Abstract
Catheter-based embolization has become a widely adopted minimally-invasive treatment for a broad range of applications. However, assessment of embolization endpoints requires x-ray fluoroscopic monitoring, exposing patients and physicians performing embolization procedures to harmful ionizing radiation. Moreover, x-ray fluoroscopy assessment of embolization endpoints is low sensitivity, subjective, and may not reflect the actual physiology of blood flow reduction, thus providing little oversight of the embolization procedure. Inspired by the observation that the dielectric properties of blood differ from those of fluids injected during the embolization procedure, a customized angiographic catheter was created with embedded electrodes for catheter-based electrochemical impedance spectroscopy as a way to monitor embolization. Real-time electrochemical impedance spectroscopy was performed in a phantom and compared to visual and videographic monitoring. Electrochemical impedance spectroscopy was able to sense endpoints of embolization, including stasis, reflux, and persistent flow. This new technique offers a label-free method of sensing embolization progress with potentially higher sensitivity and reproducibility compared to x-ray, as well as offer substantial reduction in x-ray exposure to patients and physicians.
Similar content being viewed by others
Introduction
Therapeutic embolization through angiography catheters has become a standard of care, minimally-invasive method to reduce or eliminate unwanted flow of blood, with over 45,000 Medicare-funded procedures performed annually in the US1. During an embolization procedure, plugs, coils, small particles or liquids are deposited in blood vessels to obstruct flow at a designated anatomic site, with the device used chosen to address the arterial, arteriolar, or capillary level of obstruction desired. The applications of embolization are widespread and expanding, ranging from hemostasis for trauma-related hemorrhage, where preservation of tissue viability is desired, to inducing complete devascularization and infarction for malignant and benign tumors.
Although plugs and coils may be deposited precisely, transcatheter liquid and particle embolization has a critical weakness: flow-directed embolization relies on blood flow to carry the embolic liquid and particles into the target anatomy, and thus requires x-ray fluoroscopy imaging to assess the progress and endpoints of flow reduction. The use of fluoroscopy subjects patients and their treating physicians to DNA damage and the consequent dangers of radiation (skin injury, cataracts, infertility, dementia, adverse birth outcomes, cancer)2,3,4,5,6,7,8. The absorbed dose rate in the skin from the direct beam of a fluoroscopic x-ray system is typically between 0.02 and 0.05 Gy/min (2 and 5 rad/min), but may range from 0.01 to more than 0.5 Gy/min, depending on the mode in which the fluoroscopic equipment is operated and the size of the patient9. The potential for malignant degeneration increases directly with cumulative radiation dose, but even a small dose of radiation can cause DNA damage10. Also, the radiation-induced injury is dependent on a number of variables other than the cumulative dose, such as the rate of delivery of the radiation, the fractionation of the absorbed dose, and the age and characteristics of the person exposed. The Food and Drug Administration (FDA) has reports of occasional but, at times, severe radiation-induced burns to patients from fluoroscopically-guided procedures. In 1994, the FDA issued a report for physicians and other health care professionals warning about procedures that might result in injuries, with vascular embolization listed on the 3rd place among procedures typically involving extended fluoroscopic exposure time and thus posing an increased risk of causing harm9. Recent evidence confirms that interventional radiologists who are exposed to long-term low-dose ionizing radiation have increased genomic instability11.
Another critical weakness of particle embolization is off-target embolization—also known as nontarget embolization—the inadvertent delivery of embolic material to organs or vascular territories outside of the intended distribution (Fig. 1). Since the consequences of off-target embolization can be catastrophic (e.g., lost limb, organ necrosis, paralysis, or even death), it is of paramount importance to monitor embolic material delivery to ensure patient safety. Therefore, the risks of radiation exposure to patients and physicians are considered unavoidable. Despite the acceptance of the risks of radiation exposure, x-rays are an indirect and imperfect means of monitoring embolic delivery and avoiding off-target embolization. Most embolic material cannot be directly imaged via x-rays. Thus, embolic material is typically suspended in a radiopaque iodinated contrast medium so that its delivery can be monitored with real-time x-ray fluoroscopy12, but visualization remains qualitative and low in sensitivity. Moreover, use of iodinated contrast media is contraindicated in patients with impaired renal function or prior allergic reactions13. Even if visualization is adequate by x-ray fluoroscopy, the standard treatment endpoint of ‘heartbeats of stasis’ is subjective. This subjectivity may result in underembolization, leading to inadequate treatment response, or overembolization, increasing the risk of organ necrosis and reflux, leading to off-target deposition14.
