Abstract
Growing intracranial aneurysms pose a high risk of rupture, making the detection and quantification of the growth crucial for timely treatment strategy adoption. In this paper we propose a computer-assisted approach based on the extraction of IA shapes from associated baseline and follow-up angiographic scans and non-rigid morphing of the two shapes. From the obtained shape deformations we computed four novel features, including differential volume (dV), surface area (dSA), aneurysm-size normalized median deformation path length (dMPL), and integral of cumulative deformation distances (dICDD). An experienced neuroradiologist manually extracted the IA shape models from the baseline and follow-up MRAs and, by utilizing size change and visual assessments, classified each aneurysm into stable with morphology changes, stable or growing. We investigated the classification performance and found that three of the novel and one cross-sectional feature exhibited significantly different mean values (p-value \(< 0.05\); Tukey’s HSD test) between the stable and growing IA groups, while the mean dICDD was significantly different between all the three groups. The cross-sectional features has sensitivity to growing IAs in range 0.05–0.86, while novel features had generally higher sensitivity in range 0.81–0.90, making them promising candidates as surrogate follow-up imaging-based biomarkers for IA growth detection. These findings may offer valuable information for clinical management of patients with IAs based on follow-up imaging.
Similar content being viewed by others
Introduction
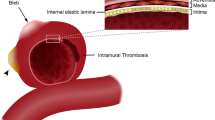
Intracranial aneurysm (IA) is an abnormal dilation of the cerebral blood vessel wall. If such an IA ruptures, it can lead to subarachnoid hemorrhage (SAH), a condition associated with significant morbidity and mortality. The prevalence of unruptured IAs in the general population ranges from 2 to 8%1, while the incidence of rupture and SAH is much lower, estimated at around 20 cases per 100,000 individuals per year2. Nevertheless, the ruptured IAs are fatal in approximately 40% of cases, and about 66% of survivors suffer from permanent neurological deficits. Since treatment and socio-economic costs associated with IA and SAH are substantial (£510 million based on a 2010 study in the United Kingdom3), there is a need to develop inventive preventive techniques and strategies.
The increasing numbers of the IAs discovered before rupture present an opportunity for optimization and timely adoption of treatment strategies. Because surgical preventive treatment presents a certain risk of complications, i.e. all-cause mortality rates of the clipping and coiling groups amount to respective 3.6% and 3.8%4, an emerging approach is longitudinal monitoring of IAs using imaging. The imaging seems justified when the risk of complications is higher than the risk of spontaneous rupture5. A 2006 study of unruptured IAs showed that annual rupture rate was 0.8% for small IAs (neck width \(<3.9\) mm), 1.2% for medium (4–10 mm), 7.1 % for large (10–25 mm) and 43.1% for the giant ones (\(>25\) mm). The relatively low rupture risk for small to medium IAs is the reason for the increasingly more frequent decision to monitor the IAs using follow-up imaging and postponing surgery until evidence of elevated rupture risk is established.
The prevailing and widely accepted hypothesis is that growing IAs have a higher risk of rupture, leading to the use of IA size changes as a surrogate measure of rupture risk. For instance, some studies assume an enlargement of \(\ge 1\) mm in IA size as a growth-associated rupture risk factor6,7. The IA size measurements are conducted by neurosurgeons using simple manual annotation and measurement tools on 2D image cross-sections8. This approach, however, is subject to a rather high intra- and inter-rater variability. For instance, Ref.9 evaluated the inter-rater intraclass correlation coefficient of manual measurements of aneurysm neck size at 0.52 (95% CI 0.31-0.74) and of aneurysm size at 0.96 (95% CI 0.94-0.98). Such variability in the measurements that form the basis for rupture risk assessment may have critical consequences. Namely, growing aneurysms may be incorrectly labeled as stable, a highly likely situation when growth patterns involve irregular or multilobular shape variations. A more accurate, reliable and objective approach that takes into account all possible 3D morphological changes is to assess IA size change status using computer-assisted analyses of the baseline and follow-up angiographic scans.
