Abstract
Hepatocellular carcinoma (HCC) is the most common liver cancer and is among the leading causes of cancer-related death worldwide. There is no reliable biomarker for the early diagnosis of HCC. Circulating microRNAs (miRNAs) have attracted attention as potential biomarkers of disease. By small-RNA next-generation sequencing, the analysis of serum miRNAs led to the identification of molecular signatures able to discriminate advanced HCC from early HCC (n = 246); advanced HCC from CIRRHOSIS (n = 299); advanced HCC from HEALTHY (n = 320); HEALTHY from early HCC (n = 343); and HEALTHY from CIRRHOSIS (n = 414). Cirrhotic patients and early HCC patients exhibited similar serum miRNA profiles, yet a small number of miRNAs (n = 57) were able to distinguish these two classes of patients. A second objective of the study was to identify serum miRNAs capable of predicting the response to therapy in patients with advanced HCC. All patients were treated with sorafenib as first-line therapy: 24 were nonresponsive and 24 responsive. Analysis of circulating miRNAs revealed a 54 miRNAs signature able to separate the two subgroups. This study suggested that circulating miRNAs could be useful biomarkers for monitoring patients with liver diseases ranging from cirrhosis to advanced HCC and possibly predicting susceptibility to first-line treatment based on sorafenib.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC) ranks sixth in incidence and fourth in cancer mortality worldwide1. In recent decades, there has been a significant increase in the incidence of HCC in Western countries2. In addition to hepatitis B and C viral infections, alcohol abuse and nonalcoholic fatty liver disease (NAFLD) are important etiologic factors of HCC3. Cirrhosis is present in 80–90% of patients with HCC and represents the main risk factor4.
The outcome of HCC is generally poor, with a 5-year survival estimated at 70% after curative surgery, only feasible for patients with early-stage HCC, and 3% for those with advanced HCC1. Therapeutic options depend on the stage of cancer. Patients with early-stage HCC are candidates for resection, transplantation and local ablation, while patients with intermediate-stage HCC are candidates for TACE, and those with advanced disease are candidates for systemic therapies5. The treatment of advanced HCC was limited for over a decade to sorafenib6, a multikinase and antiangiogenic inhibitor. Lenvatinib, another multikinase inhibitor in 20187 and the combination of atezolizumab and anti-VEGF agents in 2020 were added as first-line therapies for advanced HCC patients8,9.
Considering that most HCC cases develop in patients with liver cirrhosis or chronic HBV infection, this group of patients represents a category in which surveillance and early diagnosis can potentially be applied. Current diagnostic methods are usually based on noninvasive imaging methods. In a variable percentage of cases, imaging techniques such as ultrasonography or computed tomography (CT) as well as histopathological examination via fine needle biopsy are inconclusive in the diagnostic characterization of small nodules in patients with cirrhosis1, highlighting the need for molecular biomarkers from tissue or liquid biopsies for the early diagnosis of HCC in patients at risk.
Currently, in combination with ultrasound, α-fetoprotein (AFP) is the only circulating biomarker used for the surveillance of HCC. AFP can increase ultrasound sensitivity from 45 to 63%. However, these methods are limited by the low sensitivity of AFP (40–60%) and its variable specificity10,11,12,13. Promising approaches involve the search for circulating genetic biomarkers14. Similarly to other types of tumors, the search for gene mutations in circulating tumor DNA (ctDNA) can allow the detection of patients with early-stage HCC15 or the monitoring of patients during follow-up after tumor resection. Among circulating biomarkers, microRNAs (miRNAs) are of considerable interest. MiRNAs are small noncoding RNAs that regulate gene expression at the posttranscriptional level16,17,18. Attention has been given to potential biomarkers for cancer and other diseases because of their presence and stability in body fluids, such as blood, serum, plasma, and urine19,20. Thus, the search for diagnostic circulating miRNAs has been extensively investigated in different types of tumors, including HCC. For reviews, see18,21,22. These studies highlight the clinical relevance of circulating cell-free miRNAs in cancer18 and more specifically in HCC21,22. Guerriero et al. provide extensive tables summarizing published findings that have addressed diagnostic, prognostic, and predictive circulating miRNAs in HCC21. Very little has been reported on biomarkers for sorafenib responsiveness.