Depiction of intended on-target and unintended off-target (nontarget) embolization. (A) Microcatheter tip in the right hepatic artery (blue arrow) allows selective delivery of embolic particles to a tumor in the right hepatic lobe. Particles are filling the tumor. A sensor electrode pair is depicted as two gold dots near the catheter tip. (B) As embolic particles occlude the tumor, there is slowing of blood flow and occasional reflux of particles and carrier fluids to the sensor, which changes electrochemical impedance at the sensor and provides a warning of impending off-target embolization. (C) If embolic particles continue to be injected despite increasing changes in electrochemical impedance, particles will reflux beyond the sensor and potentially reach other organs. (D) Hepatic ischemia (grey appearance of the liver), cholecystitis (red arrow), duodenal ulcers (yellow arrow), and gastric ulcers (purple arrow) may be consequences of off-target embolization in the vicinity of the liver.
The ionic characteristics of blood are tightly regulated within a narrow window by multiple physiologic systems to achieve homeostasis, resulting in predictable dielectric properties15,16. We hypothesized that fluids injected during catheter embolization, including nonionic iodinated contrast media and normal saline, may exhibit dielectric properties that are very different from that of blood, and these differences as assessed by electrochemical impedance measurement might therefore be used to distinguish the fluids in the setting of embolotherapy. In the present work, we hypothesized that using a custom fabricated catheter with embedded electrodes, electrochemical impedance spectroscopy (EIS) can be used to sense flow-related changes of these fluids as compared to blood around the catheter tip. These changes may be used to provide a real-time, radiation-free method of monitoring the endpoints and progress of embolization, including stasis, reflux, and persistent flow.
Methods
Ethics approval
The experiments involving human blood samples conducted in this study received ethical approval from the Stanford University Institutional Review Board (IRB-12597). The methodology adhered to the principles outlined in the Declaration of Helsinki and local regulations. All procedures were carried out in strict accordance with the approved guidelines. Informed consent was obtained from all individual participants involved in the study.
Measurement of electrochemical impedance
Electrochemical spectroscopy of fluids encountered at embolization was performed on two planar electrodes patterned on a precision printed circuit board (JLCPCB, Shenzen, China) to assess feasibility of distinguishing fluids based upon electrochemical impedance magnitude, and to select an excitation frequency for subsequent experiments. Fluids were applied to the printed circuit board (PCB) electrodes while measurement was performed using an impedance analyzer (Analog Discovery 2 with Impedance Analyzer add-on, Digilent, Pullman, WA) as the excitation frequency was swept from 1 kHz to 10 MHz in 1001 steps increasing exponentially. The electrodes were 0.254 mm wide, with 3.81 mm length exposed to applied fluid by a solder mask relief, and 0.3 mm spacing between electrodes parallel in their long axis (Fig. 2). The electrodes were gold-plated on nickel on top of copper. Measurements were performed using two-wire electrochemical impedance measurement technique. Replicates of 3 were performed with the same electrodes but with removal and replacement of fluid. Electrochemical impedance spectra are presented as averages of the replicates with standard deviation.
The following fluids were tested: 0.9% normal saline (Hospira, Lake Forest, IL), gadobenate dimeglumine gadolinium chelate contrast agent (Multihance, Bracco, Milan, Italy), iopamidol iodinated contrast medium (Isovue 300, Bracco, Monroe Township, NJ), iodixanol iodinated contrast medium (Visipaque 320, GE Healthcare, Chicago, IL), iohexol iodinated contrast medium (Omnipaque 300, GE Healthcare, Chicago, IL), 5% dextrose solution (Baxter, Lake Forest, IL), and human blood from a male volunteer. 5% dextrose solution (D5) is often used in angiography and embolization when a nonionic fluid is needed, for example, as a flush fluid for n-Butyl cyanoacrylate glue. The gadolinium chelate contrast agent was also tested since it is sometimes used in lieu of iodinated contrast agents for patients who have an allergy to iodinated contrast material.
