Abstract
This study aims to evaluate the applicability of the high-resolution WaveFront Phase Imaging Sensor (WFPI) in eyes with Fuchs’ Endothelial Corneal Dystrophy (FECD) through qualitative and quantitative analysis using a custom-designed Automatic Guttae Detection Method (AGDM). The ocular phase was measured using the t\(\cdot\)eyede aberrometer and then was processed to obtain its High-Pass Filter Map (HPFM). The subjects were pathological and healthy patients from the Fundación Jiménez-Díaz Hospital (Madrid, Spain). The AGDM was developed and applied in pupils with 3 and 5 mm of diameter. A set of metrics were extracted and evaluated like the Root-Mean-Square error (RMS), Number of guttae, Guttae Area, and Area of Delaunay Triangulation (DT). Finally, a Support Vector Machine (SVM) model was trained to classify between pathological and healthy eyes. Quantitatively, the HPFM reveals a dark spots pattern according to the ophthalmologist’s description of the slit-lamp examination of guttae distribution. There were significant statistical differences in all the metrics when FECD and Healthy groups were compared using the same pupil size; but comparing both pupil sizes for the same group there were significant differences in most of the variables. This sensor is a value tool to objectively diagnose and monitor this pathology through wavefront phase changes.
Similar content being viewed by others
Introduction
Fuchs’ Endothelial Corneal Dystrophy (FECD) is a bilateral, asymmetric, and low progression corneal disease characterized by morphologic changes in the endothelial cells (pleomorphism or polymegatism), the presence of guttae (excrescences from the Descemet Membrane) as its main hallmark, and edema in the severe stages1,2,3. The ophthalmologist Ernst Fuchs was the first to observe central corneal clouding in 1910th, who described this event as epithelial dystrophy4. Later studies based on this observation found that the endothelium had the predominant role because of the referred guttae1,5,6. This disease usually appears at the age of fifty years, and its progression will take 10-20 years, being more common in females than in males7,8,9. The literature states that it is associated with inherence and other ocular conditions such as glaucoma, keratoconus, or keratitis, while the prevalence varies among endemic populations, being higher in Caucasians than in the Asian population8,10. Although in mild stages the treatment is hypertonicity drops or pomade to reduce the appearance of edema, corneal transplantation is the procedure that restores the correct vision and reduces gradual complications7.
The usual exploration of this disease is performed using the slit-lamp to evaluate the status of the cornea (the presence of guttae, bullae, or corneal scarring). This device is employed to gradate the severity of the FECD by stages based on Krachmer’s classification regarding the number of guttae observed and their confluence, such as the presence of edema in the most severe stage11,12, as can be seen in Figure 2 of the Matthaei’s work13. Nevertheless, this classification depends on the subjective physician’s criteria and the illumination method. This fact decreases the diagnosis accuracy and viability, and highlights the importance of additional objective techniques to determine severity12,14,15. Several authors expressed the relevance of a quantitative observation of guttae distribution due to its benefit in the diagnosis and prognostic purposes, the effect of guttae on the quality of vision, and determining surgical indications for endothelial surgery in eyes with mild FECD16,17. Therefore, many studies have quantitatively assessed the distribution of guttae using slit-lamp images15,18, applying imaging treatment and morphological segmentation algorithms.
Additionally, another instrument commonly used in clinical practice for the evaluation of corneal status with this pathology is the specular microscope, which is also used to assess the endothelial cell morphology and guttae influence3,8,13, acquiring images of the endothelial cells mosaic of a concrete area of the cornea of 0.2 x 0.5 mm19. Many studies have quantitatively assessed the distribution of guttae using these sections16,17,20, but, when the disease is in its moderate stage, the guttae are so confluent that the specular microscope images are not valid.
Furthermore, some of these works enhance the relevance of guttae distribution on the quality of vision17,21, which is being explored through ocular aberrations22,23,24. Consequently, these studies reveal increased trefoil, coma, and high-order aberrations in FECD eyes using the estimated values from Pentacam elevation results (anterior and posterior corneal aberrations). Still, they report that the sources of the posterior corneal surface are unknown and are not able to distinguish whether guttae are the cause of this25. In the current literature, studies on aberrations in the FECD treat the phase only using Zernike polynomials (up to 6th or 8th order), and most are reconstructed from elevation data and not from direct phase measurements, leaving details hidden behind these orders that may be of utmost importance.
Recently, studies have been published using the WaveFront Phase Imaging (WFPI) sensor to compare keratoconic eyes with healthy eyes, which, apart from showing good reliability to obtain Zernike coefficients of up to 10th order26, is also able to discover in the ocular phase characteristic structures of these pathological eyes (banding patterns) that are not appreciated in healthy eyes, also analyzed quantitatively27. Hence, evaluating different ocular conditions is motivated because of its high lateral resolution (8.55 \(\upmu\)m), and its reproducibility and repeatability already demonstrated against the gold-standard Hartmann-Shack28. Also, the technique implemented in this device has been validated in other sectors such as semiconductor metrology29, optical quality assessment30, and phase microscopy applied to biological samples31. All these fields require a high measurement precision that this sensor meets since it is capable of measuring Optical Path Differences (OPD) of a few nanometers caused by manufacturing defects or small refractive index changes on the same structure. Therefore, FECD is a clear candidate to be evaluated with this high-resolution sensor to unravel questions about how guttae affect the ocular wavefront phase.