Recent study9 focused on automatic measurements of IA size and neck width, demonstrating that it can aid radiologists in achieving more consistent measurements. The automatic cutting plane positioning methods proposed by Refs.10,11 perform effectively for IAs of representative saccular shape and simple parent vessel configuration. However, they may encounter difficulties when handling complex parent vessels configuration and irregular or multilobular shape of IAs. In recent years, numerous deep learning methods12,13,14 have also been proposed to isolate the IAs from the parent vessels. The aforementioned approaches, however, were designed to analyze the IA morphology from a single angiographic scan and do not seem adequate for the baseline to follow-up comparison of IA and its parent vessels’ shape changes over time. In this study, our main objective is to provide a comprehensive description of the Computer-Assisted Aneurysm Growth Evaluation and Detection (AGED) method, including novel features that have demonstrated promising results during a preliminary clinical evaluation15 on computer tomography angiographic (CTA) scans, and conduct an extended evaluation of its effectiveness on a new dataset, utilizing magnetic resonance angiography (MRA) scans for the assessment. AGED is a novel longitudinal IA shape morphing method that maps the baseline IA shape model into the follow-up one and, at the same time, propagates the baseline IA shape’s isolation, effectively eliminating potential errors arising if case isolation method is independently applied to the baseline and follow-up IA shape. The shape morphing yields deformation maps, from which rupture-risk associated surrogate features such as differential surface area and volume (dSA and dV, respectively), and two novel differential features, i.e. median deformation path length (dMPL), normalized by the baseline IA size, and an integral of cumulative deformation distances (dICDD) are computed. As a comparative benchmark, by applying an isolation approach independently to the baseline and follow-up IA shape, we compute relative changes in previously well-studied and commonly applied morphologic features, such as the IA’s maximum dome size, surface area, volume, neck size index (NSI)16. The performance analysis regarding the IA status change classification indicates that the most discriminative features were the novel features derived from the proposed AGED method.
Experiments and results
Experiments involved (1) quantitative and qualitative validation of shape morphing approach, (2) rigorous evaluation of the extracted longitudinal morphologic features to determine their suitability as potential surrogate biomarkers of aneurysm size change, (3) validation of agreement between the cross-sectionally and longitudinally extracted volume and surface area change feature values, and (4) evaluation of execution times.
Validation of shape morphing
The proposed AGED approach is based on shape morphing, which relied on three empirically determined parameters, \(\kappa\), \(k_{max}\) and \(\textrm{PL}_r\). The \(\kappa\) and \(k_{max}\) were set to 0.15 and 30, respectively. Validation of the shape morphing was two-fold and involved (1) quantification of the the average distance between baseline points and corresponding intersections, which should evaluate close to zero after the \(k_{max}\) iterations of the IMTMD, and (2) qualitative visual assessment and comparison of the morphed baseline and the follow-up shape models.
First, we found that after the \(k_{max}=30\) iterations, the aforementioned average distance was less than 0.02 mm in all 50 baseline and follow-up pairs, indicating that the selected values for \(\kappa\) and \(k_{max}\) were suitable and the the IMTMD converged successfully. Based on this observation we set the residual path length parameter \(\textrm{PL}_r\) to value \(-0.1\), for the dICDD feature computation. Second, Fig. 1 shows various cases of overlayed morphed baseline and follow-up shape models, indicating that the IMTMD had successfully morphed the former into the latter. The morphed baseline in intermediate iterations of the IMTMD show a sensible simulation of morphologic changes in growing and semi-stable (stable with morphology changes) IAs, hence, validating the approach.
Evaluation of longitudinal morphologic features
We evaluated the discriminative ability of the computed longitudinal morphological features in distinguishing between the growing, stable, and semi-stable (stable with morphology changes) groups of the IAs. For this purpose we employed Tukey’s HSD (honestly significant difference) test17. The significance of differences between the means of the three groups was established if the p-value was less than 0.05. By subjecting each feature value to the Tukey’s HSD test, we compared the group means and summarized the descriptive statistics and classification performance in Table 1. Figure 2 show feature distributions in form of violin plots to facilitate visual comparison among the features values in the three groups (stable with morphology changes, stable, and growing).
Aneurysm size change feature distributions in form of violin plots, according to the three groups. Upper row: four novel longitudinal and bottom row four cross-sectional features. Horizontal lines indicate tentative separation thresholds (t) between the semi-stable/stable vs. growing aneurysm groups and associated sensitivity or true positive rate (TPR; value of 1 is optimal).
The comparison of cross-sectional IA change features revealed significant p-values for all features when comparing semi-stable vs. growing groups. However, when comparing means in stable vs. growing groups, only the cSA demonstrated significance (p = 0.027), while cANI was significant (p = 0.039) for semi-stable vs. stable groups. The cSA exhibited significant differences in semi-stable vs. growing (p = 0.001) and stable vs. growing (0.027), but not between semi-stable and stable (p = 0.088) groups. Similarly, the cV showed significant difference between semi-stable vs. growing (p = 0.006) and stable vs. growing (p = 0.085), but not for semi-stable vs. stable (p = 0.291) groups.
