Abstract
Substantial progress in research on sperm cryopreservation has occurred since the twentieth century, especially focusing on improving sperm freezing procedures and optimizing semen extenders. However, the cellular biological mechanisms of sperm freezing damage are still unclear, which greatly restricts the promotion and development of sperm cryopreservation. An essential component of sperm freezing damage is the occurrence of cell death. Considering the existence of multiple types of cell death pathways, this review discusses connections between characteristics of regulated cell death (e.g., apoptosis and ferroptosis), and accidental cell death (e.g., intracellular ice crystals) with sperm freezing damage and explores possible future research directions in this field.
Similar content being viewed by others
Facts
-
The main type of cell death in sperm freezing damage remains to be determined.
-
Oxidative stress is one of the most important causes of sperm freezing damage.
-
Oxidative stress can induce various types of regulated cell death (RCD), including apoptosis and ferroptosis.
Open questions
-
Which types of RCD are driven by oxidative stress during sperm cryopreservation?
-
If multiple types of RCD appear during sperm cryopreservation, which one is most important?
-
What are the biological pathways of critical RCD?
Introduction
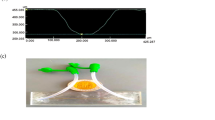
Sperm are more prone to death than other types of cells, especially during cryopreservation [1]. This is due to their highly dense chromatin, which cannot respond to changes in the microenvironment and other factors to generate genomic responses that maintain important cellular functions, such as ATP synthesis and the maintenance of redox homeostasis, and protect the integrity of the plasma membrane [2]. Cell death can be classified as accidental cell death (ACD) or regulated cell death (RCD). ACD refers to the virtually instantaneous and uncontrollable form of cell death corresponding to the physical disassembly of the plasma membrane caused by extreme physical, chemical, or mechanical cues. RCD refers to cell death that results from the activation of one or more signal transduction modules and, hence, can be pharmacologically or genetically modulated (at least kinetically to some extent) [3]. During the cryopreservation process, sperm may experience cell death caused by intracellular ice crystals, oxidative stress, and other factors, collectively referred to as sperm freezing damage [4,5,6,7]. Therefore, according to the classification of cell death types, sperm freezing damage can be divided into ACD caused by intracellular ice crystals and RCD induced by oxidative stress [1] (Fig. 1).
The occurrence of ACD due to intracellular ice crystal formation has potentially been avoided with the widespread application of glycerol. Among RCD, apoptosis is the only type that has been definitively identified in sperm cryopreservation damage, although its inductive mechanisms remain elusive. Although the term “ferroptosis” has not yet been explored in sperm cryopreservation research, it may be highly relevant to sperm freezing damage. Additionally, as oxidative stress is also associated with necroptosis, cuproptosis, and ADCD, these represent potential areas of investigation in sperm freezing damage research.
Relationship between accidental cell death and sperm freezing damage
Physical damage to the sperm plasma membrane caused by intracellular ice crystals is considered one of the main factors that contribute to the poor quality of frozen-thawed semen [1, 8,9,10,11,12]. The control of dehydration and application of osmoprotectants in sperm cryopreservation are the main measures used to delay this event (Fig. 1).
Control of dehydration
Conventional cryopreservation is the most widely used sperm cryopreservation technique and includes manual and programmable freezing. In the manual freezing technique, 0.25- or 0.5-mL plastic straws filled with extended semen are placed in contact with liquid nitrogen (LN2) vapor 4–5 cm above the LN2 for no longer than 15 min (10 min is recommended) before being immersed in LN2 for storage [11]. Programmable freezing is a method of gradually freezing/cooling sperm in two or three steps within 2 to 4 h using a programmable biofreezer [13].
The formation of intracellular ice crystals depends on the cooling rate. During the slow cooling process, sperm dehydration is controlled by the increase in osmotic pressure caused by extracellular ice crystals. Excessive dehydration can cause unexpected sperm death (osmotic damage, structural loss), called the “solution effect” [14]. In addition, extracellular ice crystals may cause physical damage to sperm [8]. A faster cooling rate can prevent sperm from dehydrating, which can lead to the formation of intracellular ice crystals, which is fatal to sperm [15]. Therefore, a suitable cooling rate is particularly important for sperm and requires a balance between the sperm dehydration rate and the formation of intracellular ice crystals during sperm freezing, which is known as the “two-factor hypothesis” [10].
Permeable cryoprotectants
For many cell types, including mammalian oocytes and embryos, the osmotic behavior of cells during freezing can be predicted from numerical models. Therefore, the probability of intracellular ice crystal formation under different linear cooling rates can be estimated [15]. This model suggests that cell freezing damage is caused by the formation of intracellular ice crystals. By combining cryomicroscopy with observation, it is possible to visualize the formation of intracellular ice crystals in oocytes and embryos subjected to different cooling rates [14]. However, experimental observations of mammalian sperm cryopreservation with glycerol are inconsistent with model prediction results [16,17,18,19,20].
The application of glycerol as a permeable cryoprotectant marks a significant advance in semen cryopreservation [21]. Similar to other permeable cryoprotectants, glycerol can undergo hydration reactions with water-based solvents, increasing the viscosity of intracellular fluids and thereby inhibiting the formation of ice crystals to a certain extent and protecting cells [22]. Morris et al. [23, 24] observed the ultrastructure of frozen human and horse semen subjected to cooling rates ranging from 0.3 to 3000 °C/min using freeze-fracture electron microscopy and freeze substitution. Intracellular ice crystals were not detected at any cooling rate, and glycerol played a major role in this process.
Regulated cell death and sperm freezing damage
However, 40–50% of sperm still die after freezing, and surviving sperm subpopulations after thawing are also affected and are unable to perform normal physiological functions [13, 25,26,27,28].
The development of sperm cryopreservation technology has significantly improved the quality of frozen semen and prevented a large proportion of sperm ACD caused by intracellular ice crystal formation [10, 21,22,23,24]. However, approximately 40–50% of sperm still experience mortality following cryopreservation. Furthermore, the surviving subpopulations of sperm demonstrate functional impairments upon thawing, compromising their ability to perform normal physiological functions [13, 25,26,27,28]. Interestingly, fresh semen (with a total motility of over 70–80%) that is considered of sufficient quality for freezing also has a mortality rate of approximately 20% after ejaculation and has significant individual [29, 30] and seasonal differences in freezability [31, 32]. In addition, the freezability of semen is not only related to the sperm itself but also to the seminal plasma [33]. These findings indicate that sperm are highly vulnerable to death, and a certain development process exists that may be accelerated by freezing. Importantly, this process can be modulated, and its characteristics do not meet the definition of ACD. Therefore, we speculate that RCD plays an important role in sperm freezing damage.
RCD regulated cell death
The first scientific observation of RCD occurred in 1842 when Karl Vogt noticed that the notochord of tadpoles disappeared during development and found that the disappearance of such cells had physiological significance during the developmental stage. When the term “apoptosis” emerged in 1972, research on RCD began to increase [34]. In the twenty-first century, multiple types of non-apoptotic RCD were discovered, such as necroptosis [35] and ferroptosis [36].
There are two distinct forms of RCD, although the underlying molecular mechanisms exhibit considerable overlap. RCD is involved in two diametrically opposed scenarios. On one hand, RCD can occur in the absence of any exogenous environmental perturbation, hence operating as a built-in effector of physiological programs for development or tissue turnover. These completely physiological forms of RCD are generally referred to as programmed cell death [3, 37, 38]. On the other hand, RCD can originate from perturbations of the intracellular or extracellular microenvironment that are too intense or prolonged for adaptative responses to cope with the stress and restore cellular homeostasis [39]. In general, cells will trigger one or more types of RCD in response to different stressors, especially oxidative stress [40].
Sperm freezing damage and oxidative stress
Oxidative stress is one of the most important causes of sperm freezing damage, resulting in damage to the structural and functional integrity of sperm. Its essence is an imbalance of intracellular oxidation-reduction reactions [41, 42]. Reactive oxygen species (ROS) are a class of highly reactive oxidative free radicals that are produced by normal physiological processes and play an important role in cell signaling and tissue homeostasis [43]. The production of ROS in mature sperm primarily occurs through two distinct pathways. One pathway involves the nicotinamide adenine dinucleotide phosphate (NADPH) oxidase system, which is located on the sperm plasma membrane. The other pathway is associated with electron leakage from the mitochondrial electron transport chain, which serves as the primary source of ROS production in sperm [8, 44,45,46]. The role played by ROS depends on their concentration in sperm; only when the concentrations are at an appropriate level can sperm exert normal physiological functions [47]. Under physiological conditions, ROS ensure the stability of chromatin and protect DNA from damage during sperm development and maturation. Additionally, ROS can activate the cAMP pathway and its downstream signaling cascade, which is important for sperm capacitation and forward movement [41, 43, 45, 46]. However, when the ROS level increases, sperm undergo oxidative stress, causing plasma membrane lipid peroxidation and mitochondrial damage. Lipid aldehydes produced by lipid peroxidation bind to proteins in the mitochondrial electron transport chain, triggering an increase in ROS in a self-perpetuating cycle and further causing DNA damage, which is referred to as “oxidative damage” [41, 43, 47,48,49].
The oxidative stress experienced by sperm during freezing can be divided into two aspects. The first aspect is the consumption of antioxidants. Sperm support their movement through a high mitochondrial metabolic rate. Due to the extreme differentiation of sperm cells, the highly dense chromatin cannot produce an antioxidant response in the genome. Additionally, during the initial support of cells, most sperm cell cytoplasm is absorbed, resulting in a lack of cytoplasmic antioxidants, including enzymes and small-molecule ROS scavengers [2]. The second aspect pertains to the disruption of the extracellular microenvironment. To accommodate changes within this microenvironment during the freezing process, including cooling and dehydration, sperm decrease their metabolic rate, thereby enhancing their chances of survival. However, during the freezing and thawing stage, as the microenvironment conditions and metabolic rate recover, ROS surge during a short period of time, and if not controlled, sperm will undergo oxidative stress and eventually die [8, 46, 50]. Oxidative damage can induce various types of RCD [3, 40, 51, 52], including apoptosis [53, 54] and ferroptosis [36, 55, 56]. Oxidative damage is not only the cause of various types of RCD, but also results from RCD.
Sperm freezing damage and apoptosis
Apoptosis is the only RCD marker of sperm freezing damage [57]. Many studies show that changes in apoptotic markers, such as activation of the caspase family, phosphatidylserine (PS) externalization, and the mitochondrial membrane potential, decrease during sperm cryopreservation [4, 25, 58,59,60,61,62,63,64] and may involve both intrinsic and extrinsic apoptotic pathways [1, 9, 57, 60, 65, 66]. These two pathways can operate independently, yet also demonstrate interconnectedness.
