Abstract
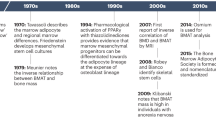
The skeleton is diverse in its functions, which include mechanical support, movement, blood cell production, mineral storage and endocrine regulation. This multifaceted role is achieved through an interplay of osteoblasts, chondrocytes, bone marrow adipocytes and stromal cells, all generated from skeletal stem cells. Emerging evidence shows the importance of cellular metabolism in the molecular control of the skeletal system. The different skeletal cell types not only have distinct metabolic demands relating to their particular functions but also are affected by microenvironmental constraints. Specific metabolites control skeletal stem cell maintenance, direct lineage allocation and mediate cellular communication. Here, we discuss recent findings on the roles of cellular metabolism in determining skeletal stem cell fate, coordinating osteoblast and chondrocyte function, and organizing stromal support of haematopoiesis. We also consider metabolic dysregulation in skeletal ageing and degenerative diseases, and provide an outlook on how the field may evolve in the coming years.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Capulli, M., Paone, R. & Rucci, N. Osteoblast and osteocyte: games without frontiers. Arch. Biochem. Biophys. 561, 3–12 (2014).
Rodan, G. A. Introduction to bone biology. Bone 13, S3–S6 (1992).
Bonewald, L. F. The amazing osteocyte. J. Bone Miner. Res. 26, 229–238 (2011).
Krishnan, Y. & Grodzinsky, A. J. Cartilage diseases. Matrix Biol. 71–72, 51–69 (2018).
Hallett, S. A., Ono, W. & Ono, N. Growth plate chondrocytes: skeletal development, growth and beyond. Int. J. Mol. Sci. 20, 6009 (2019).
Roberts, S. J., van Gastel, N., Carmeliet, G. & Luyten, F. P. Uncovering the periosteum for skeletal regeneration: the stem cell that lies beneath. Bone 70, 10–18 (2015).
Bukowska, J. et al. Bone marrow adipocyte developmental origin and biology. Curr. Osteoporos. Rep. 16, 312–319 (2018).
Crane, G. M., Jeffery, E. & Morrison, S. J. Adult haematopoietic stem cell niches. Nat. Rev. Immunol. 17, 573–590 (2017).
Hoggatt, J., Kfoury, Y. & Scadden, D. T. Hematopoietic stem cell niche in health and disease. Annu. Rev. Pathol. 11, 555–581 (2016).
Baryawno, N. et al. A cellular taxonomy of the bone marrow stroma in homeostasis and leukemia. Cell 177, 1915–1932.e1916 (2019).
Severe, N. et al. Stress-induced changes in bone marrow stromal cell populations revealed through single-cell protein expression mapping. Cell Stem Cell 25, 570–583.e577 (2019).
Tikhonova, A. N. et al. The bone marrow microenvironment at single-cell resolution. Nature 569, 222–228 (2019).
Ambrosi, T. H., Longaker, M. T. & Chan, C. K. F. A revised perspective of skeletal stem cell biology. Front. Cell Dev. Biol. 7, 189 (2019).
Matsushita, Y., Ono, W. & Ono, N. Skeletal stem cells for bone development and repair: diversity matters. Curr. Osteoporos. Rep. 18, 189–198 (2020).
Serowoky, M. A., Arata, C. E., Crump, J. G. & Mariani, F. V. Skeletal stem cells: insights into maintaining and regenerating the skeleton. Development 147, dev179325 (2020).
Spencer, J. A. et al. Direct measurement of local oxygen concentration in the bone marrow of live animals. Nature 508, 269–273 (2014).
Chandel, N. S., Jasper, H., Ho, T. T. & Passegué, E. Metabolic regulation of stem cell function in tissue homeostasis and organismal ageing. Nat. Cell Biol. 18, 823–832 (2016).
Salazar-Noratto, G. E. et al. Understanding and leveraging cell metabolism to enhance mesenchymal stem cell transplantation survival in tissue engineering and regenerative medicine applications. Stem Cells 38, 22–33 (2020).
Lunt, S. Y. & Vander Heiden, M. G. Aerobic glycolysis: meeting the metabolic requirements of cell proliferation. Annu. Rev. Cell Dev. Biol. 27, 441–464 (2011).