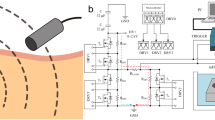
Catheter construction
Sensing catheters were created by attaching two 0.4 × 0.6 mm pieces of copper/nickel/gold contact pads as electrodes to a 4 French vertebral-shaped angiographic catheter (451-414 H0, Cordis, Santa Clara, CA) near the catheter tip, with leads of 42 gauge coaxial wire (Hitachi, Ashaway, RI) down the shaft of the catheter to a custom PCB adapter. The electrodes were spaced 4 mm apart and were 20 and 24 mm proximal to the catheter tip. Electrodes were encapsulated in silicone polymer (Si5240, Loctite, Westlake, OH) to provide electrical isolation. The catheter was covered in a Pebax jacket (Zeus Plastics, Spartanburg, SC) using lamination, and apertures at the electrodes were cut using a razor blade to allow contact with surrounding fluid (Fig. 3). After the addition of electrodes and an overlying jacket, the final largest diameter of the sensor catheter was 4.8 French (Fig. 3). A diagram of the detection circuitry is shown in Fig. 4.
Sensor catheter made with a 4 French angiographic catheter with two electrodes (arrows) and leads provided by coaxial cable (arrowhead). The separate black linear mark is from a marking pen to aid in the alignment of the electrodes with the pre-formed curvature of the catheter, for consistent construction.
In vitro characterization of impedance sensor catheters
Embolization phantom
Sensor catheters were characterized in an in vitro vessel model under pulsatile, artery-mimicking flow conditions to assess the feasibility of detecting electrochemical impedance differences between injected fluids under conditions of flow, stasis, and reflux. An embolization flow phantom was modeled with computer-aided design (CAD) to mimic the geometry and size of a large vessel with a smaller branch vessel to be selected and embolized (Fig. 5). The branch vessel diameter was 4.6 mm wide × 3 mm deep at its end, and the parent vessel was 20 mm wide and 3 mm deep. Inlet and outlet barb connectors were added proximally and distally. The 3 mm thick center construct was 3D printed in clear resin (Peopoly Clear, Shenzen, China) on a 3D printer (Peopoly Moai, Shenzen, China), laminated with two 1/8″ transparent acrylic sheets, and sealed with silicone (Si5056, Loctite, Westlake, OH). Inlet and outlet barbs were connected with 3/16″ inner diameter silicone tubing, and test fluid was transported with a centrifugal pump (BYT-7A015, Bayite, Shenzhen, China) programmed with an arterial waveform by a microcontroller (Feather ESP32-S2, Adafruit, New York, NY)17. Flow rates on each tubing segment were measured using a flow sensor (PLF2105, Posifa, San Jose, CA) read out by a microcontroller, with data saved via a serial terminal. As fluid injection was performed with the phantom on a transillumination stage, a video was recorded at 30 frames/second through a camera with timestamps for registration to impedance data.
3D-printed flow chamber for characterization of sensor catheter and endpoint detection. Direction of flow is left-to-right, as indicated. Locations of electrodes on the catheter are indicated by black arrows. The catheter tip is positioned in a branch vessel. An adjustable pipe clamp (not pictured) was used to limit the outflow of the branch vessel, simulating progressive embolization and stasis.
Measurement of flow, stasis, and reflux
The sensor catheter was positioned in the large vessel portion of the vessel phantom, with the tip engaged into the branch vessel and the sensor electrodes inserted approximately 1 cm into the branch vessel (Fig. 5). A blood-mimicking fluid was created by mixing 50 ml polyethylene glycol 400 (PEG400) with 50 ml distilled water, titrating electrochemical impedance magnitude at 100 kHz to 3 kΩ using 0.9% normal saline (typically 70 ml), and colored red with food coloring (McCormick, Hunt Valley, MD) to permit visualization under video recording. With the flow of this fluid provided by the pulsatile pump through the vessel phantom and around the sensor catheter, a nonionic solution (D5 solution) colored with blue food coloring (McCormick, Hunt Valley, MD) was injected through the catheter by hand injection until the fluids filled the side vessel and then refluxed. Electrochemical impedance magnitude and phase angle measurements were conducted at 100 kHz excitation frequency and 1.1 V excitation voltage, sampling at 10 Hz. Measurement circuitry was based upon an electrochemical and impedance front-end integrated circuit (AD5941, Analog Devices, Wilmington, MA). Timestamped video and electrical impedance measurements were saved and analyzed.