The aim of this work is to objectively evaluate the applicability of the mentioned sensor using a custom-designed Automatic Guttae Detection Method (AGDM) capable of distinguishing between healthy and pathological eyes with FECD using phase information (concretely using the high-pass filter map).
Material and methods
Device: t\(\cdot\)eyede aberrometer
In this study, the ocular phase is measured using the WFPI sensor (Wooptix S.L., La Laguna, Tenerife, Spain) implemented in the t\(\cdot\)eyede aberrometer thoroughly described in previous works28,32,33. The sensor captures two intensity images shifted at the same distance (6.35 mm) on both sides of the conjugated pupil plane to recover the ocular phase, as shown in Fig. 1. The main advantage of this wavefront phase sensor is its 8.55 \(\upmu\)m of lateral resolution obtained according to the number of pixels of a Charged-coupled device (CCD) sensor, which are converted into reliable measurement points. The system has also been optimized to prevent spurious light and speckle from reaching the sensor, and the numerous iterations performed by the algorithm make the phase recovery resistant to noise28,31.
This device uses a Superluminescent Diode (SLD) as a light source with a wavelength of 780 nm and an exposure time in the pupil plane of 30 ms with a power of 0.78 mW (value under the security limit of the ANSI rules). A Badal system is included to correct patient defocus over a range of − 10.00 to +10.00 D. Five measurements are taken with a few seconds of difference during the phase capture session, so the patient must look at the Maltese Cross used as the fixation target and may rest on the chin-rest provided on the set-up. Examples of an intensity image of both healthy and FECD eyes were shown in Fig. 2.
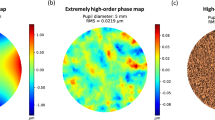
Once the measurement is completed, the intensity images are processed using the WFPI software, which recovers the ocular phase of the patient’s natural pupil with high resolution. This process has been detailed (and exemplified) in the previous study with healthy eyes and with keratoconus27. In summary, from this phase is extracted a phase map composed of the first 65th Zernike’s polynomials without the coefficients of piston, tip/tilt, and defocus (this map is considered as Low-Order Map). Moreover, the rest of the phase displayed (from the 66th coefficient and beyond) is what we name the Extremely High-Order Map because this phase map contains the high-frequencies. Then, a Gaussian high-pass filter with a cut-off frequency of 25 \(\upmu\)m is applied to the whole raw phase (the same filter is used for all eyes to ensure comparability), obtaining hence the High-Pass Filter Map (HPFM). This study is based on the latter map, as it represents the OPD caused by small ocular structures not visible due to the main wavefront change due to low-order ocular aberrations.
Patients and measurement protocol
This study includes both healthy (control group) and FECD eyes (pathological group) according to five ophthalmologists. The pathological group is composed of: isolated FECD, FECD with cataracts, and FECD with Monofocal Intraocular Lens (IOL) cases. Dilated and undilated pupils were measured, in case of dilated pupils, it was on purpose for their previous ophthalmologic consultation and not for the t\(\cdot\)eyede study. The measurements were performed at the Hospital Universitario Fundación Jiménez Díaz (Madrid, Spain). Its Institutional Review Board approved the study protocol that complied with the tenets of the Declaration of Helsinki. Informed consent was voluntarily obtained from the subjects after the explanation of the nature of the study previous t\(\cdot\)eyede measurements. The exclusion criteria were presenting other ocular pathologies, being under the legal age, being currently pregnant or breastfeeding, or participating in another interventional study within 30 days before the start of this study.
To include patients within this study, ophthalmologists relied on slit lamp examination and specular microscope sections. With the slit lamp they determined whether an eye was pathological or not according to the appearance of guttae and their distribution along the cornea, and if so, some ophthalmologists graded its severity according to Krachmer’s classification. Also, they evaluated the state of the corneal endothelium with the specular microscope, where, through its algorithm, the number of endothelial cells that remain is counted (as an example of this algorithm is shown in Fig. 3b). Since the Hospital Fundación Jiménez Díaz is a clinic external to Wooptix, what it was able to provide to the company for performing this study were the slit lamp examination descriptions and some specular microscope images (examples of different cases with the stages assigned by the ophthalmologists presented in Fig. 3).
The control group is formed by 43 healthy eyes of 25 patients (range age: 27–56 years; Gender: 11 Males, 14 Females) and the pathological group has 204 eyes of 120 patients (range age: 40–93 years; Gender: 39 Males, 81 Females). We do not consider any other demographic data relevant to this study.
Automatic Guttae detection method
As all the eyes diagnosed with FECD by the ophthalmologist presented a dark spots pattern in the HPFM, in order to objectivate the evaluation of this disease using the WFPI technique, we have developed an Automatic Detection Method based on image processing by morphological segmentation. Due to the number of images per eye (up to five valid images in the same session) and the large number of guttae per image, this method was made up with three objectives in mind: that the number and location of guttae detected for an eye should coincide in the different measures, that the method should work for the several levels of evolution of the disease, and that it should not require excessive parameters whose fine-tuning would affect the repeatability of the measurements.
The flow of operations of the method and the parameters that govern it are shown in the diagram in Fig. 4. It depends on several fixed internal parameters but only on two external modifiable ones, Minimum Brightness and CrossCorrelation Threshold. The entire experiment was performed on all images and for a wide range of combinations of both parameters. Those parameters that gave the best results were retained. In this manner, the method is self-adjusted to the depth absolute values that t\(\cdot\)eyede provides without user intervention.