Apoptosis
Extrinsic apoptosis
There are two main receptors for apoptosis on the cell membrane, FAS and tumor necrosis factor (TNF)-related apoptosis-inducing ligand receptor (TRAIL-R), which are associated with the FAS-associated via death domain (FADD) [67,68,69,70]. When FAS and TRAIL-R bind to their ligands (FAS-L and TRAIL), conformational changes occur, which further lead to conformational changes in FADD. The altered conformation of FADD causes the precursor state of Caspase 8/10 to mature, and the activated Caspase 8/10 further activates Caspase 3/7 to induce apoptosis and cleave the BH3 interacting domain (Bid) death agonist to form a truncated Bid (t-Bid) [71,72,73,74].
Intrinsic apoptosis
t-Bid binds to the mitochondrial membrane, activating the BCL2-associated X (BAX) apoptosis regulator and BCL2 antagonist/killer 1 (BAK1; commonly known as BAK) located on the mitochondrial membrane [71, 72]. Bax and Bak are inhibited by pro-apoptotic and anti-apoptotic members of the BCL2 family and BCL2-like 1 (BCLXl). When Bax and Bak cannot be inhibited and are activated, they induce mitochondrial outer membrane permeabilization (MOMP) and release cytochrome C [75,76,77]. Cytochrome C binds to the precursor of Caspase 9 and apoptotic peptidase activating factor 1 to form an apoptotic body. Such apoptosomes can induce the maturation of Caspase 9 and further activate Caspase 3/7, leading to cell apoptosis [78].
Potential factors inducing apoptosis in sperm freezing damage
Although apoptosis has been confirmed to occur in sperm freezing damage, the specific regulatory mechanisms remain unclear. Notably, the activation of Caspase 3 during sperm cryopreservation is highly correlated with the degree of lipid peroxidation [79, 80]. Therefore, in this section, we discuss the potential mechanisms underlying lipid peroxidation-induced apoptosis during this stage (Fig. 2). ROS elevation induces cardiolipin peroxidation on the inner mitochondrial membrane (IMM), leading to the separation of cytochrome C and its release. The IMM also regulates MOMP through the mitochondrial permeability transition pore (mPTP), releasing cytochrome C and activating downstream cascades to complete apoptosis [81]. In addition, lipid peroxidation products regulate apoptosis by activating different signaling pathways, including the nuclear factor kappa B (NF-κB), mitogen-activated protein kinase (MAPK), and protein kinase C (PKC) signaling pathways. The NF-κB family is widely involved in inflammation, cell death, and the stress response [82]. Lipid peroxidation products can inhibit the degradation of I kappa B to maintain NF-κB activity, and NF-κB can phosphorylate the anti-apoptotic protein Bcl-2, rendering it inactive during lipid peroxidation [83, 84]. The MAPK signaling pathway is responsible for cell signaling in response to various stimuli, including oxidative stress [85]. Lipid peroxidation products can form adducts with extracellular regulated kinases, c-Jun-N-terminal kinases, and p38, which activate MAPKs, induce caspase maturation, and initiate the apoptosis process [86, 87]. The PKC signaling pathway is a key factor regulating cell signaling transduction, such as cell proliferation, differentiation, and apoptosis [88]. Lipid peroxidation products can activate PKCδ, which is further cleaved by Caspase 3 to generate a constitutively active catalytic fragment, amplifying the apoptotic cascade reaction [89].
Apoptosis is not the only evidence of RCD in sperm freezing damage
Oxidative stress is one of the most important causes of sperm freezing damage. However, in previous studies, researchers only focused on the impact of apoptosis on sperm during this period, ignoring other types of RCD. This limitation may also be one of the reasons for the slow development of sperm cryopreservation technology. Apoptosis is the only RCD marker of sperm freezing damage. However, some studies suggest that apoptosis may not be the main factor that causes death in frozen-thawed sperm.
Z-VAD-FMK (Z-VAD) is a pan-caspase irreversible inhibitor that inhibits RCD caused by the caspase family, including apoptosis [90]. Ideally, Z-VAD could markedly reduce the death indicators of frozen-thawed semen, including improved vitality and plasma membrane integrity. However, the addition of Z-VAD before freezing had no significant effect on the integrity of the plasma membrane of frozen-thawed bovine sperm, and the addition of Z-VAD after thawing had no significant effect on the viability of bovine sperm [91]. In addition, similar conclusions were drawn from the frozen semen of dogs; regardless of whether Z-VAD was added before or after freezing, sperm motility and plasma membrane integrity were not improved [92]. Annexin V/propidium iodide (PI) double staining is a commonly used method for detecting apoptosis [93] and is widely used in studies of sperm freezing damage [94]. Annexin V can bind to PS, and PI is a nucleic acid dye that only enters cells when the cell membrane is damaged. Therefore, the Annexin V/PI double staining method can label early apoptotic cells (Annexin V+, PI−) and late apoptotic cells (Annexin V+, PI+). However, when cells undergo a type of regulated necrosis other than apoptosis, only early apoptotic cells can be used as apoptotic markers. This is because when regulated necrosis occurs with loss of plasma membrane integrity, Annexin V enters the cell and binds to PS [95, 96]. Therefore, the sperm sorted by Annexin V immunomagnetic beads (Annexin V+) [97, 98] may not be entirely apoptotic. In addition, the decrease in mitochondrial membrane potential in frozen-thawed sperm may not be entirely caused by apoptosis, and necrostatin-1 can also rescue the decrease in mitochondrial membrane potential induced by oxidative stress [99]. Moreover, DNA fragmentation, as a marker of late apoptosis, does not show significant changes during sperm cryopreservation and thawing [60, 100]. It is important to clarify that, whereas lipid peroxidation may trigger sperm apoptosis, the process of apoptosis itself does not induce lipid peroxidation [55].
Sperm freezing damage and ferroptosis
The response to oxidative stress is a key pathway determining the fate of cells. Among the factors that cause oxidative stress in cells, oxidative modification of lipids in biological membranes, especially lipid peroxidation, is an important regulator of cell fate. Widespread lipid peroxidation leads to cell death through a type of RCD called “ferroptosis” [101]. Although the term “ferroptosis” has not yet been mentioned in studies of sperm freezing damage, sperm possess many prerequisites for inducing ferroptosis, and changes in some key indicators are also reported in relevant research.
Ferroptosis
Ferroptosis is a newly discovered type of RCD characterized by a lethal level of iron-dependent lipid peroxidation, which is associated with the oxidation of polyunsaturated fatty acids bound to phospholipids (PUFA-PLs) on the biological membrane [36, 55, 56]. Oxidation-reduction and iron regulation comprise the central framework of ferroptosis [55], which is independent of the caspase family and the necrosome, and manifest as a necrotic morphology [36]. The resistance of cells to ferroptosis is mainly reflected by their ability to scavenge membrane lipid peroxides. Solute carrier family 7member 11 (SLC7A11)-reduced glutathione (GSH)-glutathione peroxidase 4 (GPX4) is the main regulator of ferroptosis [55].
GPX4 is a selenoprotein that uses GSH to reduce oxidized PUFA-PLs and inhibit ferroptosis [102]; the synthesis of GSH requires the uptake of cystine by SLC7A11. Therefore, GPX4 and SLC7A11 are also major targets for inducing cell ferroptosis [36, 103, 104]. In addition, independent anti-ferroptosis mechanisms of GPX4 have been discovered in recent years. Coenzyme Q10 (CoQ10) is the second endogenous mechanism of resistance to ferroptosis and exists throughout the entire biological membrane. Reduced CoQ10 can reduce lipid peroxides through self-oxidation, and then ferroptosis suppressor protein 1 regenerates reduced CoQ10 through NADPH [105, 106]. The oxidation of PUFA-PLs is driven by the formation of hydroxyl radicals through the Fenton reaction between Fe2+ and H2O2 [107, 108], which depends on the concentration of the labile iron pool (LIP) in cells [109]. Iron regulation is the key to ferroptosis. On one hand, Fe3+ binds to transferrin and enters the cell membrane via transferrin receptor 1, subsequently being released into the cytoplasm [110,111,112,113,114,115,116]. On the other hand, ferritin bound to Fe3+ forms autophagosomes via microtubule-associated protein 1 light chain 3 (LC3) and autophagy-related proteins 5 and 7 (ATG5/7) and combines with lysosomes to form autophagosomes. Relevant enzymes degrade proteins and release Fe3+, leading to an increase in LIP concentration and LIP accumulation, which triggers ferroptosis [117].
Key evidence of ferroptosis in sperm freezing damage
The mature sperm plasma membrane is abundant in polyunsaturated fatty acids (PUFAs), which not only maintain membrane fluidity but are also susceptible to oxidation. Consequently, membrane lipid peroxidation serves as a significant indicator of sperm freezing damage and may be associated with the Fenton reaction [118,119,120,121,122] (Fig. 3). Trolox and deferoxamine (DFO) are widely used inhibitors in ferroptosis research. Trolox can reduce lipid peroxides, whereas DFO chelates free iron ions, thereby decreasing LIP levels and suppressing the Fenton reaction [123]. The addition of Trolox to diluents safeguards the quality of frozen semen from both healthy individuals and patients with oligospermia [124] and also improves the plasma membrane integrity, acrosome integrity, and mitochondrial membrane potential of thawed rabbit semen [125]. Trolox also provides greater structural integrity (plasma membrane and mitochondria) and motility to frozen-stored ram spermatozoa [126]. In studies involving the induction of sperm oxidation models, DFO has been able to rescue sperm motility and reduce lipid peroxidation levels [127]. When Trolox and DFO are administered simultaneously, sperm motility parameters that are reduced during oxidative stress are significantly improved by up to 20% [128]. Additionally, α-lipoic acid (ALA) is an antioxidant widely used in sperm diluents that enhances the quality of thawed semen in humans [129, 130] and goats [131]. Interestingly, ALA is also considered a ferroptosis inhibitor, inhibiting ferroptosis by scavenging free radicals and chelating free iron ions [132, 133].