On the other hand, among the novel features, dICDD exhibited significant differences in between-group mean comparisons (p \(<0.017\)), indicating its advanced ability to distinguish between all group pairs effectively. While dMPL outperformed the dICDD according to lower p-value (0.008 vs. 0.015 in semi-stable vs. stable groups, it did not exhibit significant difference (p = 0.085) in mean comparison of stable vs. growing groups. Additionally, the dV was able to differentiate between the semi-stable vs. growing and stable vs. growing groups, but failed to distinguish between the semi-stable vs. stable groups.
Differentiating between the semi-stable/stable vs. growing groups is clearly of the highest clinical interest and the features extracted by the AGED approach provided most discriminative features. While potentially less relevant, it is interesting that the dICDD and dMPL features provided good discrimination between the semi-stable vs. stable groups.
Agreement of corresponding features
The cross-sectional and longitudinal approach yielded two sets of corresponding features, namely the cV and dV and the cSA and dSA, for which we assessed their agreement using Bland-Altman analysis, Wilcoxon signed rank testing and intra-class correlation coefficient (ICC) . Results are presented in Fig. 3. In the Bland–Altman plot, we observe that the largest differences exist within the growing group, whereas the differences are closer to zero for the stable and semi-stable groups. Pairwise feature comparison using Wilcoxon signed rank tests indicated that differences between the corresponding measurements were not significant, namely the comparison between cSA/dSA and cV/dV yielded a p-value of 0.56 and 0.41, respectively. The respective ICC values were 0.67 and 0.66, which, by following the interpretation provided by Koo et al.18, indicates moderate level of agreement (range 0.5–0.75).
Execution times
The shape morphing registration process for each pair of baseline and follow-up shape models was completed within a reasonable time frame, taking between 30 s and 2 min, with nearly linear dependence of execution time on the number of vertices in the baseline IA shape model.
The initial rigid registration step utilized the Go-ICP method, coded in C and was optimized for speed. The subsequent non-rigid IMTMD method was implemented in Python 3 and was not optimized for speed. The most time consuming step of the IMTMD was finding the intersection points, which could be easily implemented on modern massively parallel architectures with an expected order of magnitude speed-up.
Discussion
In this study, we presented AGED for aneurysm size change assessment and performed its thorough evaluation and comparison to established cross-section size change assessment. While AGED had previously undergone clinical evaluation in a preliminary study involving 20 CTA pairs15, our focus in this research was on the longitudinal analysis of 50 aneurysms cases based on MRA scans. This novel dataset was utilized as an external test dataset to evaluate the proposed method AGED.s Additionally, we provided a comprehensive description of the AGED methodology and its technical details, not disclosed in the previous study. In this study we also included additional group (semi-stable) which focuses on aneurysms that have shrinked. We explored both the established cross-sectional features and the novel longitudinal ones as potential biomarkers for computer-assisted aneurysm size change assessment.
Among the eight tested features, only the dICDD showed significant p-values and could distinguish between the three studied aneurysm size change groups (i.e. semi-stable, stable and growing). While it is beneficial for a feature to differentiate between the semi-stable and stable aneurysms, the most clinically relevant aspect is its ability to distinguish between the semi-stable/stable and growing aneurysms, as the latter are more likely to rupture. Table 1 reveals that the most effective model for distinguishing between the stable and growing aneurysms was dSA, with a significant p-value of 0.003, closely followed by dV with a p-value of 0.006. The dICDD and cSA also achieved significant p-values of 0.017 and 0.027, respectively. All features were capable of distinguishing between the semi-stable and growing aneurysms, but this distinction lacks additional clinical value.
We note that initially we examined 14 distinct cross-sectional features15, however, herein we presented only the four key cross-sectional features, specifically the maximum dome height or HMAX, aneurysm volume (V), surface area (SA), and anisotropy (ANI), since these have demonstrated the most promising discrimination power as classifiers of aneurysm size change status.
When examining the most promising novel features, it becomes evident that there is still some overlap among the three groups, as seen from the violin plots in Fig. 2. This overlap can be attributed to the manual 2D measurements of baseline and follow-up aneurysms. There measurements were the basis to determine the reference aneurysm size change status, but which are susceptible to both intra- and inter-rater variability. Consequently, in instances where aneurysm growth is not adequately defined, it may be challenging for any algorithm to definitively determine whether the aneurysm is indeed growing or not.
A valuable byproduct of AGED that may help address the aforementioned consideration is the a visual representation of longitudinal aneurysm development (cf. Figs. 4b and 1). This tool could enable neurosurgeons to gain deeper insights into the changes in the 3D aneurysm morphology over time. For example, identifying shape alterations in a small local area may indicate higher risk, providing critical information for more informed decision-making and patient management.
(a) Cross-sectional approach: morphologic features computed independently on baseline and follow-up aneurysm shape and their relative change considered as an aneurysm size change biomarker. (b) The AGED approach utilizes rigid initial shape baseline to follow-up co-registration and their non-rigid shape morphing to compute novel aneurysm size change features.