Shum, L. C., White, N. S., Mills, B. N., Bentley, K. L. & Eliseev, R. A. Energy metabolism in mesenchymal stem cells during osteogenic differentiation. Stem Cells Dev. 25, 114–122 (2016).
Stegen, S. et al. Adequate hypoxia inducible factor 1α signaling is indispensable for bone regeneration. Bone 87, 176–186 (2016).
Tournaire, G. et al. Nestin-GFP transgene labels skeletal progenitors in the periosteum. Bone 133, 115259 (2020).
Martínez-Reyes, I. & Chandel, N. S. Mitochondrial TCA cycle metabolites control physiology and disease. Nat. Commun. 11, 102 (2020).
Fillmore, N. et al. Effect of fatty acids on human bone marrow mesenchymal stem cell energy metabolism and survival. PLoS ONE 10, e0120257 (2015).
van Gastel, N. et al. Lipid availability determines fate of skeletal progenitor cells via SOX9. Nature 579, 111–117 (2020).
Board, M. et al. Acetoacetate is a more efficient energy-yielding substrate for human mesenchymal stem cells than glucose and generates fewer reactive oxygen species. Int. J. Biochem. Cell Biol. 88, 75–83 (2017).
Newman, J. C. & Verdin, E. β-Hydroxybutyrate: a signaling metabolite. Annu. Rev. Nutr. 37, 51–76 (2017).
Kurmi, K. & Haigis, M. C. Nitrogen metabolism in cancer and immunity. Trends Cell Biol. 30, 408–424 (2020).
Hu, G. et al. The amino acid sensor Eif2ak4/GCN2 is required for proliferation of osteoblast progenitors in mice. J. Bone Miner. Res. 35, 2004–2014 (2020).
Chen, Y. et al. miR-206 inhibits osteogenic differentiation of bone marrow mesenchymal stem cells by targetting glutaminase. Biosci. Rep. 39, BSR20181108 (2019).
Stegen, S. et al. Glutamine metabolism controls chondrocyte identity and function. Dev. Cell 53, 530–544.e8 (2020).
Stegen, S. et al. HIF-1α promotes glutamine-mediated redox homeostasis and glycogen-dependent bioenergetics to support postimplantation bone cell survival. Cell Metab. 23, 265–279 (2016).
Yu, Y. et al. Glutamine metabolism regulates proliferation and lineage allocation in skeletal stem cells. Cell Metab. 29, 966–978.e964 (2019).
DeFalco, J. et al. Virus-assisted mapping of neural inputs to a feeding center in the hypothalamus. Science 291, 2608–2613 (2001).
Masson, J. et al. Mice lacking brain/kidney phosphate-activated glutaminase have impaired glutamatergic synaptic transmission, altered breathing, disorganized goal-directed behavior and die shortly after birth. J. Neurosci. 26, 4660–4671 (2006).
Davidson, S. M. et al. Environment impacts the metabolic dependencies of Ras-driven non-small cell lung cancer. Cell Metab. 23, 517–528 (2016).
Tardito, S. et al. Glutamine synthetase activity fuels nucleotide biosynthesis and supports growth of glutamine-restricted glioblastoma. Nat. Cell Biol. 17, 1556–1568 (2015).
van Gastel, N. et al. Induction of a timed metabolic collapse to overcome cancer chemoresistance. Cell Metab. 32, 391–403.e6 (2020).
Kristensen, H. B., Andersen, T. L., Marcussen, N., Rolighed, L. & Delaisse, J. M. Increased presence of capillaries next to remodeling sites in adult human cancellous bone. J. Bone Miner. Res. 28, 574–585 (2013).
Prisby, R. et al. Intermittent PTH(1-84) is osteoanabolic but not osteoangiogenic and relocates bone marrow blood vessels closer to bone-forming sites. J. Bone Miner. Res. 26, 2583–2596 (2011).
Dirckx, N. et al. Vhl deletion in osteoblasts boosts cellular glycolysis and improves global glucose metabolism. J. Clin. Invest. 128, 1087–1105 (2018).