In this study, we searched for molecular signatures of diagnostic value by evaluating the levels of circulating miRNAs in the serum of different patients, from clinically healthy individuals to patients with cirrhosis to patients affected by early or advanced HCC. Moreover, in the case of advanced-stage patients, we evaluated whether circulating miRNAs could predict the response to sorafenib.
Materials and methods
Patients and serum samples
Serum samples from patients with advanced HCC (n = 12), early HCC (n = 11), or cirrhosis (n = 14) and from age- and sex-matched healthy individuals (n = 11) were collected at collaborating clinical facilities (University Hospital of Ferrara, University Hospital S. Orsola, Bologna and University of Milan, Italy) (Table 1). Cirrhosis was diagnosed by laboratory tests, clinical data, imaging techniques according to the EASL guidelines (European Association for the Study of the Liver, Asociación Latinoamericana para el Estudio del Hígado)23. 2D transient elastography of the liver, with values above 15 kPa, confirmed imaging and laboratory findings. Since all patients enrolled in this study had cirrhosis, HCC was diagnosed and staged by imaging techniques (contrast-enhanced multiphasic CT and/or dynamic contrast-enhanced Magnetic Resonance—MRI), according to the 2012 and 2018 guidelines endorsed by the European Association for the Study of the Liver24,25. For staging purposes, CT was extended to the chest. According to the guidelines, diagnosis was based on the typical hallmarks of HCC (hypervascular in the arterial phase with washout in the portal venous or delayed phases). ECOG PS, liver functionality and HCC staging scores, presence of vascular invasion and extrahepatic spread are reported in Table 2. All advanced HCC patients received sorafenib as first-line therapy. Response to treatment was assessed according to RECIST 1.1 criteria26. Healthy controls were collected from age and gender-matched individuals characterized by the absence of liver or other known diseases. Additional cohorts of serum samples from patients with advanced HCC were collected at University Hospital S. Orsola, Bologna (Biotep cohort, n = 12) and at the University Hospital of Milan (MIL cohort, n = 12; MEL cohort, n = 12). All methods were carried out in accordance with relevant guidelines and regulations. The study was approved by the ethical committees of the region Emilia Romagna (AVEC) and of the University Hospital of Milan (n. 496_2019; n. 271/2012/O/Oss; n. 138/2015/O/Tess). Informed consent was obtained from all subjects or their legal guardian(s). Serum samples were all collected at diagnosis, before the start of any therapy. For serum preparation, 5 ml of blood was drawn into a Beckton Dickinson Vacutainer® tube (red cap) with a clotting activator. After the samples had allowed to acclimate to the standing position for 60 min at room temperature, they were centrifuged at 1000×g for 10 min at room temperature. Then, the supernatant was quickly transferred to clean microtubes (400 μl aliquots) and stored at − 80 °C until RNA extraction. Hemolysis was detected by measuring the absorbance at 414 nm using a NanoDrop™ 1000 spectrophotometer (Thermo Fisher Scientific) according to the method described by Shah et al.27; less than 10% of the samples, which exhibited an absorbance > 3.0 were discarded.
microRNA isolation from serum samples
RNA was purified from 400 μl of frozen serum samples using the Maxwell RSC miRNA Plasma and Serum Kit (Promega Italia, Milano, Italy) in an automated Maxwell RSC Instrument (Promega). Purified RNA was collected in 40 μl of deionized sterile water; hence, each μl contained RNA from 10 μl of undiluted serum.
Small RNA library preparation and sequencing
Libraries for NGS were prepared from 5 μl of purified RNA using the QIAseq miRNA Library Kit (Qiagen). Libraries were prepared in accordance with the manufacturer’s instructions for circulating small RNA analysis. Sequencing was performed on a NextSeq500 (Illumina) using a high-output flow-cell (1 × 75 cycles).