Results
Electrochemical impedance spectroscopy of fluids encountered at embolization
Electrochemical impedance spectroscopy of fluids encountered at embolization yielded impedance magnitude (|Z|) results spanning over 3 orders of magnitude, providing a dynamic range appropriate for distinguishing these fluids by EIS (Fig. 6). The electrochemical impedance of blood has been previously studied and is modeled as a resistance provided by plasma and capacitance provided by red blood cells18. 0.9% “normal” saline exhibits a much lower electrochemical impedance magnitude than blood, and exhibited the lowest electrochemical impedance magnitude of all the fluids tested that would be used during angiography and embolization. The electrochemical impedance magnitudes of the widely used iodinated contrast agents iodixanol, iopamidol, and iohexol were much higher than that of blood—5.500, 16.186, and 27.828 kΩ, respectively, versus 1.705 kΩ at 100 kHz. 5% dextrose solution was found to have higher electrochemical impedance magnitude (84.577 kΩ at 100 kHz) compared to the iodinated contrast agents, which although they are ‘nonionic’, have small amounts of ionic excipients including calcium chloride, sodium chloride, hydrochloric acid, sodium hydroxide, and tromethamine. Based upon these results for all fluids tested, 100 kHz was selected as a reasonable excitation frequency for subsequent real-time single-frequency electrochemical impedance measurements using the electrode-bearing catheter to maximize differences between fluid impedance magnitude, while staying within the limits of the AD5941 frequency generator. Moreover, at frequencies between 100 and 300 kHz the phase angle was closer to zero for all fluids, which allowed us to ignore the effect of phase angle in real-time measurements.
In the case of the more strongly ionic fluids saline, blood, and gadobenate dimeglumine, phase angle starts out more negative at the lower frequencies than nonionic fluids but continually increases towards zero over the entire measured frequency range. This likely reflects a more significant electrode polarization in ionic fluids, due to more charge carriers, more ionic mobility, and therefore a more pronounced capacitive behavior predominating at the lower frequency range. For some fluids such as the ‘nonionic’ iodinated contrast agents, the phase angle can start off negative and increase towards zero, possibly reflecting some electrode polarization due to small amounts of ionic content. Fluids with even lower ionic content such as dextrose solution demonstrate a phase angle closer to zero at low frequencies, which may reflect no significant electrode polarization at low frequencies due to a lack of charge carriers.
Impedance is a complex measurement composed of the real and imaginary components resistance and reactance, respectively, and shown in Fig. 6. Generally, the tested fluids are largely resistive without major contribution of reactance, and therefore the impedance magnitude and resistance plots appear very similar.
A blood-mimicking fluid made of PEG400, distilled water, and 0.9% sodium chloride solution (with electrochemical impedance magnitude at 100 kHz equivalent to blood) was created to assess the ability to resolve differences in injected fluids under pulsatile flow conditions. This was done for practical purposes, to avoid having to pump a large amount of anticoagulated blood through the vessel model, and because of the difficulty in visualizing flow changes of injected fluid compared to blood, which is opaque. Electrochemical impedance spectroscopy for the blood-mimicking fluid and blood is shown in Fig. 7. Both blood and the blood-mimicking fluid demonstrate frequency dependent decrease in impedance magnitude from 1 to 100 kHz, which likely reflects the decreasing electrode polarization effects with increasing frequency. As expected, beta dispersion is evident in blood at 100 kHz–10 MHz, but not in the blood-mimicking fluid due to the absence of blood cells. However, beta dispersion was not a required feature of the blood-mimicking fluid in the subsequent pulsatile flow experiments as electrochemical impedance magnitude was measured at a single frequency (100 kHz).