The redox and iron regulatory pathways of ferroptosis play crucial roles in the process of sperm cryopreservation (Fig. 3). The reduction of membrane lipid peroxides by GPX4 utilizing GSH is essential for thawed sperm survival [134]. The expression level of GPX4 in fresh semen can predict the quality of frozen sperm [135], and GSH content decreases during sperm freezing [136]. The synthesis of GSH in spermatozoa relies on the transport of cystine by SLC7A11 rather than the transsulfuration pathway [137]. Therefore, in addition to adding GSH to the diluent, the supplementation of cystine and cysteine can also significantly improve the quality of cryopreserved semen [137,138,139,140,141]. The beneficial effects of CoQ10 on sperm cryopreservation have been widely validated, particularly by a recent study demonstrating that thawed human spermatozoa exhibit a significant increase in necrotic cells that were rescued by exogenous CoQ10 addition [142]. Sun et al. [143] conducted a proteomic analysis of spermatozoa from dairy goats with different freezability and found that differentially expressed proteins were enriched in the ferroptosis pathway. Interestingly, ferritin expression was lower in the high-freezability group than in the low-freezability group. It is possible that when spermatozoa are exposed to oxidative stress, Prominin2 promotes the loading of ferritin into multivesicular bodies and its subsequent extracellular release via exosomes, serving as a mechanism driving cellular resistance to ferroptosis and avoiding severe ferroptosis levels [144].
Interestingly, research shows that dead sperm can be harmful to live sperm [1, 145, 146]. Therefore, sperm freezing damage may include the transmission of death from dead sperm in addition to environmental factors [146]. Obviously, this transmissible death is a type of RCD, but transmissibility is not a general characteristic of apoptosis [147,148,149,150,151,152], as it can only occur under certain circumstances [152,153,154]. In a model of cysteine starvation and SLC7A11 inhibition-induced ferroptosis, somatic and cancer cells exhibited comparable levels of ferroptosis propagation capacity [147], which adds weight to the importance of ferroptosis in sperm freezing damage.
Sperm freezing damage and other types of RCD
Current research on sperm freezing damage is still limited, and the underlying mechanisms remain to be elucidated. Given that oxidative stress is associated with various types of RCD in addition to apoptosis and ferroptosis, necroptosis, cuproptosis, and autophagy-dependent cell death (ACCD) may also be potential areas of investigation (Fig. 4).
Sperm freezing damage and necroptosis
Necroptosis is a type of regulated necrosis characterized by obvious necrosis morphology, including cell swelling, plasma membrane rupture, and spillover of intracellular components [3]. Activation of necroptosis is associated with receptor-interacting serine/threonine kinase 1 and 3 (R1PK1/3) and mixed lineage kinase domain-like pseudokinase (MLKL) [155,156,157,158,159]. Similar to apoptosis, necroptosis can also induce cell death by detecting disturbances in the intracellular and extracellular microenvironment through FAS and TRAIL-R [160, 161]. In in vitro experiments, low concentrations of H2O2 usually induce apoptosis. However, as the concentration of H2O2 increases, RCD shifts from apoptosis to necroptosis [162]. Considering the surge of ROS during sperm cryopreservation, we speculate that necroptosis is correlated with sperm freezing damage, but there is currently no relevant research to verify this speculation.
Caspase 8 serves as a switch between apoptosis and necroptosis. When Caspase 8 is activated, it inhibits the phosphorylation of RIPK1 and RIPK3, leading to apoptosis. However, when Caspase 8 is inactivated, RIPK1 and RIPK3 mutually activate their phosphorylation and subsequently activate downstream MLKL, triggering necroptosis [155, 156, 158, 163, 164]. Therefore, the inability of Z-VAD to rescue increased numbers of frozen-injured sperm may not be a dose-dependent problem [91] but may be due to the amplification of necroptotic signaling while inhibiting apoptosis [165, 166]. Moreover, sperms, as a type of highly metabolizing cell, produce a large amount of ROS in mitochondria, which is necessary for necroptosis [167]. Although there is currently no research on the effect of necroptosis on sperm freezing damage, necroptosis occurs in sperm in some male reproductive diseases. For example, varicocele, which causes male infertility, seriously affects semen quality, and the expression of RIPK1 and RIPK3 in the sperm of varicocele patients was significantly increased compared to a control group [168]. In addition, necrostatin-1 significantly improved the cryopreservation quality of spermatogonial stem cells [169], indicating that male germ cells are prone to necrotic apoptosis during cryopreservation.
Sperm freezing damage and cuproptosis
Similar to iron, copper ions play a crucial role as an integral component of cells and tissues in the male reproductive system. In relatively small quantities, copper serves as an essential cofactor for numerous biologically active molecules. However, its excessive accumulation can lead to metabolic disturbances, potentially compromising male fertility [170]. Cuproptosis, a type of cell death defined in 2022, primarily relies on the intracellular accumulation of copper ions. These ions directly bind to lipidated proteins involved in the tricarboxylic acid (TCA) cycle, resulting in their aggregation and dysfunction, which in turn disrupts the TCA cycle and triggers protein toxic stress, ultimately leading to cell death [171].
Certain studies on human sperm demonstrate a negative correlation between copper content in seminal plasma and sperm motility parameters [172, 173]. Knazicka et al. [174] point out that high doses of Cu2+ have a negative impact on the motility and mitochondrial activity of bull sperm. Roychoudhury et al. [175] also show that excessive copper sulfate inhibits the motility and membrane integrity of rabbit sperm, altering sperm morphology. Similarly, Rebrelo et al. [176] observed similar results in human sperm exposed to Cu2+ concentrations of 100 μg/mL. However, the occurrence of cuproptosis during sperm cryopreservation remains elusive. The degree of lipid peroxidation in sperm exhibits a dose-dependent relationship with copper ion levels [177], which is evidently associated with ferroptosis, suggesting two potential pathways. On one hand, copper ions can generate hydroxyl radicals through the Fenton reaction, driving lipid peroxidation [178]. On the other hand, copper ions can induce autophagic degradation of GPX4 to trigger ferroptosis [179]. Crucially, whether copper ion overload occurs in sperm freezing damage remains to be determined.
Sperm freezing damage and autophagy-dependent cell death
Autophagy is a catabolic process that degrades cytoplasmic substances through lysosomes, often serving as a cellular response mechanism to stress, particularly oxidative stress [180]. Autophagy is regarded as a double-edged sword, capable of protecting cell survival by eliminating damaged organelles yet also potentially leading to cell death [181]. The role of autophagy in cell death can be categorized into two types: 1) ACCD, which relies on autophagic mechanisms and manifests as unrestricted degradation of cellular contents leading to cell disruption, belonging to RCD; and 2) autophagy-mediated cell death (AMCD), which depends on other types of RCD and serves as a foundation for initiating other types of RCD [3, 182].
LC3 is a crucial component of the autophagy pathway. Upon autophagy activation, LC3-I is lipidated and converted into LC3-II. The ratio of LC3-II/LC3-I is widely used as a marker of autophagy activation [181]. Under environmental stress conditions such as incubation with H2O2, cooling at 4 °C, and the freeze-thaw process, the ratio of LC3-II/LC3-I in sperm is upregulated, indicating the activation of autophagy [183]. Interestingly, autophagy plays different roles under different oxidative stress conditions. Blocking autophagy in sperm exposed to H2O2 leads to deterioration in sperm quality and metabolic parameters, as well as an increase in cell death markers [184]. On the other hand, the use of autophagy inhibitors such as chloroquine and 3-AM significantly improves the survival rate of sperm stored at 4 °C for 96 hours and cryopreserved in liquid nitrogen [183]. It is evident that maintaining normal autophagy flux is crucial for sperm survival, and both autophagy deficiency and excessive autophagy can lead to sperm death. To attribute cell death to ADCD, the following criteria must be met: 1) there must be an elevation of autophagic flux during the cell death process; 2) the cell death process must be reversible through genetic or pharmacological inhibition of autophagy; 3) the death process must depend on at least two autophagy-related molecules, thereby excluding the possibility of individual molecules mediating cell death independently of autophagy; and 4) the death process must not be accompanied by other forms of cell death [182]. The elevation of autophagic flux and the rescue effect of inhibitors suggest that ADCD occurs in sperm freezing damage. However, CoQ10 can also rescue autophagy-mediated necrotic cells in human thawed sperm [142]. Therefore, the relationship between ADCD and sperm freezing damage requires further elucidation, particularly in distinguishing ADCD from AMCD during this process.
Crosstalk between different types of RCD in sperm freezing damage
RCD is a major therapeutic target for various human diseases. However, the therapeutic results of inhibiting the initiation of a single RCD signal are sometimes unsatisfactory, which may be related to the highly interconnected nature of signaling modules of different types of RCD in addition to factors such as drug delivery and dose effects [3, 185,186,187,188]. Therefore, in the study of sperm freezing damage, it is not only necessary to distinguish which RCD is the primary one but also to clarify the crosstalk between different RCDs to maximize the quality of thawed sperm. Lipid peroxidation not only acts as an executor of ferroptosis but also induces apoptosis through its downstream products. The overloading of copper ions can induce both cuproptosis and ferroptosis. Necroptosis and apoptosis share a common upstream activation pathway, with Caspase 8 serving as a switch between pathways. Necroptosis can increase the intracellular ROS level, which can lead to lipid peroxidation and increase the risk of triggering ferroptosis. In addition, the connection between different types of RCD includes Ca2+ levels and autophagy.
Relationship between Ca2+ and various types of RCD
Intracellular Ca2+ homeostasis plays a crucial role in sperm, ensuring their normal physiological state and fertilization capability by regulating physiological functions closely related to sperm quality and male fertility potential, such as motility, fertilization, and the entire reproductive process. Besides massive cell death, the presence of a certain proportion of sperm in hyperactivated or acrosome-reacted states within thawed sperm is also a hallmark of sperm freezing damage. Although these states are necessary for sperm during the entire fertilization process, their premature occurrence can deplete energy and acrosomal enzymes, rendering sperm unable to effectively perform their tasks during fertilization and leading to fertilization failure. Such alterations in physiological state depend on the sperm’s ability to uptake extracellular Ca2+. Therefore, both depleting Ca2+ from the culture medium and adding the Ca2+ chelator EGTA to the thawing solution can enhance the fertilization capacity of thawed sperm [189, 190]. Within the female reproductive tract, the intracellular Ca2+ flux in sperm is tightly regulated by CatSper. An increase in intracellular Ca2+ flux, mediated by CatSper, can induce sperm hyperactivation, acrosome reaction, oocyte chemotaxis, and zona pellucida penetration during the fertilization process [191]. However, the expression of CatSper is reduced during sperm cryopreservation [192, 193], suggesting that the elevation of Ca2+ flux in cryopreserved sperm is independent of CatSper. Intriguingly, this may be associated with the development of some types of RCD.