NGS data analyses
Raw base-call data generated by the Illumina NextSeq 500 system were demultiplexed and converted to FASTQ format using the Illumina BaseSpace Sequence Hub (https://basespace.illumina.com/home/index). After a quality check with the FastQC tool v.0.11.5 (https://www.bioinformatics.babraham.ac.uk/projects/fastqc), FASTQ files were uploaded to the Qiagen GeneGlobe Data Analysis Center (https://geneglobe.qiagen.com/us/analyze), which performs read mapping and count assignment. A total of 1185 different mature miRNAs were identified (out of 2510, present in database) in at least one of the samples. To allow sample comparison, normalization of raw counts was performed using the DESeq2 bioconductor package v. 1.38.3 (http://bioconductor.org/packages/release/bioc/html/DESeq2.html). Normalized sequencing data were imported and analyzed with Qlucore Omics Explorer analysis software v.3.8 (Qlucore, Lund, Sweden). Differentially expressed miRNAs were identified using ANOVA for multiple groups and t tests for two-group comparisons, with a variable fold change (usually ≥ 1.4) and a Benjamini–Hochberg28 adjusted p value cutoff ≤ 0.01. Similarities between samples were investigated by the use of unsupervised hierarchical clustering and principal component analysis (PCA). In addition, we applied the Prediction Analysis of Microarray (PAM)29, a sample class prediction algorithm as well as a gene selection algorithm based on the “nearest shrunken centroids” analysis of gene expression data. It was applied to assess the probabilities of each sample to belong to each of the investigated classes of samples. miRNA-target interactions and functional enrichment analysis of the differentially expressed miRNAs were performed using miRNet v.2 (https://www.mirnet.ca/)30 in conjunction with the databases miRTarBase31 and Kyoto Encyclopedia of Genes and Genomes (KEGG)32. Functional enrichment analysis were computed applying the Hypergeometric test and pathways were considered significant at p value < 0.05.
Results
Serum miRNAs as diagnostic biomarkers of liver cancer
We measured the levels of miRNAs in the sera of patients (Table 1) with advanced HCC (n = 12), early HCC (n = 11), and cirrhosis (n = 14) and in age- and sex-matched healthy individuals (n = 11) with the aim of determining whether they could represent biomarkers useful for stratifying the different classes of samples.
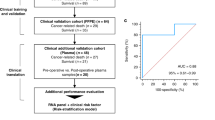
A multigroup analysis (ANOVA) revealed 557 miRNAs (p value < 0.01) (Suppl. Table 1) that could be used to identify three distinct groups via principal component analysis (PCA) and unsupervised hierarchical clustering: one comprising normal individuals, the second comprising advanced HCC patients, and the third comprising heterogeneous samples from cirrhotic or early HCC patients (Fig. 1a,b). Prediction analysis of microarray (PAM) analysis revealed the probability of each sample belonging to one of the four classes of samples: an estimated 100% probability of belonging to the right class for samples from normal individuals and patients with advanced HCC; instead, a mix of probabilities was detected in samples from patients with cirrhosis or early HCC (Supplementary Fig. 1).
Classification of phases of human HCC. (a,b) PCA and unsupervised hierarchical clustering based on serum miRNAs selected by a multigroup analysis (ANOVA) (n = 557 miRNAs, p value < 0.01). Samples were from normal individuals (n = 11) and patients with cirrhosis (n = 14), early HCC (n = 11) or advanced HCC (n = 12). The analyses could visibly separate three groups: normal individuals (Normal), advanced HCC (HCC) and patients with cirrhosis (CE)/early HCC (HCC_early).
To better discriminate between classes of samples, analyses based on two-group comparisons (t test p value < 0.01, fold change > 1.5) revealed lists of miRNAs able to distinguish every single class of samples from each of the others. Table 3 summarizes the results by indicating the number of classified miRNAs and the corresponding supplementary tables. Supplementary Fig. 2 shows the PCA results that illustrate the clear separation of every class of samples from each of the others.