The first part of the method consists of cutting the pupil diameter to 5 and/or 3 mm, as well as applying masks to cover unwanted reflections that may affect the phase representation in the HPFM, called preprocessing because it is prior to the image processing performed by the algorithm. The next step consists of thresholding the input image to select the pixels with an intensity lower than the self-adjusted parameter Minimum Brightness. Those pixels are then segmented into neighboring zones, from which the area is calculated. Zones whose areas lie between the 10th and 40th percentiles are clearly considered guttae. A gutta profile model is formed for the eye in consideration by averaging the areas that have passed the filters described up to this point. Then, a normalized cross-correlation is performed between the gutta model and the eye image. The cross-correlation output is thresholded with the second self-adjusted parameter of the method: CrossCorrelation Treshold. Finally, a non-maximal suppression is applied to keep the central location of each detected gutta.
Figure 5 shows the different stages of the method. Firstly, Fig. 5a is an input eye image with the region of interest surrounded by a red rectangle (subsequently analyzed in detail), whereas Fig. 5b ghts those zones whose intensity is superior to the Minimum Brightness. Figure 5c shows the clear guttae candidates. Figure 5d represents the gutta shape model. Figure 5e shows the output of the normalized cross-correlation of the eye image with the gutta model and highlights the zones that exceed the parameter CrossCorrelation Threshold. Notice that depending on that threshold, the number of final guttae can be greater or lower than the clear guttae candidates. As previously discussed, the method self-adjusted this parameter. Finally, Fig. 5f reveals each peak that succeeds in the non-maximal values suppression, that is, the final location of each gutta center. Hence, the surroundings of the guttae centers are analyzed to extract the metrics reported below.
Metrics description and analysis
A set of metrics is extracted to quantitatively compare healthy and pathological eyes, as well as to train an automatic binary classification model between both groups using pupil sizes of 3 and 5 mm. The calculated metrics are: the Root Mean Square error (RMS) (mrad) considering the values inside the pupil of the HPFM, the Number of Guttae Detected (accounts), Guttae Density (calculated as the number of guttae per \({mm^{2}}\)), Mean Guttae Diameter \((\mu m)\), Mean Guttae Area \(({\mu m^{2}})\), OPD Height (OPDH) (mrad) considered as the difference between the highest and the lowest point of the guttae profile, and Phase Roughness (mrad) calculated by equation 1 based on the Verma’s work equation to obtaining the roughness in ablation in corneas with Laser Vision Correction34.
In addition, Delaunay Triangulation (DT) is obtained regarding the guttae position, extracting as quantitative metrics the mean triangle area and the mean triangle area calculated after applying the Convex Hull algorithm. This mathematical tool consists of constructing triangles from a set of points (in this case, the located position of guttae) where the circumcircle of each triangle that forms the mesh must not contain any vertex of another triangle35. Therefore, when guttae are distant and scattered, the triangle area would increase (like in a healthy eye) whereas, if guttae are agglomerated (like in a FECD eye), the triangle area would decrease due to the small distance between guttae. Moreover, the Convex Hull algorithm is implemented to not ponder those external points of the map considered as false negative values.
Once the values have been obtained, the results of both groups and both sizes of students are statistically compared. For this purpose, first the Shapiro-Wilk test is used to assess the normality of each sample, and then the Mann-Whitney U test is used in case any of the samples do not meet the normality distribution. Statistical analysis was performed using the package scipy.stats (v.1.7.1) of Python (v. 3.9).
Automatic binary classifier model
As a further consideration, this work proposes the Support Vector Machine (SVM) tool from Matlab (v.R2022b) to create an automatic classifier to distinguish between healthy and pathological eyes. This method is applied to both pupil diameter analyses.
Previously, in order to avoid redundant information from the nine previous variables that can correlate with each other (like Mean Guttae Diameter and Mean Guttae Area), the Principal Component Analysis (PCA) was applied to generate a new set of variables (Principal Components(PC)) as a result of linear and orthogonal combinations of the original variables based on finding the maximum variance among the data set36,37, so the principal components will be ordered according to the largest amount of variance among the initial metrics. The number of PC is equal to that of the original set, and each eye (input) would be characterized by the scores of each PC. In this study, the SVM model’s behavior is evaluated using three and five Principal Components.
With the new representation of the sample, to train the SVM model, it is necessary to enter a training data set (composed of the 50% of each group) where each input was labeled as healthy or pathological (ophthalmologist criterion). As at least five measures per eye were taken during the measurement session, only one measure is randomly chosen to avoid the same eye appearing in both sets. Once the model is trained, it is applied to a test data set (the remaining 50%) to be the model itself which classifies each new input as healthy or pathological38,39.
Then, to compare if there are statistical differences between both classifications for the same eye, McNemar’s test is used. That is a statistical test for paired nominal data (the same eye has two independent classifications with the options: Healthy or FECD) where its null hypothesis states that the performance of both classifiers is equal (accepted when the p-value is higher than 0.05)40; also it is recommended to use when the machine learning model is only once fitted, like in the model example presented41. In addition, taking doctors’ diagnoses as the reference classification, to quantify the model hits and misses, the subsequent evaluation metrics for binary classification are obtained according to the equations presented in Rainio’s work42: Accuracy, defined as the proportion of correctly classified instances by the SVM model in the set of all the instances; Sensitivity, defined as the proportion of the truely positive instances from those cases that are pathological according to the doctors’ criteria; and Precision, defined as the instances classified as positive from those cases that are predicted as pathological by the SVM model.