In vitro testing of electrochemical impedance sensor catheter
Using the 3D-printed flow chamber and the sensor catheter with electrodes positioned 1 cm into the branch vessel, the electrochemical impedance magnitude of the blood-mimicking fluid across the electrode gap was approximately 3.200 kΩ (Fig. 8). Note that this impedance magnitude is of course different than previously measured in Fig. 6 due to differences in electrodes on the catheter compared to the PCB electrodes. The real-time electrochemical impedance magnitude trace from the sensor catheter reflected the state of flow and occlusion environment of the catheterized vessel. Free flow within the branch vessel with absence of reflux during fluid injection without the constriction of the outflow resulted in no change in electrochemical impedance magnitude from baseline blood-mimicking fluid (Fig. 8A). With 50% occlusion of the branch vessel in which the sensor catheter was positioned, hand injection of D5 through the catheter led to reflux of solution along the sensor catheter that was detectable and corresponded with strength of injection and reflux of injected fluid (Fig. 8B–D). With near occlusion of the branch, injection of D5 at the same rate led to prompt reflux into the parent vessel and high impedance magnitude readings, equal to the impedance magnitude of 100% D5 solution, and prolonged stasis of fluid in the vessel. Whereas D5 solution had an impedance magnitude of 85 kΩ at 100 kHz by measurements shown in Fig. 6, the impedance magnitude of D5 by sensor catheter measurement in Fig. 8 was 7.053 kΩ. This could reflect the effect of the coaxial wire leads to the electrodes, the different electrode geometry, and the different measurement platform. Regardless, the technique was successful in resolving temporal differences between these fluids consistent with reflux and stasis. While the phase angle data mirrored the changes in impedance magnitude, an excitation frequency in the 100–300 kHz region was previously selected to minimize the effect of phase angle, allowing us to ignore the effect of phase angle and rely solely upon impedance magnitude for discriminating fluids adjacent to the catheter electrodes.
Optical and impedimetric detection of free flow, slow flow, and occlusion based upon reflux of injected fluid and washout. Occlusion is measured as percent flow rate decrease from baseline. Graphs of fluid electrochemical impedance magnitude changes over time depicted in the top row correspond with visual appearance of reflux at peak values shown in the bottom row. (A) Free flow of injected D5 fluid (blue) into the embolized branch vessel, resulting in no change in electrochemical impedance magnitude of blood substitute (red) with baseline electrochemical impedance magnitude of 3.174 kΩ. (B & C) Slow flow in the branch vessel is evident as a buildup of a column of injected D5 fluid at the catheter tip, reaching as far as the electrodes, leading to elevation in electrochemical impedance magnitude to 3.218, and 3.980 kΩ as D5 fluid progresses further up the catheter. (D) Severe reflux at risk of entering the parent vessel achieves of a peak electrochemical impedance magnitude of 5.847 kΩ. (E) Gross reflux into the parent vessel in the setting of branch vessel occlusion. Maximal electrochemical impedance magnitude rose to 7.053 kΩ from a baseline of 3.167 kΩ and required greater than 30 s for normalization.
Discussion
Different fluids encountered during embolization procedures exhibited vastly different electrochemical impedance magnitudes compared to blood, with notably large deviations from blood exhibited by 0.9% normal saline (an order of magnitude lower than blood) and by D5 solution (an order of magnitude higher than blood). These differences could potentially be exploited to use these physiologically benign fluids as negative and positive electrochemical impedance ‘contrast agents’, whereas neither is radiopaque and neither would be a tenable x-ray fluoroscopy contrast agent. Most contemporary iodinated contrast agents for intravascular delivery are nonionic, and therefore would be expected to also be excellent electrochemical impedance contrast agents, raising the possibility of multimodal contrast agents.
In an in vitro pulsatile flow branched vessel phantom and using a custom-prototyped angiographic catheter with embedded sensing electrodes, the reflux of injected fluids flowing retrogradely from the catheter tip resulted in detectable, reproducible, and quantifiable changes in electrochemical impedance magnitude compared to a blood-mimicking fluid. The absence of such events (Fig. 8A) indicated strong persistent forward flow of blood-mimicking fluid in the vessel without reflux, whereas very slow clearance by both visual and electrochemical impedance return to baseline was observed with 80% vessel occlusion (Fig. 8E). This is consistent with what is observed in the clinical setting of embolization, where initial particle delivery typically results in no reflux due to strong forward flow of blood, but as embolization nears completion there is slowing and stasis of injected contrast observed by x-ray as the distal arterial bed is occluded.
This work introduces a potential method to replace a low-sensitivity and potentially dangerous method—x-ray fluoroscopic monitoring—with a safer, label-free, and more precise technology for monitoring angiography and embolization.
In addition, the sampling rate of electrochemical impedance measurements (10 Hz or greater) is much higher than typical x-ray fluoroscopy imaging frame rates (2–6 frames/second). Minimizing the fluoroscopic frame rate during embolization can reduce radiation exposure19, but lower sampling rates may result in transient reflux events not being detected, which places the patient at risk of off-target embolization. Similarly, using a lower radiation dose rate or higher photon energy may decrease radiation dose but would further decrease sensitivity.