The validity of AGED was verified by the matching of the morphed baseline and the follow-up shapes, visually and by assessing inter-shape distances (\(<0.02\) mm on average), but also by analysing the agreement of the two corresponding pairs of features, cSA and dSA, cV and dV, between the cross-sectional analysis approach and the longitudinal approach applied by AGED. Figure 3 demonstrates that the corresponding features exhibit similar mean values (p-value \(>0.41\) of paired Wilcoxon signed rank test) and moderate agreement according to the intra-class correlation coefficient in range of 0.5–0.7518.
It is however noteworthy that the novel features dSA and dV could discriminate better between the stable and growing aneurysm size change groups, with p-values of 0.003 and 0.006, respectively, whereas their cross-sectional counterparts, cSA and cV, yielded respective p-values of 0.027 and 0.085. This indicates that the novel features by AGED are more effective in distinguishing between the stable and growing aneurysms, which is also reflected in higher sensitivity at 0.90 for both dSA and dV, while the respective values for cSA and cV were 0.86 and 0.67 (cf. Fig. 2). This finding aligns with the fact that, although these features exhibit similarity, the novel AGED approach jointly considers the baseline to follow-up shape information through the shape morphing and therefore estimates the features with lower variability.
The improved classification performance achieved by the proposed AGED approach can be attributed to its high sensitivity to local morphological changes. In the cross-sectional analysis approach, the independent isolation of baseline and follow-up aneurysm dome shapes can lead to variations in the feature values, either due to inconsistent (automatic) isolation and/or rater variability. It is crucial to recognize that even minor inconsistencies with error magnitude of 1 mm could mistakenly indicate aneurysm growth. The AGED approach provides a significant advantage by eliminating the potential bias introduced by two independent aneurysm isolations. Namely, the AGED approach uses the baseline aneurysm shape isolation, which is subsequently deformed into the follow-up aneurysm shape, thus ensuring more reliable and consistent measurements. In this way, the AGED approach ensures that the extracted features (dICDD, dMPL, dSA, and dV) are not influenced by the variability of aneurysm isolation between the baseline and follow-up shapes. This led to consistently lower variability in the feature values, as seen in Fig. 2, whereas this reduced variability contributes to more reliable and consistent measurements.
The shape morphing approach was empirically stopped after \(k_{max}=30\) iterations, since iterations beyond that led to negligible deformations of the baseline shape and average distance towards the follow-up aneurysm shape was 0.02 mm. To ensure , We have visually inspected each registered pair of baseline and follow-up shapes (as in Fig. 1) so as to confirm the validity of the shape morphing process. An alternative solution could be to enhance the AGED algorithm by analyzing the distribution of incremental path lengths at each iteration and, for instance, stop the morphing process once the median of incremental path lengths in last iteration falls below certain threshold (e.g. 0.02 mm), ensuring a more data-driven and robust approach for determining the optimal number of iterations.
One potential limitation of this study is a rather low number of cases across all groups. To better estimate the effect size we aim to collect more cases, however, this is made difficult by the fact that “follow-up imaging” approach only recently started to gain adoption in clinical workflows and, therefore, there is scarce data regarding follow-up angiographic imaging of unruptured intracranial aneurysms. Nevertheless, the statistical analysis on groups of 17 stable, 25 growing and 8 semi-stable aneurysms cases showed that the novel and very promising surrogate biomarkers of aneurysm morphology change could be derived from the shape morphing based AGED approach.
Accurate monitoring of aneurysm growth is crucial in clinical practice as it can significantly impact patient management decisions. The growth rate of an aneurysm is a key indicator of its stability and rupture risk. Radiologists often perform manual measurements of aneurysm dimensions, which can be prone to errors due to inter-observer variability and the complexity of aneurysm shapes, similarly to the variations observed in the aneurysm isolation process. These mistakes can lead to misinterpretation and potentially delay necessary interventions for high-risk aneurysms or subject low-risk aneurysms to unnecessary procedures. An algorithm like AGED, and upon based classification models (cf. thresholds in Fig. 2), which automate the aneurysm size change assessment and quantification process, could greatly improve the accuracy and reliability of aneurysm assessment in routine clinical practice. By providing an objective and consistent measurements, AGED could enhance the radiologist’s ability to identify aneurysms at higher risk of rupture, leading to more timely and targeted treatment strategies, ultimately improving patient outcomes.
Materials and methods
In this section, we detail our evaluation dataset, two distinct IA shape change assessment methodologies, namely (1) a standard cross-sectional and (2) a novel longitudinal approach dubbed AGED, and the morphological IA shape change features derived from the analyses to serve as potential biomarkers associated to rupture risk.
