schoenoff, S. & Mardini, S. Postoperative care and monitoring of the reconstructed head and neck patient. Semin. Plast. Surg. 24(03), 281–287. https://doi.org/10.1055/s-0030-1263069 (2010).
Kostares, E., Kostare, G., Kostares, M. & Kantzanou, M. Prevalence of surgical site infections after open reduction and internal fixation for mandibular fractures: A systematic review and meta-analysis. Sci. Rep. 13(1), 55. https://doi.org/10.1038/s41598-023-37652-6 (2023).
Lee, M., Chin, R. Y., Eslick, G. D., Sritharan, N. & Paramaesvaran, S. Outcomes of microvascular free flap reconstruction for mandibular osteoradionecrosis: A systematic review. J. Cranio-Maxillofac. Surg. 43(10), 2026–2033. https://doi.org/10.1016/j.jcms.2015.03.006 (2015).
Moola, S., Munn, Z., Tufanaru, C., Aromataris, E., Sears, K., Sfetcu, R., Currie, M., Qureshi, R., Mattis, P., Lisy, K. and Mu, P-F. Chapter 7: Systematic reviews of etiology and risk. Joanna Briggs Institute Reviewer's Manual’, The Joanna Briggs Institute. Available from https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Case_Series2017_0.pdf. (2017).
Blumberg, J. M. et al. Mandibular reconstruction with the scapula tip free flap. Head Neck 41(7), 2353–2358. https://doi.org/10.1002/hed.25702 (2019).
Ma, H. et al. Computer-assisted versus traditional freehand technique for mandibular reconstruction with free vascularized fibular flap: A matched-pair study. J. Plast. Reconstr. Aesthet. Surg. 74(11), 3031–3039. https://doi.org/10.1016/j.bjps.2021.03.121 (2021).
Devine, C. M., Haffey, T. M., Trosman, S. & Fritz, M. A. Short-stay hospital admission after free tissue transfer for head and neck reconstruction. Laryngoscope 126(12), 2679–2683. https://doi.org/10.1002/lary.26047 (2016).
Ristow, O. et al. Osteoradionecrosis of the jaw-comparison between bone and soft tissue injury and their influence on surgical outcomes-a retrospective cohort study. Diagnostics (Basel, Switzerland) 13(3), 366. https://doi.org/10.3390/diagnostics13030366 (2023).
Acknowledgements
Open access funding was provided by Athanasios Tsakris.
Funding
Open access funding was provided by Athanasios Tsakris.
Author information
Authors and Affiliations
Contributions
E.K.: study conception and design, literature search, data analysis, quality assessment, statistical meta-analysis, interpretation of results and manuscript writing. M.K.: literature search, data analysis, interpretation of results, manuscript editing and professional opinion. G.K.: literature search, data analysis, interpretation of results and professional opinion. A.T.: manuscript editing and professional opinion. M.K.: critical revision of the manuscript and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kostares, E., Kostares, M., Kostare, G. et al. Prevalence of free flap failure in mandibular osteoradionecrosis reconstruction: a systematic review and meta-analysis. Sci Rep 14, 11087 (2024). https://doi.org/10.1038/s41598-024-61862-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-61862-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.