Zoch, M. L., Abou, D. S., Clemens, T. L., Thorek, D. L. & Riddle, R. C. In vivo radiometric analysis of glucose uptake and distribution in mouse bone. Bone Res. 4, 16004 (2016).
Li, Z. et al. Glucose transporter-4 facilitates insulin-stimulated glucose uptake in osteoblasts. Endocrinology 157, 4094–4103 (2016).
Wei, J. et al. Glucose uptake and Runx2 synergize to orchestrate osteoblast differentiation and bone formation. Cell 161, 1576–1591 (2015).
Zoidis, E., Ghirlanda-Keller, C. & Schmid, C. Stimulation of glucose transport in osteoblastic cells by parathyroid hormone and insulin-like growth factor I. Mol. Cell. Biochem. 348, 33–42 (2011).
Dirckx, N., Moorer, M. C., Clemens, T. L. & Riddle, R. C. The role of osteoblasts in energy homeostasis. Nat. Rev. Endocrinol. 15, 651–665 (2019).
Lee, W. C., Ji, X., Nissim, I. & Long, F. Malic enzyme couples mitochondria with aerobic glycolysis in osteoblasts. Cell Rep. 32, 108108 (2020).
Borle, A. B., Nichols, N. & Nichols, G. Jr. Metabolic studies of bone in vitro. I. Normal bone. J. Biol. Chem. 235, 1206–1210 (1960).
Esen, E., Lee, S. Y., Wice, B. M. & Long, F. PTH promotes bone anabolism by stimulating aerobic glycolysis via IGF signaling. J. Bone Miner. Res. 30, 2137 (2015).
Regan, J. N. et al. Up-regulation of glycolytic metabolism is required for HIF1α-driven bone formation. Proc. Natl Acad. Sci. USA 111, 8673–8678 (2014).
Hilton, M. J. et al. Notch signaling maintains bone marrow mesenchymal progenitors by suppressing osteoblast differentiation. Nat. Med. 14, 306–314 (2008).
Lee, S. Y. & Long, F. Notch signaling suppresses glucose metabolism in mesenchymal progenitors to restrict osteoblast differentiation. J. Clin. Invest. 128, 5573–5586 (2018).
Chen, H. et al. Increased glycolysis mediates Wnt7b-induced bone formation. FASEB J. 33, 7810–7821 (2019).
Esen, E. et al. WNT-LRP5 signaling induces Warburg effect through mTORC2 activation during osteoblast differentiation. Cell Metab. 17, 745–755 (2013).
Schmid, C., Steiner, T. & Froesch, E. R. Parathormone promotes glycogen formation from [14C]glucose in cultured osteoblast-like cells. FEBS Lett. 148, 31–34 (1982).
Schajowicz, F. & Cabrini, R. L. Histochemical studies on glycogen in normal ossification and calcification. J. Bone Joint Surg. Am. 40-A, 1081–1092 (1958).
Scott, B. L. & Glimcher, M. J. Distribution of glycogen in osteoblasts of the fetal rat. J. Ultrastruct. Res. 36, 565–586 (1971).
Dodds, R. A., Ali, N., Pead, M. J. & Lanyon, L. E. Early loading-related changes in the activity of glucose 6-phosphate dehydrogenase and alkaline phosphatase in osteocytes and periosteal osteoblasts in rat fibulae in vivo. J. Bone Miner. Res. 8, 261–267 (1993).
Dodds, R. A., Catterall, A., Bitensky, L. & Chayen, J. Effects on fracture healing of an antagonist of the vitamin K cycle. Calcif. Tissue Int. 36, 233–238 (1984).
Dodds, R. A., Catterall, A., Bitensky, L. & Chayen, J. Abnormalities in fracture healing induced by vitamin B6-deficiency in rats. Bone 7, 489–495 (1986).
Chen, C. T., Shih, Y. R., Kuo, T. K., Lee, O. K. & Wei, Y. H. Coordinated changes of mitochondrial biogenesis and antioxidant enzymes during osteogenic differentiation of human mesenchymal stem cells. Stem Cells 26, 960–968 (2008).
Guntur, A. R., Le, P. T., Farber, C. R. & Rosen, C. J. Bioenergetics during calvarial osteoblast differentiation reflect strain differences in bone mass. Endocrinology 155, 1589–1595 (2014).