Data
The dataset included a total of 45 patients (21 males and 24 females) with at least one unruptured saccular-type IA (41 had a single aneurysm, 3 had 2 aneurysms, and 1 had 3 aneurysms), where for each patient we had a pair of baseline and follow-up 3D MRA scans.
The data was acquired at the University Medical Center Ljubljana as part of a retrospective study. The study received approval from the National Medical Ethics Committee of the Republic of Slovenia. Since the study did not affect patient care and all data were anonymized, the committee waived the requirement for informed consent. Ethical guidelines outlined in the Helsinki Declaration and endorsed by institutional and national research committees were strictly adhered to throughout data collection and experimentation. All MRA acquisitions were performed on the Philips Achieva 1.5T scanner, using standard clinical protocols. Namely, the in-plane voxel spacing ranged from 0.35 to 0.45 mm, slice thickness from 0.5 to 1.29 mm, in-slice sampling from \(384 \times 284\) to \(672 \times 768\), and the number of slices from 160 to 360. The average time difference between the acquisition of baseline and follow-up scans was 2.50 years, with a minimum of 2.25 and a maximum of 9.00 years (refer to Table 2 for detailed dataset information). The time elapsed between the baseline and follow-up imaging sessions for each patient is also illustrated in Boxplot in Appendix Fig. 1.
A skilled neuroradiologist with more than 15 years of experience annotated the MRA dataset, which included a total of 50 IAs. First, a region of interest (ROI) encompassing the IA and the surrounding vessels was manually selected. Interactive thresholding was applied within the ROI to segment the aneurysm and vessels from the background. The reconstruction of the corresponding 3D surface meshes was accomplished using the marching cubes and smooth non-shrinking algorithms19,20. To ensure accuracy, potential errors or inconsistencies in the obtained aneurysm mesh, such as unattached vessels and small structures not belonging to the IA mesh, were manually corrected using MeshLab (version 2021.10).
The annotations made by the neuroradiologist involved manually determined maximal dome diameter of the IAs (referred to as the IA size). All measurements were subsequently compared to the values reported in official radiological reports to identify any discrepancies. In instances where discrepancies were found, a senior radiologist established the correct value. The IA sizes ranged from 1.4 to 12.2 mm, with a median diameter of 4.3 mm across the 50 cases. Notably, the dataset was predominantly composed of small to medium-sized IAs (diameter \(< 7\) mm), which presents a representative cohort for the follow-up imaging assessments. Based on the manual baseline and follow-up IA size measurements and a side-by-side visual analysis of the corresponding baseline and follow-up shapes the neuroradiologist classified each of the 50 IAs into one of three categories: stable, semi-stable, or growing. The classification resulted in 17 stable, 8 semi-stable, and 25 growing aneurysms in the dataset. By incorporating shapes, we aimed to overcome the limitations of 2D manual measurement and provided the radiologist with three-dimensional information about IA morphology.
Longitudinal aneurysm assessment
We present two distinct methodologies for longitudinal IA assessment, namely (1) a cross-sectional analysis that independently evaluates morphologic features from the baseline and follow-up MRA scans, and (2) a novel longitudinal approach dubbed Computer-Assisted Aneurysm Growth Evaluation and Detection (AGED). Both approaches extract feature values that will undergo rigorous evaluation to determine their suitability as potential surrogate biomarkers of aneurysm size change.
Cross-sectional analysis
We performed a well-established cross-sectional analysis and extracted associated morphological features21,22. The outline of the approach is depicted in Fig. 4a. The baseline and follow-up surface models were independently annotated using the RealGUIDE medical image visualization and annotation software (version 5.0; 3DIEMME Srl., Cantù, Italy). First, the IA and parent vessel parts were manually isolated. The isolation process involved the neuroradiologist clicking consecutive points on the vascular mesh to establish a closed curve, i.e. the IA neck, serving as a demarcation line to distinguish the IA from the parent vessels.
The morphological analysis of the isolated IA shape involved computing four features: maximum dome height (HMAX), volume (V), surface area (SA), and anisotropy (ANI). To quantify the relative change between the baseline and follow-up IA shape, we computed the difference between the corresponding values and then divided it by the baseline value. This calculation yielded features cHMAX, cV, cSA, and cANI, where the small letter ’c’ indicates the cross-sectional nature of feature change computation.
AGED: longitudinal analysis
Although AGED has been utilized in a preliminary clinical study15, its methodology has not been published yet. In this section, we provide a comprehensive and detailed description of the AGED approach, which is composed of two steps: (1) an initial rigid alignment of baseline and follow-up IA shapes, followed by their (2) non-rigid shape morphing. Figure 4b depicts the overall shape co-registration process, while detailed descriptions of each registration step and the extraction of morphological features are given in subsequent subsections.