Results
Qualitative evaluation of the Fuchs’ endothelial corneal dystrophy
Since part of the pathological eyes has not been graded into stages by ophthalmologists, it has been decided to present examples of Healthy eyes and FECD with and without severity grade in Fig. 6 to demonstrate the agreement between what the ophthalmologists described in their slit-lamp evaluations with what is observed in the HPFM, expressing both comparisons below. Figure 6a is a healthy eye with no remarkable event according to the ophthalmologist and any characteristic pattern in the HPFM; Fig. 6b is an isolated FECD eye with grade 2 and inferior-paracentral guttae (2 mm area) as reported by the doctor, also in the HPFM slight agglomeration of dark spots in the 2 mm below the center appear; Fig. 6c corresponds to an isolated FECD eye with grade 5 (any other comment from the ophthalmologist), while in the HPFM there are dark spots concentrated in aproximately the whole pupil (less frequent at the lower edge); Fig. 6d is another isolated FECD case with grade 5 with guttae in central 4–5 mm according to the slit-lamp exploration, as well as in the HPFM there are dark spots extended over approximately the entire pupil (edges less affected); Fig. 6e is a FECD eye with undefined grade and IOL, but the doctors referred central guttae, as can be seen in the HPFM, where dark spots are extended in the centre of the pupil with a zone of slight roughness change (right side) surrounded by the dark spots; at last, Fig. 6f is a FECD eye with undefined grade and incipient cataract without any comment from the ophthalmologist, but in the HPFM there are dark spots extended in the centre of the pupil with a zone of moderate roughness change (right side) surrounded by the dark spots.
HPFM of eyes regarding the opthtalmologist criteria: (a) Healthy left eye (OS), (b) FECD grade 2 right eye (OD), (c) FECD grade 5 left eye, (d) FECD grade 5 right eye, (e) FECD left eye (undefined grade) with Monocular Intraocular Lens, (f) FECD left eye (undefined grade) with incipient nuclear cataract. Representation with the patient’s natural pupil.
Furthermore, these maps can be directly comparable to those slit-lamp captures shown in Figure 2 of Matthaei and collegues13, and in slit-lamp retroilluminated images from other studies15,18,43.
Metrics results and comparisons
Regarding the metrics descriptors, their results are presented in Table 1. The values are obtained for both groups (Healthy and FECD) for both pupil diameter analyses (3 and 5 mm). The study of 3 mm includes 247 eyes (43 Healthy and 204 FECD), while the 5 mm analysis has 149 eyes (39 Healthy and 110 FECD). In this last case, the sample is lower because the patient’s natural pupil is smaller than such diameter.
The samples have been evaluated statistically using the Shapiro-Wilk test to check their normality distribution. As most cases presented a p-value lower than 0.05, the hypothesis that the samples tend to the normal distribution is rejected, and the U Mann-Whitney test is applied to compare them between groups and pupil diameters. When both groups are compared using the same pupil diameter, the p-value is lower than 0.05 for all the metrics, indicating significant statistical differences between healthy and pathological eyes in both pupil diameters. Otherwise, when different pupil diameters are compared for the same group, the statistical differences are represented in Table 1 with the * mark.
In addition, to show the stability of the phase in the same capture session (five measures with a few seconds of difference), we add an example of a healthy eye, two FECD eyes at different stages of the disease, an one ungraded FECD eye according to the ophthalmologist criteria. Therefore, three HPFM of each eye are presented in Fig. 7, and Table 2 quantitatively demonstrates the variation between the different measurements of the same eye in the same session.
Automatic binary classifier model evaluation
An example of the PCA results comparing the first three dimensions using the pupil diameter of 3 mm is represented in Fig. 8. In this case, the first principal component is mostly influenced by the results obtained with the metrics of Delaunay Triangulation (associated with the guttae distribution), the second principal component with the metric of Mean Guttae Area, and the third component is mostly influenced by the metric Number of Guttae Detected.
Regarding the statistical comparison between both classifications applying McNemar’s test, the p-values obtained for the 3 mm pupil size were 0.67 and 0.51 using 3 and 5 PCs respectively, meanwhile for the 5 mm pupil size using 3 PCs was 0.56 and 0.66 with the 5 PCs. Then, the null hypothesis is accepted for all the cases, indicating that there are no statistical differences between both classifications.
On the other hand, the evaluation metrics of the SVM model have also been calculated for these 4 analyses considering the physicians’ labels as true. The accuracy, sensitivity, and precision results for the 3 mm pupil analysis with 3 PCs were: 92.8%, 96.9%, and 94.8% respectively, meanwhile using 5 PCs the results were: 92.8%, 96.1%, and 95.2%. Also, for the 5 mm pupil analysis with 3 PCs the values were: 90.2%, 94.8%, and 92.1% respectively, and 90.7%, 94.8%, and 92.7% using the 5 PCs.