Yu, B. et al. PGC-1α controls skeletal stem cell fate and bone-fat balance in osteoporosis and skeletal aging by inducing TAZ. Cell Stem Cell 23, 193–209.e5 (2018).
Pan, J. X. et al. APP promotes osteoblast survival and bone formation by regulating mitochondrial function and preventing oxidative stress. Cell Death Dis. 9, 1077 (2018).
Morganti, C. et al. Citrate mediates crosstalk between mitochondria and the nucleus to promote human mesenchymal stem cell in vitro osteogenesis. Cells 9, 1034 (2020).
Shares, B. H., Busch, M., White, N., Shum, L. & Eliseev, R. A. Active mitochondria support osteogenic differentiation by stimulating β-catenin acetylation. J. Biol. Chem. 293, 16019–16027 (2018).
Franklin, R. B., Chellaiah, M., Zou, J., Reynolds, M. A. & Costello, L. C. Evidence that osteoblasts are specialized citrate-producing cells that provide the citrate for incorporation into the structure of bone. Open Bone J. 6, 1–7 (2014).
Karner, C. M. et al. Wnt Protein signaling reduces nuclear acetyl-CoA levels to suppress gene expression during osteoblast differentiation. J. Biol. Chem. 291, 13028–13039 (2016).
Adamek, G., Felix, R., Guenther, H. L. & Fleisch, H. Fatty acid oxidation in bone tissue and bone cells in culture. Characterization and hormonal influences. Biochem. J. 248, 129–137 (1987).
Dunham, J. et al. Aerobic glycolysis of bone and cartilage: the possible involvement of fatty acid oxidation. Cell Biochem. Funct. 1, 168–172 (1983).
Kim, S. P. et al. Fatty acid oxidation by the osteoblast is required for normal bone acquisition in a sex- and diet-dependent manner. JCI Insight 2, e92704 (2017).
Niemeier, A. et al. Uptake of postprandial lipoproteins into bone in vivo: impact on osteoblast function. Bone 43, 230–237 (2008).
Müller, D. I. H. et al. PPARδ-mediated mitochondrial rewiring of osteoblasts determines bone mass. Sci. Rep. 10, 8428 (2020).
Frey, J. L. et al. Wnt-Lrp5 signaling regulates fatty acid metabolism in the osteoblast. Mol. Cell. Biol. 35, 1979–1991 (2015).
Stegen, S. et al. Glutamine metabolism in osteoprogenitors is required for bone mass accrual and PTH‐induced bone anabolism in male mice.J. Bone Miner. Res. https://doi.org/10.1002/jbmr.4219 (2020).
Karner, C. M., Esen, E., Okunade, A. L., Patterson, B. W. & Long, F. Increased glutamine catabolism mediates bone anabolism in response to WNT signaling. J. Clin. Invest. 125, 551–562 (2015).
Torzilli, P. A., Arduino, J. M., Gregory, J. D. & Bansal, M. Effect of proteoglycan removal on solute mobility in articular cartilage. J. Biomech. 30, 895–902 (1997).
Torzilli, P. A., Grande, D. A. & Arduino, J. M. Diffusive properties of immature articular cartilage. J. Biomed. Mater. Res. 40, 132–138 (1998).
Amarilio, R. et al. HIF1alpha regulation of Sox9 is necessary to maintain differentiation of hypoxic prechondrogenic cells during early skeletogenesis. Development 134, 3917–3928 (2007).
Maes, C. et al. Soluble VEGF isoforms are essential for establishing epiphyseal vascularization and regulating chondrocyte development and survival. J. Clin. Invest. 113, 188–199 (2004).
Robins, J. C. et al. Hypoxia induces chondrocyte-specific gene expression in mesenchymal cells in association with transcriptional activation of Sox9. Bone 37, 313–322 (2005).
Schipani, E. et al. Hypoxia in cartilage: HIF-1alpha is essential for chondrocyte growth arrest and survival. Genes Dev. 15, 2865–2876 (2001).
Maes, C. et al. VEGF-independent cell-autonomous functions of HIF-1α regulating oxygen consumption in fetal cartilage are critical for chondrocyte survival. J. Bone Miner. Res. 27, 596–609 (2012).