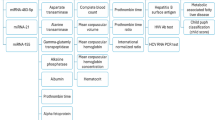
Among the various classes, the transition from cirrhosis to early HCC is the most important, as it represents the key step in the development of a frankly neoplastic disease. This step is clinically and molecularly elusive in most cases, as also apparent from the results of the multigroup analysis, as shown in Fig. 1. The comparison of serum miRNAs between patients with early HCC and patients with cirrhosis allowed us to distinguish two conditions: a panel of 57 miRNAs was capable of separating these very similar patient categories (Fig. 2, Suppl Table 7). To denote method independence, a couple of miRNAs (miR-423-5p and miR-660-5p) were evaluated by quantitative droplet digital PCR (ddPCR) and confirmed the trend of NGS data (Supplementary Fig. 3a,b).
A panel of 57 serum miRNAs differentiates patients affected by early HCC or cirrhosis. The comparison between serum miRNA levels of patients affected by cirrhosis (CE) or early HCC identified a panel of 57 miRNAs (p value < 0.01, FC > 1.33 UP or DOWN) able to classify the two categories of patients, as evidenced by hierarchical clustering and PAM analyses. Albeit with variable probabilities, both analyses correctly classified 100% of the samples. The list of miRNAs is in Suppl Table 7.
The results of these analyses based on serum miRNAs indicate that the quantitative profiles of different miRNA panels can correctly classify the different phases of the disease in the absence of any previous information and that separating patients with cirrhosis in the absence of cancer from patients with early-stage HCC is also possible.
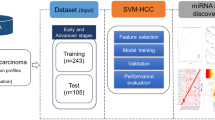
Serum miRNAs as predictive biomarkers of response to sorafenib in advanced HCC patients
Analysis of serum miRNAs was also applied to the search for molecular signatures predictive of response to therapy. A further 12 patients from an independent cohort were added to the 12 patients with advanced-stage HCC included in the previously described diagnostic studies. All patients were treated with sorafenib as first-line therapy. Overall, 12 patients were nonresponsive (NR), and 12 were responsive (R) at the first evaluation two months after the start of therapy. The analysis of circulating miRNAs was applied to these patient cohorts to verify the possibility of distinguishing R patients from NR patients before the start of therapy. The analyses revealed that a panel of 54 miRNAs (fold change > 1.38; p value < 0.01) was able to correctly predict the response to sorafenib in 94% (23 out of 24) of the patients (Fig. 3, Suppl Table 8). The algorithm PAM28 calculates the probability of each sample belonging to one of the classes. This prediction tool correctly classified the same 23 of 24 patients.
A panel of 54 serum miRNAs predicts sorafenib response in patients with advanced HCC. (a,b) PCA and unsupervised hierarchical clustering classified the samples in two main groups, each including either R or NR patients. Overall, 23 of the 24 samples were included in the correct group. (c) Like PCA and clustering analyses, PAM confirmed the good classification prediction of the miRNAs panel, with only LG932 misclassified. Notably, sample LG932 turned out to be NR at the second clinical assessment, 4 months after start of therapy. R = responder; NR = non-responder. The list of miRNAs (p-value < 0.05, FC > 1.35 UP or DOWN) is in Suppl Table 8.
Although the classification was not perfect, the results were very good and suggested that serum miRNAs could be used to stratify the response to sorafenib in the majority of patients before the start of treatment, thus providing a potentially useful tool for a more rational use of therapeutic approaches available against advanced HCC.