Elevated Ca2+ influx resulting in morphological changes such as osmotic stress and cell rupture is a hallmark event in regulated necrosis, including necroptosis and ferroptosis [3]. MLKL forms a homotrimer through its amino-terminal coiled-coil domain, localizes to the cytoplasmic membrane during TNF-induced necroptosis, and activates downstream TRPM7 to mediate Ca2+ influx [194]. Similar to necroptosis, the increase in Ca2+ flux in cells undergoing ferroptosis precedes cell rupture, which is associated with the formation of nanoscale pores on the plasma membrane; however, the molecular mechanism underlying the formation of these pores remains unclear [147, 195, 196]. Recent studies show that treatment of sperm with different concentrations of the SLC7A11 inhibitor sulfasalazine (SS) significantly affects their motility [137]; in fresh horse sperm, low concentrations of SS enhance motility, exhibiting a phenomenon similar to hyperactivation, whereas high concentrations lead to decreased motility. However, for cryopreserved sperm, motility is reduced regardless of inhibitor concentration. Therefore, some phenotypic changes in cryopreserved sperm resemble the development of regulated necrosis, progressing from normal sperm to viable sperm with elevated intracellular Ca2+ flux without rupturing (undergoing hyperactivation, acrosome reaction, etc.) to dead sperm. Interestingly, intracellular Ca2+ overload can trigger endogenous apoptosis, potentially related to the mitochondria. Pretreatment of sperm with Ru360 to block Ca2+ entry into mitochondria reduces Caspase 3 activation and phosphatidylserine externalization induced by H2O2 stimulation [197]. Similarly, FAS-driven exogenous apoptosis is also associated with an increase in cytosolic Ca2+ [198,199,200].
Relationship between AMCD and various types of RCD
Autophagy determines the cellular fate of sperm under various environmental stresses. Exploring how autophagy induces other types of RCD and serves as a switch between different RCDs is crucial for understanding sperm freezing damage. The relationship between autophagy and apoptosis in sperm cryopreservation remains unclear. One possibility is that autophagy suppresses apoptosis, as activation of autophagy can enhance sperm motility, reduce the expression of mitochondrial outer membrane translocase TOMM20 and PINK1, and inhibit the activation of Caspase 3 and 7, thus reducing apoptosis and promoting cell survival [201]. Another possibility is that autophagy promotes apoptosis, which is a crucial step in the process of cell death, occurring mainly through two orderly mechanisms. First, autophagy directly induces cell death by phagocytosing apoptotic molecules or organelles such as mitochondria. In this process, specific autophagy-related proteins, like Fas-associated phosphatase 1 (Fap-1) and ATG5, interact with molecules in the apoptotic signaling pathway to regulate the initiation and execution of apoptosis. For instance, the degradation of Fap-1 enhances the activity of the Fas receptor, thereby promoting the transmission of apoptotic signals [202]; additionally, truncated fragments of ATG5 can directly act on mitochondria, driving the apoptotic process by disrupting mitochondrial function [203]. Second, autophagy molecules like ATG12 interfere with cellular survival mechanisms by directly binding to apoptotic molecules, thus triggering apoptosis [204]. This direct interaction impairs the function of anti-apoptotic proteins such as Bcl-2 and Mcl-1, relieving their inhibitory effect on apoptosis. This mechanism further intensifies the apoptotic tendency of cells, ensuring the smooth execution of the apoptotic program.
In necroptosis, the assembly and activation of the necrosome are crucial, with its core consisting of RIPK1, RIPK3, and MLKL. Autophagy machinery not only serves as a scaffold for the necrosome but also indirectly promotes the progression of necroptosis by degrading the apoptotic inhibitors c-IAP1 and c-IAP2 [205]. As sperm require a significant amount of energy to maintain their motility, sperm viability is generally positively correlated with ATP levels. Interestingly, autophagy can function as a switch between apoptosis and necroptosis, similar to Caspase 8, and this depends on the intracellular ATP content. When ATP reserves decrease, autophagy tends to trigger necroptosis, whereas when ATP is sufficient, autophagy may promote apoptosis [206, 207]. Additionally, autophagosome membranes and their associated proteins, such as p62, are also involved in this switching mechanism, regulating the localization and activity of molecules related to apoptosis and necroptosis and thereby facilitating the transition between different cell death modes [208].
Mitophagy may serve as one of the primary pathways for AMCD during sperm cryopreservation. Mitochondria, the primary source of energy for sperm, play a crucial role in maintaining sperm function through their quality control. Mitophagy, as an important means of quality control, is closely associated with sperm oxidative damage [209]. On one hand, mitophagy helps maintain mitochondrial homeostasis in sperm during cryopreservation, thereby suppressing apoptosis [201]. On the other hand, mitophagy may disrupt mitochondrial energy production, leading to the generation of excessive ROS in sperm during H2O2 incubation and the freeze-thaw process, which can then induce apoptosis and necrosis—the latter which can be rescued by CoQ10 [142]. Although the role of mitochondria in ferroptosis remains controversial, mitophagy may play a pivotal role in ferroptosis induction [210]. For instance, mitochondrial autophagy effectors such as PINK1 and DRP1 positively regulate ferroptosis [211]. However, the specific mechanisms underlying how mitochondrial autophagy affects the duration and intensity of lipid peroxidation in ferroptosis require further investigation. Additionally, mitochondrial fusion mediated by the fusion proteins MFN1 and MFN2 can also promote kinase-induced ferroptosis in certain situations [212], further highlighting the complexity of the interaction between mitochondrial autophagy and ferroptosis. In many cases, the occurrence of ferroptosis is highly dependent on autophagy mechanisms, including ferritinophagy, mitochondrial autophagy, and lipophagy. This type of ferroptosis is referred to as autophagy-dependent ferroptosis [213].
Concluding remarks
The essence of sperm freezing damage is sperm death. This review summarizes the types of cell death that may occur after sperm freezing damage and analyzes the correlation between sperm freezing damage and ACD and RCD based on their characteristics. Overall, understanding the role of each type of RCD in sperm freezing damage may be the key to improving the quality of thawed semen. This review provides a feasible direction for future research on frozen semen.
References
Roca J, Parrilla I, Gil MA, Cuello C, Martinez EA, Rodriguez-Martinez H. Non-viable sperm in the ejaculate: lethal escorts for contemporary viable sperm. Anim Reprod Sci. 2016;169:24–31.
Teves ME, Roldan ERS. Sperm bauplan and function and underlying processes of sperm formation and selection. Physiol Rev. 2022;102:7–60.
Galluzzi L, Vitale I, Aaronson SA, Abrams JM, Adam D, Agostinis P, et al. Molecular mechanisms of cell death: recommendations of the Nomenclature Committee on Cell Death 2018. Cell Death Differ. 2018;25:486–541.
Upadhyay VR, Ramesh V, Dewry RK, Kumar G, Raval K, Patoliya P. Implications of cryopreservation on structural and functional attributes of bovine spermatozoa: an overview. Andrologia. 2021;53:e14154.
Peris-Frau P, Soler AJ, Iniesta-Cuerda M, Martín-Maestro A, Sánchez-Ajofrín I, Medina-Chávez DA, et al. Sperm cryodamage in ruminants: Understanding the molecular changes induced by the cryopreservation process to optimize sperm quality. Int J Mol Sci. 2020;21:2781.
Hezavehei M, Sharafi M, Kouchesfahani HM, Henkel R, Agarwal A, Esmaeili V, et al. Sperm cryopreservation: a review on current molecular cryobiology and advanced approaches. Reprod Biomed Online. 2018;37:327–39.
Lv C, Wu G, Hong Q, Quan G. Spermatozoa cryopreservation: state of art and future in small ruminants. Biopreserv Biobank. 2019;17:171–82.
Kumar A, Prasad JK, Srivastava N, Ghosh SK. Strategies to minimize various stress-related freeze-thaw damages during conventional cryopreservation of mammalian spermatozoa. Biopreserv Biobank. 2019;17:603–12.
Sieme H, Oldenhof H, Wolkers W. Sperm membrane behaviour during cooling and cryopreservation. Reprod Dom Anim. 2015;50:20–26.
Mazur P, Leibo SP, Chu EHY. A two-factor hypothesis of freezing injury: evidence from Chinese hamster tissue-culture cells. Exp Cell Res. 1972;71:345–55.
Roussel JD, Kellgren HC, Patrick TE. Bovine semen frozen in liquid nitrogen vapor. J Dairy Sci. 1964;47:1403–6.
Yeste M. Sperm cryopreservation update: Cryodamage, markers, and factors affecting the sperm freezability in pigs. Theriogenology. 2016;85:47–64.
Barbas JP, Mascarenhas RD. Cryopreservation of domestic animal sperm cells. Cell Tissue Bank. 2009;10:49–62.
Mazur P. Principles of cryobiology. In: Life in the frozen state. Boca Raton, Florida, United States: CRC Press; 2004.
Mazur P. Kinetics of water loss from cells at subzero temperatures and the likelihood of intracellular freezing. J Gen Physiol. 1963;47:347–69.
Curry MR, Millar JD, Watson PF. Calculated optimal cooling rates for ram and human sperm cryopreservation fail to conform with empirical observations. Biol Reprod. 1994;51:1014–21.
Gilmore JA. Cryoprotective agent and temperature effects on human sperm membrane permeabilities: convergence of theoretical and empirical approaches for optimal cryopreservation methods. Hum Reprod. 2000;15:335–43.
Noiles EE, Mazur P, Watson PF, Kleinhans FW, Critser JK. Determination of water permeability coefficient for human spermatozoa and its activation energy. Biol Reprod. 1993;48:99–109.
Mazur P, Koshimoto C. Is intracellular ice formation the cause of death of mouse sperm frozen at high cooling rates? Biol Reprod. 2002;66:1485–90.
Devireddy RV. The effect of extracellular ice and cryoprotective agents on the water permeability parameters of human sperm plasma membrane during freezing. Hum Reprod. 2000;15:1125–35.
Polge C, Smith AU, Parkes AS. Revival of spermatozoa after vitrification and dehydration at low temperatures. Nature. 1949;164:666–666.
Holt WV. Basic aspects of frozen storage of semen. Anim Reprod Sci. 2000;62:3–22.
Morris GJ, Faszer K, Green JE, Draper D, Grout BWW, Fonseca F. Rapidly cooled horse spermatozoa: loss of viability is due to osmotic imbalance during thawing, not intracellular ice formation. Theriogenology. 2007;68:804–12.