Discussions
This study illustrates the applicability of the WFPI Sensor to evaluate Fuchs’ Endothelial Dystrophy by means of a qualitative and quantitative analysis using metrics extracted from the ocular wavefront phase. The usefulness of the current sensor demonstrates the relevance of considering the phase beyond extreme orders to uncover minor details such as guttae. Reviewing the literature, no previous aberrometer has revealed a pattern like these from the wavefront phase, being one of their main disadvantages representing the phase up to the 10th order of Zernike’s polynomials as well as recalculating the corneal wavefront from elevation data.
First of all, examples of a healthy and FECD eyes HPFM with different corneal status according to the ophthalmologist’s description are shown in Fig. 6. In these cases, there is concordance between what is described by the ophthalmologist in his examination using the slit lamp (distribution of guttae) with the pattern of dots observed in the HPFM. Likewise, these patterns are similar to the distribution of guttae shown by other authors with slit-lamp15,18,43, and as clear examples are the comparisons between our maps (d) and (f) in Fig. 6 with the slit lamp images (c) and (e) in Figure 2 of Matthaei’s work respectively. In the first example, the guttae are agglomerated in the center of the pupil but do not exist in the periphery; while in the second case there is an area of changing roughness surrounded by guttae that Matthaei describes as a bullae. On the other hand, given the novelty of the sensor and its applicability in ophthalmology, but previously validated in artificial and human eyes27,28, it has been decided to show examples of stability of the wavefront phase measurement between 5 captures (taken consecutively a few seconds apart with blinks in between) to demonstrate that it is not random noise generated by the sensor or type or fluctuating structures such as tear deposits or vacuoles due to their variable position (Fig. 7). We have also calculated the mean and standard deviation of some metrics between the measurements for each eye, showing that the standard deviation is not critical (Table 2).
Regarding the statistical differences obtained in the metrics extracted from the Automatic Guttae Detection Method, we can hypothesize that: the metric Number of Guttae Detected increments when the pupil diameter increases, but the metric Guttae Density does not change in the Healthy group, indicating that in this group the regions detected are not dependent of the pupil diameter while in the FECD group the value was slightly decreased due to the highest concentration of guttae in the central region that tends to spread toward the periphery, as stated in all reviews1,3,7,8,9. The metrics Mean Guttae Diameter and Mean Guttae Area are statistically different between healthy and pathological eyes independently of pupil diameter, but, for the same group, the value remains regardless of pupil size, indicating that each group has its own characteristics. In this case, although no literature characterizes these parameters with wavefront phase information, these results can be compared with other studies that use different methods to calculate it: Soh and colleagues obtained a mean value of guttae size of 407 ± 155 \(\upmu\)m218, being closer to ours obtained in the healthy group rather than in the pathological group, and Dong and colleagues reported guttae diameters in a range of 20 to 60 \(\upmu\)m44 in agreement with our values obtained in both groups. Concerning the OPDH metric, there were statistical differences in the FECD group expressing that it decreases when the external area is evaluated, launching the hypothesis that this could be associated with the dystrophy severity, while this metric remains constant in healthy eyes between different pupil sizes. The Phase Roughness does not change in any of the groups despite pupil size but differs from group to group, as was also illustrated in Vaitinadapoulé’s work, demonstrating that the roughness increases in the FECD eyes against the healthy ones measuring corneal nanotopography by chromatic confocal microscopy45. The results with DT metric match with those of the Guttae Density, indicating that the guttae distribution changes tend to spread along the pupil (explaining the triangle area increment) in the FECD group meanwhile the distribution is uniform in healthy eyes. Otherwise, when Convex Hull method is applied, the DT mean area illustrates that removing external points affects the Healthy group (increasing the triangle area) but not the FECD eyes due to the high amount of guttae also in the periphery because these spots are not considered as outsiders. Nevertheless, due to the different methodologies of acquisition, the quantitative comparisons between works are not completely reliable, only tentative.
After this detailed analysis, the usability of the automatic method is supported by the number of metrics that are easy to interpret and are distinguishable between healthy and pathological eyes. Moreover, this method is able to directly acquire more features than conventional images, such as phase roughness. This parameter should be evaluated in more detail in future studies, as it has been seen in some pathological eyes as there is a change of roughness in certain regions, so it should be evaluated individually as it could be key in the early detection of the appearance of edema in mild cases that could be missed in slit lamp examination. There are already studies focused on this aspect using the Anterior Segment Spectral Domain Optical Coherence Tomography (OCT) technique46, where the presence of edema at different stages of the pathology is mainly evaluated by means of a specific number of corneal transversal sections. But in these cases, the distribution of the guttae is not relevant, which should be taken into account since it has been shown the relation between the guttae distribution and corneal edema47. Moreover, Soh and colleagues in their Figure 418 represent the area with greater accumulation of guttae regarding the laterality of the eye, being clearly superior in the inferotemporal pupil zone, which agrees with the regions where the HPFM changes the roughness in right eyes (on the left side of the map), and left eyes (on the right side of the map), like are exemplified in Fig. 6e, f. With this in mind, the device presented in this study could quantitatively monitor pathology over time based on the distribution of guttae and can assess when this change in roughness occurs.
Notice that throughout the paper we have been talking about the Optical Path Difference Height because we want to make it clear that we are not measuring the morphological height or depth of these per se, but the phase change they produce. That justifies the scale with which the HPFM is represented, together with the fact that when recovering the phase by measuring the intensity propagation, the details that are below the axis resolution of the system (not the lateral resolution) are mitigated but not disappeared, as vanDam refers in his work48.