To validate the ability of the miRNA signature to predict differential response to sorafenib, we collected 24 additional samples. The validation samples were obtained from independent institutions (12 samples in the MIL5 cohort and 12 samples in the MEL cohort). Data on circulating miRNAs were obtained by NGS as described previously. Then, based on the previously identified 54-miRNA signature, the data were analyzed via PCA, unsupervised hierarchical clustering and PAM analyses (Fig. 4). Discrimination of samples according to R or NR class was very good: excellent on the Biotep and LG cohorts (training sets) and good on the validation sets MEL and MIL5. The statistical performances of the hierarchical clustering and PAM class prediction results are reported in Table 4. A couple of miRNAs (Let7b-5p and miR-16-5p) were also evaluated by quantitative ddPCR and confirmed the trend of NGS data (Supplementary Fig. 3c,d).
Validation of the 54 miRNAs signature on 48 patients with advanced HCC treated with sorafenib as first line therapy. Sera from all patients were collected at diagnosis, before the start of therapy. PCA analysis (a) and unsupervised hierarchical clustering (b) was performed by using the 54 miRNAs signature (Supplementary Table 8) on all 48 samples. The analysis identified two main clusters: one made mainly of R patients; the second mainly of NR patients: overall 41 of 48 patients grouped in the correct cluster. (C) PAM analysis also produced a correct prediction in 41 of 48 patients. Statistical performances of the analyses are shown in Table 3.
Discussion
This study aimed to identify molecular signatures of circulating serum miRNAs able to classify different phases of human HCC.
In this study, we were very careful to ensure that all the samples were treated homogeneously. Attention to technical aspects is important, as it is believed that the known difficulties in reproducing results deriving from studies on circulating miRNAs are not only due to biological heterogeneity but also to small but significant technical differences21. Hence, all preanalytical steps were performed using the same procedures: Blood sampling and serum separation were performed in the same type of BD vacutainer tube, all the serum samples were stored at − 80 °C for several weeks, and the same method and same amount of serum were used for RNA purification of all the serum samples. The sequencing phases employed the same type of reagents for library preparation and NGS sequencing. The analytical steps for counting miRNAs and normalization were carried out simultaneously for all the samples. Therefore, all the statistical comparisons were based on data obtained from samples treated homogeneously in each of the experimental phases. In this way, we planned to decrease the technical variability in the most relevant methodological steps.
The first scientific objective was to identify molecular signatures consisting of circulating serum miRNAs capable of successfully stratifying patients belonging to distinct HCC natural history classes (healthy liver/cirrhosis/early HCC/advanced HCC). Multiple group ANOVA-based analysis could clearly stratify three of the four groups of samples, but it failed to distinguish cirrhotic patients from early HCC patients, the key step in the development of a frankly neoplastic disease. This is not surprising considering that regenerative nodules of a cirrhotic liver and early tumor nodules are not easily distinguishable from a diagnostic point of view. However, an analysis based on two-group comparisons succeeded in identifying a molecular signature composed of 57 miRNAs (p value < 0.01 and fold change > 1.5), which allowed us to differentiate these two classes of patients. Owing to its potential usefulness in the early detection of HCC and the absence of available reliable biomarkers, this finding is of particular clinical value because it might have an impact on the monitoring of cirrhotic patients for the development of HCC in the context of surveillance programs. A number of other studies have previously addressed this question. According to the results reported in the review by Guerriero et al.21, several miRNAs were in common with the results of the analyses in the present study. However, most of them (let-7f., miR-101, miR-106b, miR-181b, miR-125b, miR-145, miR-15, miR-16, miR-221, miR-26a, miR-29a, miR-29c, miR-30e, and miR-96) originate from the comparison of advanced HCC versus cirrhosis, and only a small number (miR-125a-5p, miR-26a and miR-145) originate from the comparison of early HCC versus cirrhosis. This finding is not surprising considering that, in many of the published studies, patients with HCC were likely affected by advanced-stage disease. If a circulating miRNA signature has to be applied for the early detection of liver cancer in cirrhotic patients, this observation is relevant and should not be underestimated. In fact, the results of this study indicated that patients with advanced HCC exhibit profiles of circulating miRNAs that are very different from those of patients with early HCC, which are instead very similar to those of patients with cirrhosis without cancer.