Morris GJ. Rapidly cooled human sperm: no evidence of intracellular ice formation. Hum Reprod. 2006;21:2075–83.
Medeiros CMO, Forell F, Oliveira ATD, Rodrigues JL. Current status of sperm cryopreservation: why isn’t it better? Theriogenology. 2002;57:327–44.
Menchaca A, Rubianes E. New treatments associated with timed artificial insemination in small ruminants. Reprod Fertil Dev. 2004;16:403–13.
Gillan L, Maxwell WMC, Evans G. Preservation and evaluation of semen for artificial insemination. Reprod Fertil Dev. 2004;16:447–54.
Watson PF. The causes of reduced fertility with cryopreserved semen. Anim Reprod Sci. 2000;60–61:481–92.
Menezes TDA, Bustamante‐Filho IC, Paschoal AFL, Dalberto PF, Bizarro CV, Bernardi ML, et al. Differential seminal plasma proteome signatures of boars with high and low resistance to hypothermic semen preservation at 5 °C. Andrology. 2020;8:1907–22.
Xu B, Wang R, Wang Z, Liu H, Wang Z, Zhang W, et al. Evaluation of lipidomic change in goat sperm after cryopreservation. Front Vet Sci. 2022;9.
Zarazaga LA, Guzmán JL, Domínguez C, Pérez MC, Prieto R. Effect of plane of nutrition on seasonality of reproduction in Spanish Payoya goats. Anim Reprod Sci. 2005;87:253–67.
Zarazaga LA, Gatica MC, Delgado-Pertíñez M, Hernández H, Guzmán JL, Delgadillo JA. Photoperiod-Treatment in mediterranean bucks can improve the reproductive performance of the male effect depending on the extent of their seasonality. Animals. 2021;11:400.
Moreira SSJ, Lago AEdeA, Moura AAA, Silva AR. Impact of seminal plasma composition on sperm freezability in wild mammals: a review. Biopreserv Biobank. 2022;20:90–96.
Kerr JFR, Wyllie AH, Currie AR. Apoptosis: a basic biological phenomenon with wideranging implications in tissue kinetics. Br J Cancer. 1972;26:239–57.
Degterev A, Huang Z, Boyce M, Li Y, Jagtap P, Mizushima N, et al. Chemical inhibitor of nonapoptotic cell death with therapeutic potential for ischemic brain injury. Nat Chem Biol. 2005;1:112–9.
Dixon SJ, Lemberg KM, Lamprecht MR, Skouta R, Zaitsev EM, Gleason CE, et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell. 2012;149:1060–72.
Conradt B. Genetic control of programmed cell death during animal development. Annu Rev Genet. 2009;43:493–523.
Fuchs Y, Steller H. Programmed cell death in animal development and disease. Cell. 2011;147:742–58.
Galluzzi L, Bravo-San Pedro JM, Kepp O, Kroemer G. Regulated cell death and adaptive stress responses. Cell Mol Life Sci. 2016;73:2405–10.
Tang D, Kang R, Berghe TV, Vandenabeele P, Kroemer G. The molecular machinery of regulated cell death. Cell Res. 2019;29:347–64.
Aitken RJ. Reactive oxygen species as mediators of sperm capacitation and pathological damage. Mol Reprod Dev. 2017;84:1039–52.
Aitken RJ, Baker MA. Oxidative stress, sperm survival and fertility control. Mol Cell Endocrinol. 2006;250:66–69.
Aitken RJ, Buckingham DW, West KM. Reactive oxygen species and human spermatozoa: analysis of the cellular mechanisms involved in luminol- and lucigenin-dependent chemiluminescence. J Cell Physiol. 1992;151:466–77.
Tosic J, Walton A. Formation of hydrogen peroxide by spermatozoa and its inhibitory effect on respiration. Nature. 1946;158:485–485.
Bisht S, Faiq M, Tolahunase M, Dada R. Oxidative stress and male infertility. Nat Rev Urol. 2017;14:470–85.
Guérin P, El Mouatassim S, Ménézo Y. Oxidative stress and protection against reactive oxygen species in the pre-implantation embryo and its surroundings. Hum Reprod Update. 2001;7:175–89.
Aitken RJ, Curry BJ. Redox regulation of human sperm function: from the physiological control of sperm capacitation to the etiology of infertility and DNA damage in the germ line. Antioxid Redox Signal. 2011;14:367–81.
De Iuliis GN, Thomson LK, Mitchell LA, Finnie JM, Koppers AJ, Hedges A, et al. DNA damage in human spermatozoa is highly correlated with the efficiency of chromatin remodeling and the formation of 8-Hydroxy-2′-Deoxyguanosine, a marker of oxidative stress. Biol Reprod. 2009;81:517–24.
Thomson LK, Fleming SD, Aitken RJ, De Iuliis GN, Zieschang J-A, Clark AM. Cryopreservation-induced human sperm DNA damage is predominantly mediated by oxidative stress rather than apoptosis. Hum Reprod. 2009;24:2061–70.
Du Plessis SS, Makker K, Desai NR, Agarwal A. Impact of oxidative stress on IVF. Expert Rev Obstet Gynecol. 2008;3:539–54.
Su LJ, Zhang JH, Gomez H, Murugan R, Hong X, Xu D, et al. Reactive oxygen species-induced lipid peroxidation in apoptosis, autophagy, and ferroptosis. Oxid Med Cell Longev. 2019;2019:1–13.
Dionísio PA, Amaral JD, Rodrigues CMP. Oxidative stress and regulated cell death in Parkinson’s disease. Ageing Res Rev. 2021;67:101263.
Sinha K, Das J, Pal PB, Sil PC. Oxidative stress: the mitochondria-dependent and mitochondria-independent pathways of apoptosis. Arch Toxicol. 2013;87:1157–80.
Clutton S. The importance of oxidative stress in apoptosis. Br Med Bull. 1997;53:662–8.
Stockwell BR. Ferroptosis turns 10: emerging mechanisms, physiological functions, and therapeutic applications. Cell. 2022;185:2401–21.
Stockwell BR, Friedmann Angeli JP, Bayir H, Bush AI, Conrad M, Dixon SJ, et al. Ferroptosis: a regulated cell death nexus linking metabolism, redox biology, and disease. Cell. 2017;171:273–85.
Martin G, Sabido O, Durand P, Levy R. Cryopreservation Induces an Apoptosis-Like Mechanism in Bull Sperm. Biol Reprod. 2004;71:28–37.
Zeng C, Peng W, Ding L, He L, Zhang Y, Fang D, et al. A preliminary study on epigenetic changes during boar spermatozoa cryopreservation. Cryobiology. 2014;69:119–27.
Peña FJ, Johannisson A, Wallgren M, Rodrı́guez-Martı́nez H. Assessment of fresh and frozen–thawed boar semen using an Annexin-V assay: a new method of evaluating sperm membrane integrity. Theriogenology. 2003;60:677–89.
Paasch U, Sharma RK, Gupta AK, Grunewald S, Mascha EJ, Thomas AJ Jr, et al. Cryopreservation and thawing is associated with varying extent of activation of apoptotic machinery in subsets of ejaculated human spermatozoa. Biol Reprod. 2004;71:1828–37.
Duru NK, Morshedi M, Schuffner A, Oehninger S. Cryopreservation-thawing of fractionated human spermatozoa and plasma membrane translocation of phosphatidylserine. Fertil Steril. 2001;75:263–8.
Di Santo M, Tarozzi N, Nadalini M, Borini A. Human sperm cryopreservation: update on techniques, effect on DNA integrity, and implications for ART. Adv Urol. 2011;2012:e854837.
Said TM, Gaglani A, Agarwal A. Implication of apoptosis in sperm cryoinjury. Reprod Biomed Online. 2010;21:456–62.
Anzar M, He L, Buhr MM, Kroetsch TG, Pauls KP. Sperm apoptosis in fresh and cryopreserved bull semen detected by flow cytometry and its relationship with fertility. Biol Reprod. 2002;66:354–60.
Paasch U, Grunewald S, Agarwal A, Glandera HJ. Activation pattern of caspases in human spermatozoa. Fertil Steril. 2004;81:802–9.
Asadi A, Ghahremani R, Abdolmaleki A, Rajaei F. Role of sperm apoptosis and oxidative stress in male infertility: a narrative review. Int J Reprod Biomed. 2021;19:493–504.
Karstedt S, Montinaro A, Walczak H. Exploring the TRAILs less travelled: TRAIL in cancer biology and therapy. Nat Rev Cancer. 2017;17:352–66.
Wajant H. The Fas signaling pathway: more than a paradigm. Science. 2002;296:1635–6.
Fleten KG, Flørenes VA, Prasmickaite L, Hill O, Sykora J, Mælandsmo GM, et al. hvTRA, a novel TRAIL receptor agonist, induces apoptosis and sustained growth retardation in melanoma. Cell Death Discov. 2016;2:1–11.
Aggarwal BB, Gupta SC, Kim JH. Historical perspectives on tumor necrosis factor and its superfamily: 25 years later, a golden journey. Blood. 2012;119:651–65.
Gross A, Yin X-M, Wang K, Wei MC, Jockel J, Milliman C, et al. Caspase cleaved BID targets mitochondria and is required for cytochrome c release, while BCL-XL prevents this release but not tumor necrosis factor-R1/Fas death. J Biol Chem. 1999;274:1156–63.
Huang K, Zhang J, O’Neill KL, Gurumurthy CB, Quadros RM, Tu Y, et al. Cleavage by Caspase 8 and mitochondrial membrane association activate the BH3-only protein bid during TRAIL-induced apoptosis. J Biol Chem. 2016;291:11843–51.
Fu Q, Fu TM, Cruz AC, Sengupta P, Thomas SK, Wang S, et al. Structural basis and functional role of intramembrane trimerization of the Fas/CD95 death receptor. Mol Cell. 2016;61:602–13.
Scott FL, Stec B, Pop C, Dobaczewska MK, Lee JJ, Monosov E, et al. The Fas–FADD death domain complex structure unravels signalling by receptor clustering. Nature. 2009;457:1019–22.
Tait SWG, Green DR. Mitochondria and cell death: outer membrane permeabilization and beyond. Nat Rev Mol Cell Biol. 2010;11:621–32.
Delbridge ARD, Grabow S, Strasser A, Vaux DL. Thirty years of BCL-2: translating cell death discoveries into novel cancer therapies. Nat Rev Cancer. 2016;16:99–109.
Luna-Vargas MPA, Chipuk JE. Physiological and pharmacological control of BAK, BAX, and beyond. Trends Cell Biol. 2016;26:906–17.