Concerning the PCA and the SVM model, the example ploted in the Fig. 8 with the first 3 PCs for 3 mm pupil diameter shows that both groups are in two separate regions, and the principal components that distinguish between both groups are obtained from the metrics that would be easily interpreted by ophthalmologists: guttae distribution, guttae area, and regions detected. The pathologic group tends to be more crowded than the healthy group. Given the clear distribution of values of both groups, we have chosen to perform the automatic binary classification using the SVM method, thinking that it would be the best fit since it generates a plane that tries to separate both groups with the greatest possible difference. This model has achieved a sensitivity of approximately 95%, and there is no difference between its classification and that of the ophthalmologists, being more sensitive than other works with 91% using only images to train the classifier model49. However, the remaining percentage would be influenced by the fact that each eye has been evaluated by a single ophthalmologist, having participated five in total. So, the examination and diagnosis depend on the experience of each one, where it may be the case that incipient cases of FECD can be classified as healthy (False Negatives) or vice versa (False Positives). Also, we should consider that the recovered phase is from all the ocular media and not just from the cornea. Hence, particles, vacuoles, or pigment could be detected by the automatic method as guttae in a healthy eye, labeling it as FECD (False Positives). Moreover, the pathological sample includes patients with cataracts that could hide guttae where both media overlap and the method would classify an eye with FECD as a healthy eye (False Negatives).
On the other hand, this automatic classifier is trained only using metrics, but we are aware that these accuracy results can be improved by applying algorithms that allow training neural networks combining the results of the metrics together with the HPFM, and that is also able to distinguish between different pathologies by taking advantage of the results of previous studies, as other authors have already achieved using only images50. Despite this, the purpose of this study is to present the automatic gutta detection method, its development, and its ability to obtain objective results, leaving in the background the initial proposal of a binary classification model.
In summary, the objective quantification of guttae is an important prerequisite for the Fuchs’ Dystrophy assessment and treatment, and it would allow a better understanding of the origin of visual impairment, as the authors of the references advocate. In the same way, the literature raises the hypothesis that guttae are the source of the aberrations of the posterior corneal surface, although the cause is so far unknown. Because of the presented results, using this high-resolution sensor, it has been possible to process the phase so guttae could be extracted, demonstrating the relevance of analyzing the wavefront phase further low orders, as well as the impact of these protrusions in the ocular aberrations. Alongside this, a reliable objective analysis of the guttae could be performed with an automatic detection method, being a valid tool for the diagnosis and monitoring of the pathology over time.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to private company reasons but are available from the corresponding author upon reasonable request.
References
Adamis, A., Filatov, V., Tripathi, B. & Tripathi, R. Fuchs endothelial dystrophy of the cornea. Surv. Ophthalmol. 38, 149–168. https://doi.org/10.1016/0039-6257(93)90099-s (1993).
Mustonen, R. et al. In vivo confocal microscopy of fuchs’ endothelial dystrophy. Cornea 17, 493–503. https://doi.org/10.1097/00003226-199809000-00006 (1998).
Elhalis, H., Azizi, B. & Jurkunas, U. Fuchs endothelial corneal dystrophy. Ocul. Surf. 8, 173–184. https://doi.org/10.1016/s1542-0124(12)70232-x (2010).
Fuchs, E. Dystrophia epithelialis corneae. Albrecht von Graefes Archiv fur klinische und experimentelle ophthalmologie 76, 478–508. https://doi.org/10.1007/BF01986362 (1910).
Kirby, D. Excrescences of the central area of descemet’s membrane. Arch. Ophthalmol. 54, 588–91 (1925).
Gifford, S. Epithelial dystrophy of the cornea and its relation to endothelial dystrophy. Am. J. Ophthalmol. 9, 81–85. https://doi.org/10.1016/S0002-9394(26)90951-3 (1926).
Ali, M., Cho, K. & Srikumaran, D. Fuchs dystrophy and cataract: Diagnosis, evaluation and treatment. Ophthalmol. Ther. 12, 691–704. https://doi.org/10.1007/s40123-022-00637-1 (2023).
Vedana, G., Villarreal, J. & Jun, A. Fuchs endothelial corneal dystrophy: Current perspectives. Clin. Ophthalmol. 10, 321–330. https://doi.org/10.2147/OPTH.S83467 (2016).
Zhang, J. & Patel, D. The pathophysiology of fuchs’ endothelial dystrophy - a review of molecular and cellular insights. Exp. Eye Res. 130, 97–105. https://doi.org/10.1016/j.exer.2014.10.023 (2015).
Kobashi, H., Kamiya, K. & Shimizu, K. Factors influencing visual acuity in fuchs’ endothelial corneal dystrophy. OPTOMETRY VISION SCI. 95, 21–26. https://doi.org/10.1097/OPX.0000000000001157 (2018).
Krachmer, J. Corneal endothelial dystrophy. Arch. Ophthalmol. 96, 2036. https://doi.org/10.1001/archopht.1978.03910060424004 (1978).
Repp, D., Hodge, D., Baratz, K., McLaren, J. & Patel, S. Fuchs’ endothelial corneal dystrophy subjective grading versus objective grading based on the central-to-peripheral thickness ratio. Ophthalmology 120, 687–694. https://doi.org/10.1016/j.ophtha.2012.09.022 (2013).