Bywaters, E. G. L. Metabolism of cartilage. Nature 138, 30–31 (1936).
Kunin, A. S. & Krane, S. M. The effect of dietary phosphorus on the intermediary metabolism of epiphyseal cartilage from rachitic rats. Biochim. Biophys. Acta 107, 203–214 (1965).
Hough, S., Russell, J. E., Teitelbaum, S. L. & Avioli, L. V. Regulation of epiphyseal cartilage metabolism and morphology in the chronic diabetic rat. Calcif. Tissue Int. 35, 115–121 (1983).
Silverton, S. F., Matsumoto, H., DeBolt, K., Reginato, A. & Shapiro, I. M. Pentose phosphate shunt metabolism by cells of the chick growth cartilage. Bone 10, 45–51 (1989).
Lee, S. Y., Abel, E. D. & Long, F. Glucose metabolism induced by Bmp signaling is essential for murine skeletal development. Nat. Commun. 9, 4831 (2018).
Stegen, S. et al. HIF-1α metabolically controls collagen synthesis and modification in chondrocytes. Nature 565, 511–515 (2019).
Daimon, T. The presence and distribution of glycogen particles in chondrogenic cells of the tibiotarsal anlage of developing chick embryos. Calcif. Tissue Res. 23, 45–51 (1977).
Horigome, Y. et al. Loss of autophagy in chondrocytes causes severe growth retardation. Autophagy 16, 501–511 (2020).
Daniëls, V. W. et al. Cancer cells differentially activate and thrive on de novo lipid synthesis pathways in a low-lipid environment. PLoS ONE 9, e106913 (2014).
Kikuchi, M. et al. Crucial role of Elovl6 in chondrocyte growth and differentiation during growth plate development in mice. PLoS ONE 11, e0159375 (2016).
Handley, C. J., Speight, G., Leyden, K. M. & Lowther, D. A. Extracellular matrix metabolism by chondrocytes. 7. Evidence that L-glutamine is an essential amino acid for chondrocytes and other connective tissue cells. Biochim. Biophys. Acta 627, 324–331 (1980).
Scheller, E. L. et al. Region-specific variation in the properties of skeletal adipocytes reveals regulated and constitutive marrow adipose tissues. Nat. Commun. 6, 7808 (2015).
Li, Y., Meng, Y. & Yu, X. The unique metabolic characteristics of bone marrow adipose tissue. Front. Endocrinol. 10, 69 (2019).
Maridas, D. E. et al. Progenitor recruitment and adipogenic lipolysis contribute to the anabolic actions of parathyroid hormone on the skeleton. FASEB J. 33, 2885–2898 (2019).
Tencerova, M. et al. Metabolic programming determines the lineage-differentiation fate of murine bone marrow stromal progenitor cells. Bone Res. 7, 35 (2019).
Tormos, K. V. et al. Mitochondrial complex III ROS regulate adipocyte differentiation. Cell Metab. 14, 537–544 (2011).
Collins, J. M. et al. De novo lipogenesis in the differentiating human adipocyte can provide all fatty acids necessary for maturation. J. Lipid Res. 52, 1683–1692 (2011).
Suchacki, K. J. et al. Bone marrow adipose tissue is a unique adipose subtype with distinct roles in glucose homeostasis. Nat. Commun. 11, 3097 (2020).
Wellen, K. E. et al. ATP-citrate lyase links cellular metabolism to histone acetylation. Science 324, 1076–1080 (2009).
Attane, C. et al. Human bone marrow is comprised of adipocytes with specific lipid metabolism. Cell Rep. 30, 949–958.e946 (2020).
Scheller, E. L. et al. Bone marrow adipocytes resist lipolysis and remodeling in response to β-adrenergic stimulation. Bone 118, 32–41 (2019).
Hofer, M. et al. The pharmacological activation of adenosine A1 and A3 receptors does not modulate the long- or short-term repopulating ability of hematopoietic stem and multipotent progenitor cells in mice. Purinergic Signal. 9, 207–214 (2013).