Li P, Nijhawan D, Budihardjo I, Srinivasula SM, Ahmad M, Alnemri ES, et al. Cytochrome c and dATP-dependent formation of Apaf-1/Caspase-9 complex initiates an apoptotic protease cascade. Cell. 1997;91:479–89.
Ferrusola CO, Fernández LG, Morrell JM, Sandoval CS, García BM, Rodríguez-Martinez H, et al. Lipid peroxidation, assessed with BODIPY-C11, increases after cryopreservation of stallion spermatozoa, is stallion-dependent and is related to apoptotic-like changes. Reproduction. 2009;138:55–63.
MartinMuñoz P, Ferrusola CO, Vizuete G, Dávila MP, Martinez HR, Peña FJ. Depletion of intracellular thiols and increased production of 4-hydroxynonenal that occur during cryopreservation of stallion spermatozoa lead to caspase activation, loss of motility, and cell death. Biol Reprod. 2015;93:143. 1–11
Zhong H, Xiao M, Zarkovic K, Zhu M, Sa R, Lu J, et al. Mitochondrial control of apoptosis through modulation of cardiolipin oxidation in hepatocellular carcinoma: a novel link between oxidative stress and cancer. Free Radic Biol Med. 2017;102:67–76.
Hoesel B, Schmid JA. The complexity of NF-κB signaling in inflammation and cancer. Mol Cancer. 2013;12:86.
Page S, Fischer C, Baumgartner B, Haas M, Kreusel U, Loidl G, et al. 4-Hydroxynonenal prevents NF-κB activation and tumor necrosis factor expression by inhibiting IκB phosphorylation and subsequent proteolysis. J Biol Chem. 1999;274:11611–8.
Bodur C, Kutuk O, Tezil T, Basaga H. Inactivation of Bcl-2 through IκB kinase (IKK)-dependent phosphorylation mediates apoptosis upon exposure to 4-hydroxynonenal (HNE). J Cell Physiol. 2012;227:3556–65.
Meng X, Zhang S. MAPK cascades in plant disease resistance signaling. Annu Rev Phytopathol. 2013;51:245–66.
Preston GA, Zarella CS, Pendergraft WFI, Rudolph EH, Yang JJ, Sekura SB, et al. Novel effects of neutrophil-derived proteinase 3 and elastase on the vascular endothelium involve in vivo cleavage of NF-kappaB and proapoptotic changes in JNK, ERK, and p38 MAPK signaling pathways. J Am Soc Nephrol. 2002;13:2840.
Forman HJ, Dickinson DA, Iles KE. HNE––signaling pathways leading to its elimination. Mol Asp Med. 2003;24:189–94.
Giorgi C, Agnoletto C, Baldini C, Bononi A, Bonora M, Marchi S, et al. Redox control of protein kinase C: cell- and disease-specific aspects. Antioxid Redox Signal. 2010;13:1051–85.
Zhao M, Xia L, Chen G-Q. Protein kinase cδ in apoptosis: a brief overview. Arch Immunol Ther Exp. 2012;60:361–72.
Fearnhead HO, Dinsdale D, Cohen GM. An interleukin-1β-converting enzyme-like protease is a common mediator of apoptosis in thymocytes. FEBS Lett. 1995;375:283–8.
Pagano N, Longobardi V, De Canditiis C, Zuchegna C, Romano A, Michal Andrzej K, et al. Effect of caspase inhibitor Z‐VAD‐FMK on bovine sperm cryotolerance. Reprod Domest Anim. 2020;55:530–6.
Peter AT, Linde-Forsberg C. Efficacy of the anticaspase agent zVAD-fmk on post-thaw viability of canine spermatozoa. Theriogenology. 2003;59:1525–32.
Koopman G, Reutelingsperger CPM, Kuijten GAM, Keehnen RMJ, Pals ST, van Oers MHJ. Annexin V for flow cytometric detection of phosphatidylserine expression on B cells undergoing apoptosis. Blood. 1994;84:1415–20.
Glander H, Schaller J. Binding of annexin V to plasma membranes of human spermatozoa: a rapid assay for detection of membrane changes after cryostorage. Mol Hum Reprod. 1999;5:109–15.
Wallberg F, Tenev T, Meier P. Analysis of apoptosis and necroptosis by fluorescence-activated cell sorting. Cold Spring Harb Protoc. 2016;2016:pdb.prot087387.
Kabakov AE, Gabai VL. Cell death and survival assays. Methods Mol Biol. 2018;1709:107–27.
Said TM, Grunewald S, Paasch U, Rasch M, Agarwal A, Glander HJ. Effects of magnetic-activated cell sorting on sperm motility and cryosurvival rates. Fertil Steril. 2005;83:1442–6.
Grunewald S, Paasch U, Said TM, Rasch M, Agarwal A, Glander HJ. Magnetic-activated cell sorting before cryopreservation preserves mitochondrial integrity in human spermatozoa. Cell Tissue Bank. 2006;7:99–104.
Chen R, Xu J, She Y, Jiang T, Zhou S, Shi H, et al. Necrostatin-1 protects C2C12 myotubes from CoCl2-induced hypoxia. Int J Mol Med. 2018;41:2565–72.
Duru NK, Morshedi MS, Schuffner A, Oehninger S. Cryopreservation-thawing of fractionated human spermatozoa is associated with membrane phosphatidylserine externalization and not DNA fragmentation. J Androl. 2001;22:646–51.
Jiang X, Stockwell BR, Conrad M. Ferroptosis: mechanisms, biology and role in disease. Nat Rev Mol Cell Biol. 2021;22:266–82.
Ursini F, Maiorino M, Valente M, Ferri L, Gregolin C. Purification from pig liver of a protein which protects liposomes and biomembranes from peroxidative degradation and exhibits glutathione peroxidase activity on phosphatidylcholine hydroperoxides. Biochim Biophys Acta. 1982;710:197–211.
Yang WS, SriRamaratnam R, Welsch ME, Shimada K, Skouta R, Viswanathan VS, et al. Regulation of ferroptotic cancer cell death by GPX4. Cell. 2014;156:317–31.
Dixon SJ, Patel DN, Welsch M, Skouta R, Lee ED, Hayano M, et al. Pharmacological inhibition of cystine-glutamate exchange induces endoplasmic reticulum stress and ferroptosis. Elife. 2014;3:e02523.
Bersuker K, Hendricks JM, Li Z, Magtanong L, Ford B, Tang PH, et al. The CoQ oxidoreductase FSP1 acts parallel to GPX4 to inhibit ferroptosis. Nature. 2019;575:688–92.
Doll S, Freitas FP, Shah R, Aldrovandi M, da Silva MC, Ingold I, et al. FSP1 is a glutathione-independent ferroptosis suppressor. Nature. 2019;575:693–8.
Shah R, Shchepinov MS, Pratt DA. Resolving the role of lipoxygenases in the initiation and execution of ferroptosis. ACS Cent Sci. 2018;4:387–96.
Fenton HJH. Oxidation of tartaric acid in presence of iron. J Chem Soc Trans. 1894;65:899–910.
Patel SJ, Frey AG, Palenchar DJ, Achar S, Bullough KZ, Vashisht A, et al. A PCBP1–BolA2 chaperone complex delivers iron for cytosolic [2Fe–2S] cluster assembly. Nat Chem Biol. 2019;15:872–81.
Pinilla-Tenas JJ, Sparkman BK, Shawki A, Illing AC, Mitchell CJ, Zhao N, et al. Zip14 is a complex broad-scope metal-ion transporter whose functional properties support roles in the cellular uptake of zinc and nontransferrin-bound iron. Am J Physiol Cell Physiol. 2011;301:C862–C871.
Liuzzi JP, Aydemir F, Nam H, Knutson MD, Cousins RJ. Zip14 (Slc39a14) mediates non-transferrin-bound iron uptake into cells. Proc Natl Acad Sci USA. 2006;103:13612–7.
Andrews NC. The iron transporter DMT1. Int J Biochem Cell Biol. 1999;31:991–4.
Holmberg CG, Laurell C-B. Studies on the Capacity of Serum to Bind Iron. A contribution to our knowledge of the regulation mechanism of serum iron. Acta Physiol Scand. 1945;10:307–19.
Sendamarai AK, Ohgami RS, Fleming MD, Lawrence CM. Structure of the membrane proximal oxidoreductase domain of human Steap3, the dominant ferrireductase of the erythroid transferrin cycle. Proc Natl Acad Sci USA. 2008;105:7410–5.
Gao M, Monian P, Quadri N, Ramasamy R, Jiang X. Glutaminolysis and Transferrin regulate ferroptosis. Mol Cell. 2015;59:298–308.
Tang D, Chen X, Kang R, Kroemer G. Ferroptosis: molecular mechanisms and health implications. Cell Res. 2021;31:107–25.
Masaldan S, Clatworthy SAS, Gamell C, Meggyesy PM, Rigopoulos A-T, Haupt S, et al. Iron accumulation in senescent cells is coupled with impaired ferritinophagy and inhibition of ferroptosis. Redox Biol. 2018;14:100–15.
Wang Y, Sharma RK, Agarwal A. Effect of cryopreservation and sperm concentration on lipid peroxidation in human semen. Urology. 1997;50:409–13.
Bell M, Wang R, Hellstrom WJG, Sikka SC. Effect of cryoprotective additives and cryopreservation protocol on sperm membrane lipid peroxidation and recovery of motile human sperm. J Androl. 1993;14:472–8.
Alvarez JG, Storey BT. Evidence for increased lipid peroxidative damage and loss of superoxide dismutase activity as a mode of sublethal cryodamage to human sperm during cryopreservation. J Androl. 1992;13:232–41.
Suleiman SA, Ali ME, Zaki ZMS, El-Malik EMA, Nasr MA. Lipid peroxidation and human sperm motility: protective role of vitamin E. J Androl. 1996;17:530–7.
Alvarez JG, Touchstone JC, Blasco L, Storey BT. Spontaneous lipid peroxidation and production of hydrogen peroxide and superoxide in human spermatozoa. Superoxide dismutase as major enzyme protectant against oxygen toxicity. J Androl. 1987;8:338–48.
Du Y, Guo Z. Recent progress in ferroptosis: inducers and inhibitors. Cell Death Discov. 2022;8:1–10.
Nekoonam S, Nashtaei MS, naji M, Zangi BM, Amidi F. Effect of Trolox on sperm quality in normozospermia and oligozospermia during cryopreservation. Cryobiology. 2016;72:106–11.