Our approach leverages the simplicity of electrochemical impedance spectroscopy, which only requires two electrodes. As a result, our approach is miniaturizable, inexpensive, and biocompatible.
Another potential major advantage of this technology is more precise fluid injection and achieving of embolization endpoints, which may translate to improved therapeutic accuracy. Currently, interventional radiologists may assess the endpoint for particulate embolization by “beats of stasis”, counting the number of heartbeats needed to clear a vessel of injected radiopaque contrast medium, but this is subject to multiple sources of variability and subjectivity, including patient factors such as tachycardia or bradycardia as well as overlapping structures (i.e. a bladder filled with excreted iodinated contrast agent). A quantitative, reproducible, and physiology-reflective technique, such as the measurement of electrochemical impedance, could potentially provide improved standardization of embolotherapy.
A limitation of the current study is the in vitro nature of the work. The vessel phantom used was composed of hard, inflexible walls within the 3D-printed portion as compared to actual human anatomy, which is typically elastic and may influence the rate at which injected fluids move compared to blood. A blood-mimicking fluid tailored to the electrochemical impedance magnitude of blood at a specific frequency, of course, lacks blood cells and ionic species that contribute to the complex dielectic properties of blood. In addition, the blood-mimicking fluid we used was not specifically tailored to mimic the flow properties of blood, so stagnation and backflow may be different in blood. The blood-mimicking fluid also cannot recapitulate clotting, and it’s therefore unclear to what extent a clot surrounding the catheter will affect performance, or potentially lead to false negative or false positive readings. Future work includes evaluation of in vivo performance and any possible effects of clotting and biofouling, but the current work is a critical proof of feasibility prior to moving to in vivo models.
A potential limitation of this technology for embolization monitoring is that it is tailored to detect stasis and reflux as a treatment endpoint in an end organ with a dendritic capillary system. Forward shunting distal to the sampled vascular territory (e.g., arteriovenous shunting) may be difficult to detect. Sampling error may also occur depending on the location of electrodes relative to intravascular flow patterns, which can be influenced by vessel length, size, and curvature. Future work will evaluate the effect of catheter position within the vessel and different electrode geometries upon baseline impedance magnitude and detection sensitivity.
In conclusion, the dielectric properties of fluids encountered during angiography and embolization as assessed by electrochemical impedance spectroscopy vary widely, and these properties can be measured via catheters bearing electrodes under flow conditions that inform the status of flow in an in vitro embolization model. This represents an opportunity for using nontoxic, non-radiopaque fluids as impedimetric contrast agents at angiography and embolization. Ongoing development holds promise to yield a more accurate, sensitive, and quantitative method to measure blood flow, embolization progress, and stasis without the use of ionizing radiation.
Data availability
Data from this manuscript is available upon request from the corresponding author.
References
Topper, S. R. et al. Trends in percutaneous embolization procedures by radiologists and other specialists. J. Vasc. Interv. Radiol. 31, 961–966. https://doi.org/10.1016/j.jvir.2020.01.031 (2020).
Vano, E., Gonzalez, L., Fernández, J. M. & Haskal, Z. J. Eye lens exposure to radiation in interventional suites: Caution is warranted. Radiology 248, 945–953. https://doi.org/10.1148/radiol.2482071800 (2008).
Klein, L. W. et al. Occupational health hazards in the interventional laboratory: Time for a safer environment. J. Vasc. Interv. Radiol. 20, S278-283. https://doi.org/10.1016/j.jvir.2009.04.027 (2009).
Vano, E., Kleiman, N. J., Duran, A., Romano-Miller, M. & Rehani, M. M. Radiation-associated lens opacities in catheterization personnel: Results of a survey and direct assessments. J. Vasc. Interv. Radiol. 24, 197–204. https://doi.org/10.1016/j.jvir.2012.10.016 (2013).
Srivastava, T. et al. Exposure to ionizing radiation and risk of dementia: A systematic review and meta-analysis. Radiat. Res. 199, 490–505. https://doi.org/10.1667/rade-22-00153.1 (2023).
Frangione, B., Hinton, P. & Villeneuve, P. J. Low-dose ionizing radiation and adverse birth outcomes: A systematic review and meta-analysis. Int. Arch. Occupation Environ. Health 96, 77–92. https://doi.org/10.1007/s00420-022-01911-2 (2023).