Matthaei, M. et al. Fuchs endothelial corneal dystrophy: Clinical, genetic, pathophysiologic, and therapeutic aspects. In Movshon, J. & Wandell, B. (eds.) Annu. Rev. Vis. Sci., vol. 5 of Annual Review of Vision Science, 151–175, https://doi.org/10.1146/annurev-vision-091718-014852 (Annual review of vision science, 2019).
Zoega, G. et al. Prevalence and risk factors for cornea guttata in the reykjavik eye study. Ophthalmology 113, 565–569. https://doi.org/10.1016/j.ophtha.2005.12.014 (2006).
Eghrari, A. et al. Retroillumination photography analysis enhances clinical definition of severe fuchs corneal dystrophy. Cornea 34, 1623. https://doi.org/10.1097/ICO.0000000000000656 (2015).
Giasson, C. J. et al. Morphometry of cells and guttae in subjects with normal or guttate endothelium with a contour detection algorithm. Eye Contact Lens 31, 158–165. https://doi.org/10.1097/01.icl.0000165286.05080.23 (2005).
Watanabe, S. et al. Relationship between corneal guttae and quality of vision in patients with mild fuchs’ endothelial corneal dystrophy. Ophthalmology 122, 2103–2109. https://doi.org/10.1016/j.ophtha.2015.06.019 (2015).
Soh, Y., Peh, G., Naso, S., Kocaba, V. & Mehta, J. Automated clinical assessment of corneal guttae in fuchs endothelial corneal dystrophy. Am. J. Ophthalmol. 221, 260–272. https://doi.org/10.1016/j.ajo.2020.07.029 (2021).
Hara, M., Morishige, N., Chikama, T. & Nishida, T. Comparison of confocal biomicroscopy and noncontact specular microscopy for evaluation of the corneal endothelium. Cornea 22, 512–515. https://doi.org/10.1097/00003226-200308000-00005 (2003).
Fujimoto, H. et al. Quantitative regional differences in corneal endothelial abnormalities in the central and peripheral zones in fuchs’ endothelial corneal dystrophy. Investig. Ophthalmol. Vis. Sci. 55, 5090–5098. https://doi.org/10.1167/iovs.14-14249 (2014).
Patel, S., Amin, S., Baratz, K., Kane, K. & McLaren, J. Anterior corneal aberrations in relation to severity of fuchs endothelial dystrophy. Investig. Ophthalmol. Vis. Sci. 55, 3580–3580 (2014).
Arora, R. et al. Analysis of corneal scheimpflug densitometry and ocular wavefront aberrations post descemet stripping automated endothelial keratoplasty. Eye Contact Lens 48, 242–249. https://doi.org/10.1097/ICL.0000000000000868 (2022).
van Dijk, K. et al. Optical quality of the cornea after descemet membrane endothelial keratoplasty. Am. J. Ophthalmol. 158, 71–79. https://doi.org/10.1016/j.ajo.2014.04.008 (2014).
Waldrop, W., Gillings, M., Robertson, D., Petroll, W. & Mootha, V. Lower corneal haze and aberrations in descemet membrane endothelial keratoplasty versus descemet stripping automated endothelial keratoplasty in fellow eyes for fuchs endothelial corneal dystrophy. Cornea 39, 1227–1234. https://doi.org/10.1097/ICO.0000000000002416 (2020).
Wacker, K., McLaren, J., Amin, S., Baratz, K. & Patel, S. Corneal high-order aberrations and backscatter in fuchs’ endothelial corneal dystrophy. Ophthalmology 122, 1645–1652. https://doi.org/10.1016/j.ophtha.2015.05.005 (2015).
Velarde-Rodriguez, G. et al. Ultra-high resolution optical aberrometry in patients with keratoconus: A cross-sectional study. Ophthalmol. Ther. 12, 1569–1582. https://doi.org/10.1007/s40123-023-00684-2 (2023).
Belda-Para, C. et al. Comparing the clinical applicability of wavefront phase imaging in keratoconus versus normal eyes. Sci. Rep. 14, 9984. https://doi.org/10.1038/s41598-024-60842-9 (2024).
Bonaque-González, S. et al. The optics of the human eye at 8.6 \(\mu\)m resolution. Sci. Rep. 11, 23334. https://doi.org/10.1038/s41598-021-02653-w (2021).
Trujillo-Sevilla, J. M., Casanova Gonzalez, O., Bonaque-González, S., Gaudestad, J. & Rodríguez Ramos, J. M. High-resolution wave front phase sensor for silicon wafer metrology. In Photonic Instrumentation Engineering VI, vol. 10925, 109250I, https://doi.org/10.1117/12.2505764. International Society for Optics and Photonics (SPIE, 2019).
Trujillo-Sevilla, J., Velasco-Ocaña, M., Bonaque-González, S., Belda-Para, C. & Rodríguez-Ramos, J. Wavefront phase measurement of striae in optical glass. Appl. Opt. 61, 3912–3918. https://doi.org/10.1364/AO.450219 (2022).
Cairós, C. et al. Refractive index estimation in biological tissues by quantitative phase imaging. Opt. Mater. 142, 114087. https://doi.org/10.1016/j.optmat.2023.114087 (2023).