A second objective of the study was to identify serum miRNAs capable of predicting the response to therapy in patients with advanced HCC. All patients with advanced HCC enrolled in the study were treated with sorafenib as first-line therapy. Serum samples from these patients were all collected prior to the start of therapy. A comparison of the NR and R patients revealed a signature consisting of 54 circulating miRNAs able to predict the correct clinical class in most of the patients (88%, 41 out of 48) from 4 different cohorts of patients collected from 3 different institutions. Although a larger series of patients and a prospective study design are needed for translation into clinical application, these findings represent proof of principle of the possibility of applying signatures based on circulating miRNAs to predict the response to therapy in advance. Currently, there are no clinically validated biomarkers for predicting the response to sorafenib33. To date, only a small number of studies have evaluated circulating miRNAs as predictors of sorafenib responsiveness34,35, and a 146-gene signature was associated with improved recurrence-free survival in sorafenib-treated patients36.
While it is noteworthy that the most significant major pathways associated with dysregulated miRNAs (in early HCC versus cirrhosis or in sorafenib responder versus non-responder patients) are linked to cancer, one should be careful in concluding that these pathways reveal the potential biological or molecular mechanisms underlying the classifications, for two main reasons. First, it is unclear whether dysregulated circulating miRNAs can actually influence biological processes as if they were internal to cells. Secondly, dysregulated circulating miRNAs represent a systemic dysregulation, which cannot be attributed to miRNAs released only by tumor cells but also by numerous other types of non-tumor cells (lymphocytes, macrophages, platelets, fibroblasts) which are nevertheless influenced by neoplastic milieu.
While sorafenib was the first treatment for advanced HCC and remains one of the first-line therapies available, other first-line therapies have been added in recent years. The optimal use of these therapeutic options will require predictive diagnostic approaches capable of identifying the best therapy for each patient. The use of circulating miRNAs appears to be one of the most easily and practically feasible possibilities to examine.
In summary, the study revealed miRNA signatures capable of clearly classifying phases of the natural history of human HCC, although the most biologically similar conditions, such as cirrhosis versus early HCC, were more difficult to distinguish, and only a direct comparison revealed a discriminating miRNA signature. Likewise, advanced HCC tumors are biologically very similar, and even in this case, it was difficult to obtain a miRNA signature capable of discriminating differential response to sorafenib. Here, the difficulty was even more accentuated because the model was applied to 4 different cohorts obtained from three different institutions. Overall, the result was very good (41 out of 48 samples were classified correctly), but, in spite of careful homogeneous technical approaches, the classification was not 100% correct. Hence, we concluded that circulating miRNAs represent useful biomarkers for monitoring patients with liver diseases ranging from cirrhosis to advanced HCC and possibly predicting susceptibility to first-line treatment based on sorafenib, but there are still elusive factors attributable to preanalytical steps distinct from each institution that may influence circulating miRNA levels in such a way that renders their use as signatures not yet fully ready for broad clinical use.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Llovet, J. M. et al. Hepatocellular carcinoma. Nat. Rev. Dis. Primers 7, 6. https://doi.org/10.1038/s41572-020-00240-3 (2021).
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2015. CA Cancer J. Clin. 65, 5–29. https://doi.org/10.3322/caac.21254 (2015).
Kulik, L. & El-Serag, H. B. Epidemiology and management of hepatocellular carcinoma. Gastroenterology 156, 477–491. https://doi.org/10.1053/j.gastro.2018.08.065 (2019).
Heidelbaugh, J. J. & Bruderly, M. Cirrhosis and chronic liver failure: Part I. Diagnosis and evaluation. Am. Family Physician 74, 756–762 (2006).
Sidali, S., Trepo, E., Sutter, O. & Nault, J. C. New concepts in the treatment of hepatocellular carcinoma. Unit. Eur. Gastroenterol. J. 10, 765–774. https://doi.org/10.1002/ueg2.12286 (2022).
Llovet, J. M. et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 359, 378–390. https://doi.org/10.1056/NEJMoa0708857 (2008).