Rigid registration
The rigid registration process in this study utilized the Go-ICP algorithm23, an iterative closest point method renowned for its ability to find a global alignment solution, regardless of the initial poses of the baseline and follow-up shapes. The Go-ICP incorporates the local ICP registration24 within a branch and bound (BnB) framework, enabling comprehensive exploration of the entire 3D motion space SO(3) to find the global alignment solution. We used a publicly available implementation provided by the original authors of Go-ICP, version 1.325. In IA cases exhibiting growth, considerable disparities may emerge between the baseline and follow-up IA shapes, posing challenges in shape co-registration using the Go-ICP. To address this, we adopted a selective approach, focusing solely on the parts of the surface meshes corresponding to the parent vessels of the IA. This decision was based on the assumption that the IA’s parent vessels remain mostly unchanged even if the IA grows or shrinks. This strategy successfully improved the robustness of the rigid registration process using Go-ICP, particularly for the IAs exhibiting substantial morphological changes.
Non-rigid registration
For a comprehensive characterization of the changes between the baseline and follow-up aneurysm shapes, we developed a novel non-rigid shape registration algorithm called Iterative Mesh to Mesh Deformation (IMTMD). This algorithm aims to achieve a perfect alignment of the baseline and follow-up IA shape models though morphing the former into the latter. The resulting deformation reveals the IA changes between (and within) the considered time points. The detailed outline of the IMTMD shape morphing algorithm can be found in Algorithm 1.
The input into the IMTMD algorithm are the rigidly co-registered vertices \(v_j \in \mathscr {V}\) and faces \(f_i \in \mathscr {F}\) of the respective baseline (\(\{\mathscr {V}^{I}, \mathscr {F}^{I}\}\)) and follow-up (\(\{\mathscr {V}^{I}, \mathscr {F}^{II}\}\)) surface meshes. The input surface mesh included regions corresponding to the IA’s dome and its parent vessels. Each face is defined by three vertices \(f_i = [v_x,v_y,v_z]\) and a face normal denoted as \(\overrightarrow{n}_{f,i}\), calculated using the cross product of the vectors formed by any two distinct pairs of the face points. For further computations, we interpolate the vertex normals \(\overrightarrow{n}_{v,j}\) from proximal face normals \(\overrightarrow{n}_{f,i}\) as follows:
where \(\mathscr {C} = \{i; v_{j} \in f_i\}\) represents a set of indices of proximal face normals, and \(|\cdot |\) denotes the cardinality of the set.
In the first step of Algorithm 1, we compute the follow-up shape’s face normals \(\overrightarrow{n}_{f,i}^{II}\), which remain constant throughout the execution of the algorithm. Within the number of iterations loop (step 2), we compute the baseline shape’s vertex normals \(\overrightarrow{n}_{v,j}^{II}\) using Eq. (1).
In step 3, for each vertex on the baseline shape \(v_{j}^{I}\), we seek the intersections \(P_{j,k}^{II}\) between the line going through \(v_{j}^{I}\) with a direction coefficient of \(\overrightarrow{n}_{v,j}^{I}\) and the follow-up shape’s face \(\mathscr {F}^{II}\). For future computations, we assume that the normal \(\overrightarrow{n}_{p,j}^{II}\) at each intersection on the follow-up shape \(P_{j,k}^{II}\) is the same as the normal of the intersected face \(\overrightarrow{n}_{f,i}^{II}\).
To determine the matching intersection point \(p_j\) (step 4) from the set of possible intersections \(P_{j,k}^{II}\) (see Fig. 5), we follow a two-step process: (1) eliminate intersections with a dot product between \(\overrightarrow{n}_{v,j}^{I}\) and \(\overrightarrow{n}_{P_{j,k}}^{II}\) smaller than \(\tau\), and (2) among the remaining points that pass the dot product condition, we choose the closest point. The value of \(\tau\) was empirically set to 0.8, which ensured that the vertex’s normal \(\overrightarrow{n_i^{I}}\) and the corresponding intersection normal (\(\overrightarrow{n_{p_i}^{II}}\)) had similar orientations. Selecting the matching k from \(P_{j,k}^{II}\) was thus defined as:
where \(\Vert \cdot \Vert\) denotes the L2 distance. A graphical representation of the matching process is shown in Fig. 5.