Bonaque-González, S. et al. New high-resolution wavefront sensing ophthalmic technique for the characterization of ocular optics. Ophthalmic Technol. XXX 11218, 117–123. https://doi.org/10.1117/12.2548595 (2020).
Bonaque-González, S. et al. Extremely high resolution ocular aberrometry up to 2.4 million points. Investig. Ophthalmol. Vis. Sci. 60, 603–603 (2019).
Verma, S., Hesser, J. & Arba-Mosquera, S. Optimum laser beam characteristics for achieving smoother ablations in laser vision correction. Investig. Ophthalmol. Vis. Sci. 58, 2021–2037. https://doi.org/10.1167/iovs.16-21025 (2017).
Yang, X. & Cui, W. A novel spatial clustering algorithm based on delaunay triangulation. J. Softw. Eng. Appl. 03, 141–149. https://doi.org/10.4236/jsea.2010.32018 (2010).
Greenacre, M. et al. Principal component analysis. Nat. Rev. Methods Primers 2, 100. https://doi.org/10.1038/s43586-022-00184-w (2022).
MathWorks. Principal component analysis of raw data. https://es.mathworks.com/help/stats/pca.html.
MathWorks. Support vector machines for binary classification. https://mathworks.com/help/stats/support-vector-machines-for-binary-classification.html.
Cristianini, N. & Shawe-Taylor, J. An Introduction to Support Vector Machines and Other Kernel-based Learning Methods (Cambridge University Press, Cambridge, 2000).
McNemar, Q. Note on the sampling error of the difference between correlated proportions or percentages. Psychometrika 12, 153–157. https://doi.org/10.1007/bf02295996 (1947).
Dietterich, T. Approximate statistical tests for comparing supervised classification learning algorithms. Neural Comput. 10, 1895–1923. https://doi.org/10.1162/089976698300017197 (1998).
Rainio, O., Teuho, J. & Klén, R. Evaluation metrics and statistical tests for machine learning. Sci. Rep.[SPACE]https://doi.org/10.1038/s41598-024-56706-x (2024).
Rosenblum, P., Stark, W., Maumenee, I., Hirst, L. & Maumenee, A. Hereditary fuchs’ dystrophy. Am. J. Ophthalmol. 90, 455–462. https://doi.org/10.1016/s0002-9394(14)75011-1 (1980).
Dong, W., Zou, L., Pan, Z. & Wang, L. Morphologic characteristics of cornea in fuchs endothelial dystrophy observed by confocal microscopy. [Zhonghua yan ke za zhi] Chin. J. Ophthalmol. 40, 465–470 (2004).
Vaitinadapoulé, H. et al. Nanotopography by chromatic confocal microscopy of the endothelium in fuchs endothelial corneal dystrophy, pseudophakic bullous keratopathy and healthy corneas. Br. J. Ophthalmol.[SPACE]https://doi.org/10.1136/bjo-2023-323297 (2023).
Iovino, C. et al. Corneal endothelium features in fuchs’ endothelial corneal dystrophy: A preliminary 3d anterior segment optical coherence tomography study. PLoS ONE 13, 1–12. https://doi.org/10.1371/journal.pone.0207891 (2018).
Shah, K., Eghrari, A., Vanner, E., O’Brien, T. & Koo, E. Scheimpflug corneal densitometry values and severity of guttae in relation to visual acuity in fuchs endothelial corneal dystrophy. Cornea 41, 692–698. https://doi.org/10.1097/ico.0000000000002762 (2022).
van Dam, M. & Lane, R. Extended analysis of curvature sensing. JOSA A 19, 1390–1397. https://doi.org/10.1364/JOSAA.19.001390 (2002).
Eleiwa, T., Elsawy, A., Ozcan, E. & Abou Shousha, M. Automated diagnosis and staging of fuchs’ endothelial cell corneal dystrophy using deep learning. Eye and Vision 7, 44. https://doi.org/10.1186/s40662-020-00209-z (2020).
Elsawy, A. et al. Multidisease deep learning neural network for the diagnosis of corneal diseases. Am. J. Ophthalmol. 226, 252–261. https://doi.org/10.1016/j.ajo.2021.01.018 (2021).
Acknowledgements
J.G.M.-H. was partially funded by “Research agreement on ophthalmology Wooptix-ULL, 2023”.
Author information
Authors and Affiliations
Contributions
C.B.P. contributed to all stages of the project, J.G.M.H. contributed to all stages of the project, M.V.O. contributed to all stages of the project except data acquisition, J.M.T.S. contributed to the software used in the work and the manuscript review, J.M.R.R. contributed to all stages of the project except data acquisition, G.V.R. contributed to the acquisition of the data and the manuscript review, N.A.A. contributed to the acquisition of the data and the manuscript review.
Corresponding author
Ethics declarations
Competing interests
The authors declare the following competing interests: C.B.P., employment. M.V.O., employment. J.M.T.S., employment. J.M.R.R., funding. J.G.M.H., non-financial competing interests. G.V.R., non-financial competing interests. N.A.A., non-financial competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Belda-Para, C., Velarde-Rodríguez, G., Marichal-Hernández, J.G. et al. Fuchs’ Endothelial Corneal Dystrophy evaluation using a high-resolution wavefront sensor. Sci Rep 14, 20369 (2024). https://doi.org/10.1038/s41598-024-71480-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71480-6
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.