Kudo, M. et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet 391, 1163–1173. https://doi.org/10.1016/S0140-6736(18)30207-1 (2018).
Finn, R. S. et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N. Engl. J. Med. 382, 1894–1905. https://doi.org/10.1056/NEJMoa1915745 (2020).
Yang, X., Wang, D., Lin, J., Yang, X. & Zhao, H. Atezolizumab plus bevacizumab for unresectable hepatocellular carcinoma. Lancet. Oncol. 21, e412. https://doi.org/10.1016/S1470-2045(20)30430-7 (2020).
Ahmed Mohammed, H. F. & Roberts, L. R. Should AFP (or any biomarkers) be used for HCC surveillance?. Curr. Hepatol. Rep. 16, 137–145. https://doi.org/10.1007/s11901-017-0349-7 (2017).
Daher, D. et al. Hepatocellular carcinoma surveillance patterns and outcomes in patients with cirrhosis. Clin. Gastroenterol. Hepatol.: Off. Clin. Pract. J. Am. Gastroenterol. Assoc. https://doi.org/10.1016/j.cgh.2023.08.003 (2023).
Tzartzeva, K. et al. Surveillance imaging and alpha fetoprotein for early detection of hepatocellular carcinoma in patients with cirrhosis: A meta-analysis. Gastroenterology 154, 1706–1718. https://doi.org/10.1053/j.gastro.2018.01.064 (2018).
Hu, J. et al. Diagnostic value of alpha-fetoprotein combined with neutrophil-to-lymphocyte ratio for hepatocellular carcinoma. BMC Gastroenterol. 18, 186. https://doi.org/10.1186/s12876-018-0908-6 (2018).
Pan, A., Truong, T. N., Su, Y. H. & Dao, D. Y. Circulating biomarkers for the early diagnosis and management of hepatocellular carcinoma with potential application in resource-limited settings. Diagnostics 13, 676. https://doi.org/10.3390/diagnostics13040676 (2023).
Labgaa, I. et al. A pilot study of ultra-deep targeted sequencing of plasma DNA identifies driver mutations in hepatocellular carcinoma. Oncogene 37, 3740–3752. https://doi.org/10.1038/s41388-018-0206-3 (2018).
Ambros, V. microRNAs: Tiny regulators with great potential. Cell 107, 823–826 (2001).
Calin, G. A. & Croce, C. M. MicroRNA-cancer connection: The beginning of a new tale. Cancer Res. 66, 7390–7394. https://doi.org/10.1158/0008-5472.CAN-06-0800 (2006).
Schwarzenbach, H., Nishida, N., Calin, G. A. & Pantel, K. Clinical relevance of circulating cell-free microRNAs in cancer. Nat. Rev. Clin. Oncol. 11, 145–156. https://doi.org/10.1038/nrclinonc.2014.5[pii] (2014).
Mitchell, P. S. et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc. Natl. Acad. Sci. USA 105, 10513–10518. https://doi.org/10.1073/pnas.0804549105[pii] (2008).
Valadi, H. et al. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell Biol. 9, 654–659. https://doi.org/10.1038/ncb1596 (2007).
Guerriero, P. et al. Circulating tumor DNAs and non-coding RNAs as potential biomarkers for hepatocellular carcinoma diagnosis, prognosis and response to therapy. Hepatoma Res. 5, 6. https://doi.org/10.20517/2394-5079.2018.108 (2019).
Pezzuto, F., Buonaguro, L., Buonaguro, F. M. & Tornesello, M. L. The role of circulating free DNA and MicroRNA in non-invasive diagnosis of HBV- and HCV-related hepatocellular carcinoma. Int. J. Mol. Sci. 19, 1007. https://doi.org/10.3390/ijms19041007 (2018).
European Association for the Study of the Liver. Electronic address, e. e. e., Clinical Practice Guideline, P., Chair, representative, E. G. B. & Panel, m. EASL Clinical Practice Guidelines on non-invasive tests for evaluation of liver disease severity and prognosis - 2021 update. J. Hepatol. 75, 659–689, https://doi.org/10.1016/j.jhep.2021.05.025 (2021).