Given the corresponding intersection \(p_j\) and \(v_j^{I}\), the subsequent steps involved computing the deformation that gradually warped the baseline shape towards the follow-up shape. We employed a simple translation for each baseline shape’s vertex in the direction of the \(p_j\), according to the following equation:
where \(\kappa\) is a constant value, m denotes the iteration number, and \(m_{max}\) denotes the maximal iteration count. For regularization purposes, we set the constant \(\kappa\) to empirically determined value of 0.15. Such low value of \(\kappa\) made convergence of the method rather slow, but at the same time reduced the likelihood of causing discontinuous deformations of the baseline shape across the iterations. The number of iterations \(m_{max}\) was set to 30, which was found sufficient in all 50 cases to morph the baseline shape into the follow-up one.
Novel morphologic features
Four novel morphologic features are derived based on the obtained deformations between the baseline and follow-up IA shape models, as obtained by shape morphing using IMTMD algorithm. In all feature abbreviations we use letter ’d’ to indicate the differential (or longitudinal) nature of feature computation.
The first two features are based on path length (\(PL_j\)), which is approximated by summing the deformation vectors for each point on the baseline shape across all IMTMD iterations:
For stable aneurysms, it is expected that the distribution of \(\textrm{PL}_j\) for all indices \(j_D\in \{j; v_j^{I} \in \mathscr {V}^{I} / \mathscr {V}_{vessels}^{I}\}\) belonging to the IA dome will be unimodal around the value zero. On the other hand, for growing IAs, it will extend from zero towards higher values and may even exhibit multiple modes. Figure 6a illustrates the path length distribution. The first proposed feature is the median path length (dMPL):
where the role of HMAX is to normalize path lengths according to the baseline size of the IA, thus expressing its relative change in size.
The second feature is the integral of cumulative deformation distances (dICDD), in which the cumulative density (cd) is computed based on the final deformation path lengths (PLs). Each value of cd is defined as the fraction of vertices \(v_j^{I}\) on the image with a \(\textrm{PL}_j\) less than or equal to the specified \(\textrm{PL}_j\). dICDD is the integral of cd:
where \(j_D\) represents indexes of vertices on the IA dome, \(\textrm{PL}_r\) the expected residual error and \(\max _j(\textrm{PL})\) the maximal PL in the particular case. The slope of the cd is expected to be steeper for stable IAs around the value of \(\textrm{PL}_r\), while for growing IAs, the slope will be more gradual. For graphical representation of the cd, see Fig. 6b.
The third and fourth novel features quantify volume change (dV) and surface area change (dSA). The dV is computed as follows:
where \(V_{i,m}(f_i^{{I}_m}, f_i^{{I}_{m-1}})\) represents the volume defined by points of one face (\(f_i^{{I}}\)) in two consecutive iterations of the IMTMD algorithm, m is the number iterations, and i are the indices of all the faces belonging to the baseline shape’s IA dome. The enclosed volume \(V_{i,m}(f_i^{{I}_m}, f_i^{{I}_{m-1}})\) is depicted in Fig. 6c.
The dSA is computed as:
where \(\mathscr {F}_{dome}^{I} = \mathscr {F}^{I} / \mathscr {F}_{vessels}^{I}\), \(\sum _i \textrm{SA}_i^{{I}_{m_{max}}}\) represents the surface area of the baseline IA shape’s dome in the last iteration of the IMTMD algorithm, and \(\sum _i \textrm{SA}_i^{{I}_0}\) the surface area of the non-deformed baseline IA shape’s dome.
Data availability
Due to the sensitive medical nature of the images, data availability is restricted. However, upon reasonable request, access to the data can be provided.
References
Vlak, M. H., Algra, A., Brandenburg, R. & Rinkel, G. J. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: A systematic review and meta-analysis. Lancet Neurol. 10, 626–636 (2011).
Kotowski, M. et al. Safety and occlusion rates of surgical treatment of unruptured intracranial aneurysms: A systematic review and meta-analysis of the literature from 1990 to 2011. J. Neurol. Neurosurg. Psychiatry 84, 42–48 (2013).
Rivero-Arias, O., Gray, A. & Wolstenholme, J. Burden of disease and costs of aneurysmal subarachnoid haemorrhage (asah) in the united kingdom. Cost Effectiveness Resource Allocation 8, 6 (2010).
Belavadi, R. et al. Surgical clipping versus endovascular coiling in the management of intracranial aneurysms. Cureus 13, https://doi.org/10.7759/cureus.20478 (2021).
Brinjikji, W. et al. Risk factors for growth of intracranial aneurysms: A systematic review and meta-analysis. Am. J. Neuroradiol. 37, 615–620 (2016).
van der Kamp, L. T. et al. Risk of rupture after intracranial aneurysm growth. JAMA Neurol. 78, 1228–1235 (2021).
Hackenberg, K. A. et al. Definition and prioritization of data elements for cohort studies and clinical trials on patients with unruptured intracranial aneurysms: Proposal of a multidisciplinary research group. Neurocrit. Care 30, 87–101 (2019).