Zhu Z, Fan X, Lv Y, Zhang N, Fan C, Zhang P, et al. Vitamin E analogue improves rabbit sperm quality during the process of cryopreservation through its antioxidative action. PLoS ONE. 2015;10:e0145383.
Silva SV, Soares AT, Batista AM, Almeida FC, Nunes JF, Peixoto CA, et al. Vitamin E (Trolox) addition to Tris-egg yolk extender preserves ram spermatozoon structure and kinematics after cryopreservation. Anim Reprod Sci. 2013;137:37–44.
Guthrie HD, Welch GR. Use of fluorescence-activated flow cytometry to determine membrane lipid peroxidation during hypothermic liquid storage and freeze-thawing of viable boar sperm loaded with 4, 4-difluoro-5-(4-phenyl-1,3-butadienyl)-4-bora-3a,4a-diaza-s-indacene-3-undecanoic acid1. J Anim Sci. 2007;85:1402–11.
Gerzilov V, Andreeva M, Tsvetanova E, Georgieva A, Alexandrova A. Improvement of diluted semen from Muscovy (Cairina moschata) drakes by the addition of water-soluble antioxidants. Reprod Domest Anim. 2023;58:1702–11.
Jannatifar R, Asa E, Sahraei SS, Verdi A, Piroozmanesh H. N-acetyl-l-cysteine and alpha lipoic acid are protective supplement on human sperm parameters in cryopreservation of asthenoteratozoospermia patients. Andrologia. 2022;54:e14612.
Shaygannia E, Ghandehari-Alavijeh R, Tavalaee M, Nasr-Esfahani MH. The protective effects of alpha lipoic acid on human sperm function during freezing-thawing. Cryo Lett. 2020;41:344–50.
Ren F, Feng T, Dai G, Wang Y, Zhu H, Hu J. Lycopene and alpha-lipoic acid improve semen antioxidant enzymes activity and cashmere goat sperm function after cryopreservation. Cryobiology. 2018;84:27–32.
Liu Y, Zhu W, Ni D, Zhou Z, Gu J, Zhang W, et al. Alpha lipoic acid antagonizes cytotoxicity of cobalt nanoparticles by inhibiting ferroptosis-like cell death. J Nanobiotechnol. 2020;18:141.
Ghibu S, Richard C, Vergely C, Zeller M, Cottin Y, Rochette L. Antioxidant properties of an endogenous thiol: alpha-lipoic acid, useful in the prevention of cardiovascular diseases. J Cardiovasc Pharmacol. 2009;54:391.
Meseguer M, Martinez-Conejero JA, Muriel L, Pellicer A, Remohi J, Garrido N. The human sperm glutathione system: a key role in male fertility and successful cryopreservation. Drug Metab Lett. 2007;1:121–6.
Meseguer M, Garrido N, Simón C, Pellicer A, Remohí J. Concentration of glutathione and expression of glutathione peroxidases 1 and 4 in fresh sperm provide a forecast of the outcome of cryopreservation of human spermatozoa. J Androl. 2004;25:773–80.
Stradaioli G, Noro T, Sylla L, Monaci M. Decrease in glutathione (GSH) content in bovine sperm after cryopreservation: Comparison between two extenders. Theriogenology. 2007;67:1249–55.
Ortiz-Rodriguez JM, Martín-Cano FE, Ortega-Ferrusola C, Masot J, Redondo E, Gázquez A, et al. The incorporation of cystine by the soluble carrier family 7 member 11 (SLC7A11) is a component of the redox regulatory mechanism in stallion spermatozoa. † Biol Reprod. 2019;101:208–22.
Zhu Z, Ren Z, Fan X, Pan Y, Lv S, Pan C, et al. Cysteine protects rabbit spermatozoa against reactive oxygen species-induced damages. PLoS ONE. 2017;12:e0181110.
Zou J, Wei L, Li D, Zhang Y, Wang G, Zhang L, et al. Effect of glutathione on sperm quality in guanzhong dairy goat sperm during cryopreservation. Front Vet Sci. 2021;8:771440.
Öğretmen F, İnanan BE, Kutluyer F, Kayim M. Effect of semen extender supplementation with cysteine on postthaw sperm quality, DNA damage, and fertilizing ability in the common carp (Cyprinus carpio). Theriogenology. 2015;83:1548–52.
Masoudi R, Sharafi M, Shahneh AZ, Khodaei-Motlagh M. Effects of reduced glutathione on the quality of rooster sperm during cryopreservation. Theriogenology. 2019;128:149–55.
Shi H, Li QY, Li H, Wang H-Y, Fan CX, Dong QY, et al. ROS-induced oxidative stress is a major contributor to sperm cryoinjury. Hum Reprod. 2024;39:310–25.
Sun P, Zhang G, Xian M, Zhang G, Wen F, Hu Z, et al. Proteomic analysis of frozen–thawed spermatozoa with different levels of freezability in dairy goats. Int J Mol Sci. 2023;24:15550.
Brown CW, Amante JJ, Chhoy P, Elaimy AL, Liu H, Zhu LJ, et al. Prominin2 drives ferroptosis resistance by stimulating iron export. Dev Cell. 2019;51:575–.e4.
Brinsko SP, Blanchard TL, Rigby SL, Love CC, Varner DD. Effects of dead spermatozoa on motion characteristics and membrane integrity of live spermatozoa in fresh and cooled-stored equine semen. Theriogenology. 2003;59:735–42.
Martinez-Alborcia MJ, Valverde A, Parrilla I, Vazquez JM, Martinez EA, Roca J. Detrimental effects of non-functional spermatozoa on the freezability of functional spermatozoa from boar ejaculate. PLoS ONE. 2012;7:e36550.
Riegman M, Sagie L, Galed C, Levin T, Steinberg N, Dixon SJ, et al. Ferroptosis occurs through an osmotic mechanism and propagates independently of cell rupture. Nat Cell Biol. 2020;22:1042–8.
Juncadella IJ, Kadl A, Sharma AK, Shim YM, Hochreiter-Hufford A, Borish L, et al. Apoptotic cell clearance by bronchial epithelial cells critically influences airway inflammation. Nature. 2013;493:547–51.
Monks J, Smith-Steinhart C, Kruk ER, Fadok VA, Henson PM. Epithelial cells remove apoptotic epithelial cells during post-lactation involution of the mouse mammary gland. Biol Reprod. 2008;78:586–94.
Mesa KR, Rompolas P, Zito G, Myung P, Sun TY, Brown S, et al. Niche-induced cell death and epithelial phagocytosis regulate hair follicle stem cell pool. Nature. 2015;522:94–97.
Elmore SA, Dixon D, Hailey JR, Harada T, Herbert RA, Maronpot RR, et al. Recommendations from the INHAND apoptosis/necrosis working group. Toxicol Pathol. 2016;44:173–88.
Riegman M, Bradbury MS, Overholtzer M. Population dynamics in cell death: mechanisms of propagation. Trends Cancer. 2019;5:558–68.
Link N, Chen P, Lu W-J, Pogue K, Chuong A, Mata M, et al. A collective form of cell death requires homeodomain interacting protein kinase. J Cell Biol. 2007;178:567–74.
Garcia-Hughes G, Link N, Ghosh AB, Abrams JM. Hid arbitrates collective cell death in the Drosophila wing. Mech Dev. 2015;138:349–55.
Vandenabeele P, Declercq W, Van Herreweghe F, Vanden Berghe T. The role of the kinases RIP1 and RIP3 in TNF-induced necrosis. Sci Signal. 2010;3:re4–re4.
Li J, McQuade T, Siemer AB, Napetschnig J, Moriwaki K, Hsiao Y-S, et al. The RIP1/RIP3 necrosome forms a functional amyloid signaling complex required for programmed necrosis. Cell. 2012;150:339–50.
Murphy JM, Czabotar PE, Hildebrand JM, Lucet IS, Zhang J-G, Alvarez-Diaz S, et al. The pseudokinase MLKL mediates necroptosis via a molecular switch mechanism. Immunity. 2013;39:443–53.
Cho Y, Challa S, Moquin D, Genga R, Ray TD, Guildford M, et al. Phosphorylation-driven assembly of the RIP1-RIP3 complex regulates programmed necrosis and virus-induced inflammation. Cell. 2009;137:1112–23.
Linkermann A, Green DR. Necroptosis. N Engl J Med. 2014;370:455–65.
Vercammen D, Beyaert R, Denecker G, Goossens V, Van Loo G, Declercq W, et al. Inhibition of caspases increases the sensitivity of L929 cells to necrosis mediated by tumor necrosis factor. J Exp Med. 1998;187:1477–85.
Holler N, Zaru R, Micheau O, Thome M, Attinger A, Valitutti S, et al. Fas triggers an alternative, caspase-8–independent cell death pathway using the kinase RIP as effector molecule. Nat Immunol. 2000;1:489–95.
Xiang J, Wan C, Guo R, Guo D. Is hydrogen peroxide a suitable apoptosis inducer for all cell types? Biomed Res Int. 2016;2016:e7343965.
O’Donnell MA, Perez-Jimenez E, Oberst A, Ng A, Massoumi R, Xavier R, et al. Caspase 8 inhibits programmed necrosis by processing CYLD. Nat Cell Biol. 2011;13:1437–42.
Li X, Zhong C-Q, Wu R, Xu X, Yang Z-H, Cai S, et al. RIP1-dependent linear and nonlinear recruitments of caspase-8 and RIP3 respectively to necrosome specify distinct cell death outcomes. Protein Cell. 2021;12:858–76.
Vandenabeele P, Vanden Berghe T, Festjens N. Caspase inhibitors promote alternative cell death pathways. Sci STKE. 2006;2006:pe44.
Sawai H. Differential effects of caspase inhibitors on TNF-induced necroptosis. Biochem Biophys Res Commun. 2013;432:451–5.
Zhang J, Song L, Jia J, Tian W, Lai R, Zhang Z, et al. Knowledge mapping of necroptosis from 2012 to 2021: a bibliometric analysis. Front Immunol. 2022;13:917155.
Sun TC, Li DM, Yu H, Song LL, Jia YJ, Lin L, et al. Bilateral varicocele leads to ferroptosis, pyroptosis and necroptosis of human spermatozoa and affects semen quality in infertile men. Front Cell Dev Biol. 2023;11:1091438.
Jung SE, Ahn JS, Kim YH, Oh HJ, Kim BJ, Ryu BY. Necrostatin-1 improves the cryopreservation efficiency of murine spermatogonial stem cells via suppression of necroptosis and apoptosis. Theriogenology. 2020;158:445–53.