European Association for the Study of the, L., European Organisation for, R. & Treatment of, C. EASL-EORTC clinical practice guidelines: Management of hepatocellular carcinoma. J. Hepatol. 56, 908–943, https://doi.org/10.1016/j.jhep.2011.12.001 (2012).
European Association for the Study of the Liver. Electronic address, e. e. e. & European Association for the Study of the, L. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 69, 182–236, https://doi.org/10.1016/j.jhep.2018.03.019 (2018).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer 45, 228–247. https://doi.org/10.1016/j.ejca.2008.10.026 (2009).
Shah, J. S., Soon, P. S. & Marsh, D. J. Comparison of methodologies to detect low levels of hemolysis in serum for accurate assessment of serum microRNAs. PLoS ONE 11, e0153200. https://doi.org/10.1371/journal.pone.0153200 (2016).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. B 57, 289–300 (1995).
Tibshirani, R., Hastie, T., Narasimhan, B. & Chu, G. Diagnosis of multiple cancer types by shrunken centroids of gene expression. Proc. Natl. Acad. Sci. USA 99, 6567–6572. https://doi.org/10.1073/pnas.082099299 (2002).
Chang, L., Zhou, G., Soufan, O. & Xia, J. miRNet 2.0: Network-based visual analytics for miRNA functional analysis and systems biology. Nucleic Acids Res. 48, W244–W251. https://doi.org/10.1093/nar/gkaa467 (2020).
Huang, H. Y. et al. miRTarBase update 2022: An informative resource for experimentally validated miRNA-target interactions. Nucleic Acids Res. 50, D222–D230. https://doi.org/10.1093/nar/gkab1079 (2022).
Kanehisa, M., Furumichi, M., Sato, Y., Kawashima, M. & Ishiguro-Watanabe, M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 51, D587–D592. https://doi.org/10.1093/nar/gkac963 (2023).
Gramantieri, L. & Fornari, F. MicroRNAs as predictive biomarkers of treatment response to tyrosine kinase inhibitors in hepatocellular carcinoma: How much is missing?. Oncoscience 9, 52–54. https://doi.org/10.18632/oncoscience.564 (2022).
Nishida, N. et al. MicroRNAs for the prediction of early response to sorafenib treatment in human hepatocellular carcinoma. Liver Cancer 6, 113–125. https://doi.org/10.1159/000449475 (2017).
Fornari, F. et al. In hepatocellular carcinoma miR-221 modulates sorafenib resistance through inhibition of caspase-3-mediated apoptosis. Clin. Cancer Res.: Off. J. Am. Assoc. Cancer Res. 23, 3953–3965. https://doi.org/10.1158/1078-0432.CCR-16-1464 (2017).
Pinyol, R. et al. Molecular predictors of prevention of recurrence in HCC with sorafenib as adjuvant treatment and prognostic factors in the phase 3 STORM trial. Gut 68, 1065–1075. https://doi.org/10.1136/gutjnl-2018-316408 (2019).
Acknowledgements
This work was supported by Associazione Italiana per la Ricerca sul Cancro (to MN), European Programme H2020 MSCA-RISE-2018 n. 824036 (RNADIAGON) (to MN), the University of Ferrara (FAR to MN, SS and EC) and the Italian Ministry of Health n. RC-2023-2778942 (to LG).
Author information
Authors and Affiliations
Contributions
L.D.A., E.C., F.M., P.G., A.M., and F.M. performed the experimental analyses; C.B. performed the statistical and bioinformatics analyses; A.C.G., A.S., and F.P. provided the samples and clinical information; S.S., L.G., and M.N. designed the study and wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
D’Abundo, L., Bassi, C., Callegari, E. et al. Circulating microRNAs as biomarkers for stratifying different phases of liver cancer progression and response to therapy. Sci Rep 14, 18551 (2024). https://doi.org/10.1038/s41598-024-69548-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69548-4
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.