Backes, D., Rinkel, G. J., Laban, K. G., Algra, A. & Vergouwen, M. D. Patient-and aneurysm-specific risk factors for intracranial aneurysm growth: A systematic review and meta-analysis. Stroke 47, 951–957 (2016).
Rajabzadeh-Oghaz, H. et al. Computer-assisted three-dimensional morphology evaluation of intracranial aneurysms. World Neurosurg. 119, e541–e550 (2018).
Piccinelli, M. et al. Automatic neck plane detection and 3d geometric characterization of aneurysmal sacs. Ann. Biomed. Eng. 40, 2188–2211 (2012).
Jerman, T., Pernuš, F., Likar, B., Špiclin, Ž. & Chien, A. Automatic cutting plane identification for computer-aided analysis of intracranial aneurysms. in 2016 23rd International Conference on Pattern Recognition (ICPR), 1484–1489 (IEEE, 2016).
Bizjak, Ž., Likar, B., Pernuš, F. & Špiclin, Ž. Vascular surface segmentation for intracranial aneurysm isolation and quantification. in Medical Image Computing and Computer Assisted Intervention–MICCAI 2020: 23rd International Conference, Lima, Peru, October 4–8, 2020, Proceedings, Part VI 23, 128–137 (Springer, 2020).
Podgorsak, A. R. et al. Automatic radiomic feature extraction using deep learning for angiographic parametric imaging of intracranial aneurysms. J. Neurointervent. Surg. 12, 417–421 (2020).
Bizjak, Ž, Pernuš, F. & Špiclin, Ž. Deep shape features for predicting future intracranial aneurysm growth. Front. Physiol. 12, 644349 (2021).
Chien, A., Špiclin, Ž., Bizjak, Ž. & Nael, K. Computer-assisted aneurysm growth evaluation and detection (aged): Comparison with clinical aneurysm follow-up. J. Blood Disord. Transfusion. 13, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10174624/ (2022).
Dhar, S. et al. Morphology parameters for intracranial aneurysm rupture risk assessment. Neurosurgery 63, 185–197 (2008).
Tukey, J. W. Comparing individual means in the analysis of variance. Biometrics. 5(2), 99–114 (1949).
Koo, T. K. & Li, M. Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropractic Med. 15, 155–163 (2016).
Lorensen, W. E. & Cline, H. E. Marching cubes: A high resolution 3D surface construction algorithm. in Proceedings of the 14th Annual Conference on Computer Graphics and Interactive Techniques, SIGGRAPH ’87, 163–169. https://doi.org/10.1145/37401.37422 (ACM, New York, NY, USA, 1987).
Cebral, J. R. & Löhner, R. From medical images to anatomically accurate finite element grids. Int. J. Numer. Methods Eng. 51, 985–1008. https://doi.org/10.1002/nme.205 (2001).
Dhar, S. et al. Morphology parameters for intracranial aneurysm rupture risk assessment. Neurosurgery 63, 185–197. https://doi.org/10.1227/01.NEU.0000316847.64140.81 (2008).
Chien, A. et al. Nonsphericity index and size ratio identify morphologic differences between growing and stable aneurysms in a longitudinal study of 93 cases. Am. J. Neuroradiol. 39, 500–506 (2018).
Yang, J., Li, H., Campbell, D. & Jia, Y. Go-ICP: A globally optimal solution to 3D ICP point-set registration. IEEE Trans. Pattern Anal. Machine Intell. 38, 2241–2254. https://doi.org/10.1109/TPAMI.2015.2513405 (2016).
Besl, P. J. & McKay, N. D. Method for registration of 3-d shapes. Sensor Fusion IV: Control Paradigms Data Structures. 1611, 586–606 (1992).
Yang, J. Go-ICP for globally optimal 3D pointset registration (2023). Original-date: 2018-09-03T05:14:10Z.
Acknowledgements
The authors thank 3DIEMME Srl., for providing the RealGUIDE Software version 5.0. The authors would like to thank A.P. for performing the manual visual assessment and quantification of the aneurysm cases. This work was supported in part by the Slovenian Research Agency (Research Grant nos. J2-2500 and J2-3059
Author information
Authors and Affiliations
Contributions
Ž.B. and Ž.Š. conceived the experiment(s), Ž.B. conducted the experiment(s), Ž.B analysed the results. Both authors contributed to the writing and review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bizjak, Ž., Špiclin, Ž. Aneurysm growth evaluation and detection: a computer-assisted follow-up MRA analysis. Sci Rep 14, 19609 (2024). https://doi.org/10.1038/s41598-024-70453-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-70453-z
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.