Rossi, L., Salvestrini, V., Ferrari, D., Di Virgilio, F. & Lemoli, R. M. The sixth sense: hematopoietic stem cells detect danger through purinergic signaling. Blood 120, 2365–2375 (2012).
Taya, Y. et al. Depleting dietary valine permits nonmyeloablative mouse hematopoietic stem cell transplantation. Science 354, 1152–1155 (2016).
Zhang, W. et al. Stromal control of cystine metabolism promotes cancer cell survival in chronic lymphocytic leukaemia. Nat. Cell Biol. 14, 276–286 (2012).
Showalter, M. R. et al. Primed mesenchymal stem cells package exosomes with metabolites associated with immunomodulation. Biochem. Biophys. Res. Commun. 512, 729–735 (2019).
Mistry, J. J. et al. ROS-mediated PI3K activation drives mitochondrial transfer from stromal cells to hematopoietic stem cells in response to infection. Proc. Natl Acad. Sci. USA 116, 24610–24619 (2019).
Moschoi, R. et al. Protective mitochondrial transfer from bone marrow stromal cells to acute myeloid leukemic cells during chemotherapy. Blood 128, 253–264 (2016).
Shafat, M. S. et al. Leukemic blasts program bone marrow adipocytes to generate a protumoral microenvironment. Blood 129, 1320–1332 (2017).
Grote, C., Reinhardt, D., Zhang, M. & Wang, J. Regulatory mechanisms and clinical manifestations of musculoskeletal aging. J. Orthop. Res. 37, 1475–1488 (2019).
Bellantuono, I., Aldahmash, A. & Kassem, M. Aging of marrow stromal (skeletal) stem cells and their contribution to age-related bone loss. Biochim. Biophys. Acta 1792, 364–370 (2009).
Neri, S. & Borzì, R. M. Molecular mechanisms contributing to mesenchymal stromal cell aging. Biomolecules 10, 340 (2020).
Song, J. et al. Nicotinamide mononucleotide promotes osteogenesis and reduces adipogenesis by regulating mesenchymal stromal cells via the SIRT1 pathway in aged bone marrow. Cell Death Dis. 10, 336 (2019).
Sui, B., Hu, C. & Jin, Y. Mitochondrial metabolic failure in telomere attrition-provoked aging of bone marrow mesenchymal stem cells. Biogerontology 17, 267–279 (2016).
Huang, T. et al. Aging reduces an ERRalpha-directed mitochondrial glutaminase expression suppressing glutamine anaplerosis and osteogenic differentiation of mesenchymal stem cells. Stem Cells 35, 411–424 (2017).
Kondrikov, D. et al. Kynurenine inhibits autophagy and promotes senescence in aged bone marrow mesenchymal stem cells through the aryl hydrocarbon receptor pathway. Exp. Gerontol. 130, 110805 (2020).
Pierce, J. L. et al. Kynurenine suppresses osteoblastic cell energetics in vitro and osteoblast numbers in vivo. Exp. Gerontol. 130, 110818 (2020).
Hadjiargyrou, M. & O’Keefe, R. J. The convergence of fracture repair and stem cells: interplay of genes, aging, environmental factors and disease. J. Bone Miner. Res. 29, 2307–2322 (2014).
Mobasheri, A. et al. The role of metabolism in the pathogenesis of osteoarthritis. Nat. Rev. Rheumatol. 13, 302–311 (2017).
Arra, M. et al. LDHA-mediated ROS generation in chondrocytes is a potential therapeutic target for osteoarthritis. Nat. Commun. 11, 3427 (2020).
Tang, Q. et al. Trehalose ameliorates oxidative stress-mediated mitochondrial dysfunction and ER stress via selective autophagy stimulation and autophagic flux restoration in osteoarthritis development. Cell Death Dis. 8, e3081 (2017).
Hu, S. et al. Stabilization of HIF-1α alleviates osteoarthritis via enhancing mitophagy. Cell Death Dis. 11, 481 (2020).
Choi, W. S. et al. The CH25H-CYP7B1-RORα axis of cholesterol metabolism regulates osteoarthritis. Nature 566, 254–258 (2019).
Sekar, S. et al. Saturated fatty acids induce development of both metabolic syndrome and osteoarthritis in rats. Sci. Rep. 7, 46457 (2017).