Borrego, D., Yoder, C., Balter, S. & Kitahara, C. M. Collar badge lens dose equivalent values among United States physicians performing fluoroscopically guided interventional procedures. J. Vasc. Interv. Radiol. 33, 219-224.e212. https://doi.org/10.1016/j.jvir.2021.10.027 (2022).
Ko, S. et al. Health effects from occupational radiation exposure among fluoroscopy-guided interventional medical workers: A systematic review. J. Vasc. Interv. Radiol. 29, 353–366. https://doi.org/10.1016/j.jvir.2017.10.008 (2018).
Important information for physicians and other health care professionals: Avoidance of serious x-ray-induced skin injuries to patients during fluoroscopically-guided procedures. (Food and Drug Administration, 1994).
Health Effects of Exposure to Low Levels of Ionizing Radiation: Beir V. in National Research Council (US) Committee on the Biological Effects of Ionizing Radiation (BEIR V), 25032334 (Washington (DC), National Academies Press (US), 1990).
Kochanova, D. et al. Effects of low-dose ionizing radiation on genomic instability in interventional radiology workers. Sci. Rep. 13, 15525. https://doi.org/10.1038/s41598-023-42139-5 (2023).
Lewandowski, R. J., Geschwind, J. F., Liapi, E. & Salem, R. Transcatheter intraarterial therapies: Rationale and overview. Radiology 259, 641–657. https://doi.org/10.1148/radiol.11081489 (2011).
Wang, C., et al. American College of Radiology Manual on Contrast Media. American College of Radiology, Reston, VA, (2021).
Schirf, B. E., Vogelzang, R. L. & Chrisman, H. B. Complications of uterine fibroid embolization. Semin. Interv. Radiol. 23, 143–149. https://doi.org/10.1055/s-2006-941444 (2006).
Bernal, A., Zafra, M. A., Simón, M. J. & Mahía, J. Sodium homeostasis, a balance necessary for life. Nutrients https://doi.org/10.3390/nu15020395 (2023).
Gabriel, S., Lau, R. W. & Gabriel, C. The dielectric properties of biological tissues: III. Parametric models for the dielectric spectrum of tissues. Phys. Med. Biol. 41, 2271–2293. https://doi.org/10.1088/0031-9155/41/11/003 (1996).
Herwald, S. E., Sze, D. Y., Ennis, D. B. & Vezeridis, A. M. Design and implementation of a cost-effective, open-source, and programmable pulsatile flow system. HardwareX https://doi.org/10.1016/j.ohx.2024.e00561 (2024).
Zhao, T. X. Electrical impedance and haematocrit of human blood with various anticoagulants. Physiol. Meas 14, 299–307. https://doi.org/10.1088/0967-3334/14/3/008 (1993).
Sapoval, M. et al. Uterine artery embolization for leiomyomata: Optimization of the radiation dose to the patient using a flat-panel detector angiographic suite. Cardiovasc. Interv. Radiol. 33, 949–954. https://doi.org/10.1007/s00270-010-9795-0 (2010).
Acknowledgements
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number KL2TR003143. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors thank Dr. Anna Romanowska-Pawliczek for valuable editorial input.
Funding
National Center for Advancing Translational Sciences, KL2TR003143.
Author information
Authors and Affiliations
Contributions
A.M.V. conceived and designed the work, collected the data, performed the analysis, and wrote the paper. As the corresponding author, A.M.V. also coordinated the research project and is the primary point of contact for the manuscript. S.E.H. contributed to the design of the work and analysis, assisted in data collection, and critically revised the manuscript for important intellectual content. K-H.P. made substantial contributions to the conception of the work, assisted in data collection, and reviewed the manuscript. B.L.D. contributed to the design of the work and analysis, contributed to the interpretation of the results, and provided critical revision of the manuscript for important intellectual content. D.Y.S. assisted in formulating the research question, contributed to the design of the methodology, and critically revised the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
This work is subject of a full patent application to the US Patent and Trademark Office (inventors including AMV and BLD on behalf of Stanford University), as well as an additional provisional patent disclosure (inventors including AMV, SEH, BLD, and DYS on behalf of Stanford University). KHP has no competing interests to disclose relevant to the current manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Vezeridis, A.M., Herwald, S.E., Paik, KH. et al. Label-free monitoring of embolotherapy via catheter electrochemical impedance spectroscopy. Sci Rep 14, 21310 (2024). https://doi.org/10.1038/s41598-024-71835-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71835-z
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.