Tvrda E, Peer R, Sikka SC, Agarwal A. Iron and copper in male reproduction: a double-edged sword. J Assist Reprod Genet. 2015;32:3–16.
Tsvetkov P, Coy S, Petrova B, Dreishpoon M, Verma A, Abdusamad M, et al. Copper induces cell death by targeting lipoylated TCA cycle proteins. Science. 2022;375:1254–61.
Eidi M, Eidi A, Pouyan O, Shahmohammadi P, Fazaeli R, Bahar M. Seminal plasma levels of copper and its relationship with seminal parameters. Int J Reprod Biomed. 2010;8:60–65.
Schmid TE, Grant PG, Marchetti F, Weldon RH, Eskenazi B, Wyrobek AJ. Elemental composition of human semen is associated with motility and genomic sperm defects among older men. Hum Reprod. 2013;28:274–82.
Knazicka Z, Tvrda E, Bardos L, Lukac N. Dose- and time-dependent effect of copper ions on the viability of bull spermatozoa in different media. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2012;47:1294–1300.
Roychoudhury S, Massanyi P, Bulla J, Choudhury MD, Straka L, Lukac N, et al. In vitro copper toxicity on rabbit spermatozoa motility, morphology and cell membrane integrity. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2010;45:1482–91.
Roblero L, Guadarrama A, Lopez T, Zegers-Hochschild F. Effect of copper ion on the motility, viability, acrosome reaction and fertilizing capacity of human spermatozoa in vitro. Reprod Fertil Dev. 1996;8:871–4.
Roy D, Dey S, Majumder GC, Bhattacharyya D. Copper: a biphasic regulator of caprine sperm forward progression. Syst Biol Reprod Med. 2014;60:52–57.
Thomas C, Mackey MM, Diaz AA, Cox DP. Hydroxyl radical is produced via the Fenton reaction in submitochondrial particles under oxidative stress: implications for diseases associated with iron accumulation. Redox Rep. 2009;14:102–8.
Xue Q, Yan D, Chen X, Li X, Kang R, Klionsky DJ, et al. Copper-dependent autophagic degradation of GPX4 drives ferroptosis. Autophagy. 2023;19:1982–96.
Filomeni G, De Zio D, Cecconi F. Oxidative stress and autophagy: the clash between damage and metabolic needs. Cell Death Differ. 2015;22:377–88.
Jung S, Jeong H, Yu S-W. Autophagy as a decisive process for cell death. Exp Mol Med. 2020;52:921–30.
Liu S, Yao S, Yang H, Liu S, Wang Y. Autophagy: regulator of cell death. Cell Death Dis. 2023;14:1–17.
Aparicio IM, Martin Muñoz P, Salido GM, Peña FJ, Tapia JA. The autophagy-related protein LC3 is processed in stallion spermatozoa during short-and long-term storage and the related stressful conditions. Animal. 2016;10:1182–91.
Uribe P, Meriño J, Matus CE, Schulz M, Zambrano F, Villegas JV, et al. Autophagy is activated in human spermatozoa subjected to oxidative stress and its inhibition impairs sperm quality and promotes cell death. Hum Reprod. 2022;37:680–95.
Ashkenazi A, Salvesen G. Regulated cell death: signaling and mechanisms. Annu Rev Cell Dev Biol. 2014;30:337–56.
Berghe TV, Linkermann A, Jouan-Lanhouet S, Walczak H, Vandenabeele P. Regulated necrosis: the expanding network of non-apoptotic cell death pathways. Nat Rev Mol Cell Biol. 2014;15:135–47.
Lalaoui N, Lindqvist LM, Sandow JJ, Ekert PG. The molecular relationships between apoptosis, autophagy and necroptosis. Semin Cell Dev Biol. 2015;39:63–69.
Green DR, Llambi F. Cell death signaling. Cold Spring Harb Perspect Biol. 2015;7:a006080.
Okazaki T, Yoshida S, Teshima H, Shimada M. The addition of calcium ion chelator, EGTA to thawing solution improves fertilizing ability in frozen-thawed boar sperm. Anim Sci J. 2011;82:412–9.
Suzuki-Migishima R, Hino T, Takabe M, Oda K, Migishima F, Morimoto Y, et al. Marked improvement of fertility of cryopreserved C57BL/6J mouse sperm by depletion of Ca2+ in medium. J Reprod Dev. 2009;55:386–92.
Antonouli S, Di Nisio V, Messini C, Samara M, Salumets A, Daponte A, et al. Sperm plasma membrane ion transporters and male fertility potential: a perspective under the prism of cryopreservation. Cryobiology. 2024;114:104845.
Baňas Š, Benko F, Ďuračka M, Lukáč N, Tvrdá E. Epicatechin prevents cryocapacitation of bovine spermatozoa through antioxidant activity and stabilization of transmembrane ion channels. Int J Mol Sci. 2023;24:2510.
Benko F, Fialková V, Žiarovská J, Ďuračka M, Lukáč N, Tvrdá E. In vitro versus cryo-induced capacitation of bovine spermatozoa, Part 2: Changes in the expression patterns of selected transmembrane channels and protein Kinase A. Int J Mol Sci. 2022;23:14646.
Cai Z, Jitkaew S, Zhao J, Chiang H-C, Choksi S, Liu J, et al. Plasma membrane translocation of trimerized MLKL protein is required for TNF-induced necroptosis. Nat Cell Biol. 2014;16:55–65.
Galluzzi L, Kepp O, Kroemer G. MLKL regulates necrotic plasma membrane permeabilization. Cell Res. 2014;24:139–40.
Pedrera L, Espiritu RA, Ros U, Weber J, Schmitt A, Stroh J, et al. Ferroptotic pores induce Ca2+ fluxes and ESCRT-III activation to modulate cell death kinetics. Cell Death Differ. 2021;28:1644–57.
Bejarano I, Lozano GM, Ortiz A, García JF, Paredes SD, Rodríguez AB, et al. Caspase 3 activation in human spermatozoa in response to hydrogen peroxide and progesterone. Fertil Steril. 2008;90:1340–7.
Boehning D, van Rossum DB, Patterson RL, Snyder SH. A peptide inhibitor of cytochrome c/inositol 1,4,5-trisphosphate receptor binding blocks intrinsic and extrinsic cell death pathways. Proc Natl Acad Sci USA. 2005;102:1466–71.
Oshimi Y, Miyazaki S. Fas antigen-mediated DNA fragmentation and apoptotic morphologic changes are regulated by elevated cytosolic Ca2+ level. J Immunol. 1995;154:599–609.
Wozniak AL, Wang X, Stieren ES, Scarbrough SG, Elferink CJ, Boehning D. Requirement of biphasic calcium release from the endoplasmic reticulum for Fas-mediated apoptosis. J Cell Biol. 2006;175:709–14.
Aparicio IM, Espino J, Bejarano I, Gallardo-Soler A, Campo ML, Salido GM, et al. Autophagy-related proteins are functionally active in human spermatozoa and may be involved in the regulation of cell survival and motility. Sci Rep. 2016;6:33647.
Gump JM, Staskiewicz L, Morgan MJ, Bamberg A, Riches DWH, Thorburn A. Autophagy variation within a cell population determines cell fate through selective degradation of Fap-1. Nat Cell Biol. 2014;16:47–54.
Yousefi S, Perozzo R, Schmid I, Ziemiecki A, Schaffner T, Scapozza L, et al. Calpain-mediated cleavage of Atg5 switches autophagy to apoptosis. Nat Cell Biol. 2006;8:1124–32.
Rubinstein AD, Eisenstein M, Ber Y, Bialik S, Kimchi A. The autophagy protein Atg12 associates with antiapoptotic Bcl-2 family members to promote mitochondrial apoptosis. Mol Cell. 2011;44:698–709.
He W, Wang Q, Srinivasan B, Xu J, Padilla MT, Li Z, et al. A JNK-mediated autophagy pathway that triggers c-IAP degradation and necroptosis for anticancer chemotherapy. Oncogene. 2014;33:3004–13.
Loos B, Engelbrecht A-M, Lockshin RA, Klionsky DJ, Zakeri Z. The variability of autophagy and cell death susceptibility: Unanswered questions. Autophagy. 2013;9:1270–85.
Leist M, Single B, Castoldi AF, Kühnle S, Nicotera P. Intracellular adenosine triphosphate (ATP) concentration: a switch in the decision between apoptosis and necrosis. J Exp Med. 1997;185:1481–6.
Goodall ML, Fitzwalter BE, Zahedi S, Wu M, Rodriguez D, Mulcahy-Levy JM, et al. The autophagy machinery controls cell death switching between apoptosis and necroptosis. Dev Cell. 2016;37:337–49.
Samare-Najaf M, Neisy A, Samareh A, Moghadam D, Jamali N, Zarei R, et al. The constructive and destructive impact of autophagy on both genders’ reproducibility, a comprehensive review. Autophagy. 2023;19:3033–61.
Chen X, Kang R, Kroemer G, Tang D. Organelle-specific regulation of ferroptosis. Cell Death Differ. 2021;28:2843–56.
Basit F, van Oppen LM, Schöckel L, Bossenbroek HM, van Emst-de Vries SE, Hermeling JC, et al. Mitochondrial complex I inhibition triggers a mitophagy-dependent ROS increase leading to necroptosis and ferroptosis in melanoma cells. Cell Death Dis. 2017;8:e2716–e2716.
Li C, Liu J, Hou W, Kang R, Tang D. STING1 promotes ferroptosis through MFN1/2-dependent mitochondrial fusion. Front Cell Dev Biol. 2021;9:698679.
Chen X, Tsvetkov AS, Shen H-M, Isidoro C, Ktistakis NT, Linkermann A, et al. International consensus guidelines for the definition, detection, and interpretation of autophagy-dependent ferroptosis. Autophagy 2024:1–34.
Acknowledgements
We would like to acknowledge the reviewers for their helpful comments on this paper.
Funding
This work was supported by a grant from the National Key R&D Program of China (grant number 2021YFD1300901) and the 12th Inner Mongolia “Grassland Talent” High-level Talent Training Project (2023).
Author information
Authors and Affiliations
Contributions
Erhan Hai and Jiaxin Zhang wrote the manuscript. Erhan Hai, Jiaxin Zhang and Boyuan Li revised it. Erhan Hai and Jian Zhang created the figures. All authors reviewed and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hai, E., Li, B., Zhang, J. et al. Sperm freezing damage: the role of regulated cell death. Cell Death Discov. 10, 239 (2024). https://doi.org/10.1038/s41420-024-02013-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41420-024-02013-3