Ratneswaran, A. et al. Peroxisome proliferator-activated receptor δ promotes the progression of posttraumatic osteoarthritis in a mouse model. Arthritis Rheumatol. 67, 454–464 (2015).
Akasaki, Y. et al. Dysregulated FOXO transcription factors in articular cartilage in aging and osteoarthritis. Osteoarthritis Cartilage 22, 162–170 (2014).
Zhong, L., Huang, X., Karperien, M. & Post, J. N. Correlation between gene expression and osteoarthritis progression in human. Int. J. Mol. Sci. 17, 1126 (2016).
Ashraf, S., Mapp, P. I. & Walsh, D. A. Contributions of angiogenesis to inflammation, joint damage, and pain in a rat model of osteoarthritis. Arthritis Rheum. 63, 2700–2710 (2011).
Elefteriou, F. & Yang, X. Genetic mouse models for bone studies—strengths and limitations. Bone 49, 1242–1254 (2011).
Stiers, P. J., van Gastel, N., Moermans, K., Stockmans, I. & Carmeliet, G. Regulatory elements driving the expression of skeletal lineage reporters differ during bone development and adulthood. Bone 105, 154–162 (2017).
Ast, T. & Mootha, V. K. Oxygen and mammalian cell culture: are we repeating the experiment of Dr. Ox? Nat. Metab. 1, 858–860 (2019).
Lagziel, S., Gottlieb, E. & Shlomi, T. Mind your media. Nat. Metab. https://doi.org/10.1038/s42255-020-00299-y (2020).
Agathocleous, M. et al. Ascorbate regulates haematopoietic stem cell function and leukaemogenesis. Nature 549, 476–481 (2017).
Ma, E. H. et al. Metabolic profiling using stable isotope tracing reveals distinct patterns of glucose utilization by physiologically activated CD8+ T cells. Immunity 51, 856–870.e855 (2019).
Hartmann, F.J. et al. Single-cell metabolic profiling of human cytotoxic T cells. Nat. Biotechnol. https://doi.org/10.1038/s41587-020-0651-8 (2020).
Levine, L.S. et al. Single-cell metabolic dynamics of early activated CD8 T cells during the primary immune response to infection. Preprint at bioRxiv https://doi.org/10.1101/2020.01.21.911545 (2020).
Narendra, D. P. & Steinhauser, M. L. Metabolic analysis at the nanoscale with multi-isotope imaging mass spectrometry (MIMS). Curr. Protoc. Cell Biol. 88, e111 (2020).
DiGirolamo, D. J., Clemens, T. L. & Kousteni, S. The skeleton as an endocrine organ. Nat. Rev. Rheumatol. 8, 674–683 (2012).
Acknowledgements
N.v.G. is supported by a Young Investigator Award from Alex’s Lemonade Stand Foundation for Childhood Cancer and Tap Cancer Out, and by funding from the de Duve Institute. G.C. receives funding from FWO G0B3418 and G0C5120, KUL-C24/17/077.
Author information
Authors and Affiliations
Contributions
N.v.G. and G.C. conceived the idea, wrote and revised the manuscript and approved the final version; N.v.G. prepared the figures.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Primary Handling Editors: Christoph Schmitt; Pooja Jha. Nature Metabolism thanks Ryan C. Riddle, Erica Scheller and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
van Gastel, N., Carmeliet, G. Metabolic regulation of skeletal cell fate and function in physiology and disease. Nat Metab 3, 11–20 (2021). https://doi.org/10.1038/s42255-020-00321-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s42255-020-00321-3
This article is cited by
-
The serine synthesis pathway drives osteoclast differentiation through epigenetic regulation of NFATc1 expression
Nature Metabolism (2024)
-
Metabolic regulation of skeletal cell fate and function
Nature Reviews Endocrinology (2024)
-
SIRT1 maintains bone homeostasis by regulating osteoblast glycolysis through GOT1
Cellular and Molecular Life Sciences (2024)
-
Molecular mechanisms of cellular metabolic homeostasis in stem cells
International Journal of Oral Science (2023)
-
Insights into skeletal stem cells
Bone Research (2022)