Abstract
The effect of obesity on diabetic retinopathy (DR) has been under scrutiny in recent years. The weight-adjusted waist index (WWI) has been reported to better assess the degree of centripetal obesity in humans, with a higher WWI indicating a higher amount of body fat. The present study is the first to investigate the relationship between WWI and DR and to assess the difference in the predictive ability of WWI and other obesity indices for DR. This cross-sectional study utilized data from the National Health and Nutrition Examination Survey (NHANES) from 2005 to 2008. Researchers collected complete anthropometric data (weight and waist circumference), dilated fundus images, and adult baseline information. Independent interactions between WWI and DR were investigated using multivariate regression and subgroup analyses. In addition, nonlinear associations and threshold effects between WWI and DR were searched for by smoothed curve fitting and by two-stage linear regression modeling. Finally, the receiver operating characteristic curve (ROC) was plotted to compare the predictive power of WWI with other indices of obesity for DR. A total of 1228 eligible patients with diabetes were collected in this study. There were 631 (51.38%) males and 597 (48.62%) females. Among them, 545 (44.38%) were without diabetic retinopathy, 555 (45.20%) had mild diabetic retinopathy, 100 (8.14%) had moderate/severe diabetic retinopathy and 28 (2.28%) had proliferative diabetic retinopathy (PDR). In the fully adjusted model, each unit increase in WWI was associated with a corresponding 31% reduction in the prevalence of DR [OR (95% CI) = 0.69 (0.58, 0.83)]. Compared with subjects in the lowest quartile (quartile 1), subjects in the highest quartile of WWI levels (quartile 4) were 45% less likely to have DR [OR (95% CI) = 0.55 (0.38, 0.78)]. In the case of female participants, a U-shaped correlation was observed between WWI and DR with an inflection point of 11.49. WWI also possesses a better predictive ability for DR compared to obesity indicators such as weight, BMI, and ABSI. This study showed a negative association between WWI and DR in the U.S. population aged 40 years and older.
Similar content being viewed by others
Introduction
The prevalence of diabetes is on the rise, attributed to both the aging of society and the widespread adoption of detrimental lifestyle habits. Diabetes is predicted to affect 592 million people globally by 20351. Diabetic retinopathy (DR) is a common microvascular disease caused by diabetes2. However, diabetic retinopathy progresses slowly before onset, often leading to delays in medical intervention. Such delays may lead to a poor prognosis and severe vision loss at a later stage, thereby affecting quality of life and increasing the socioeconomic burden.3 Therefore, the early prediction and diagnosis of DR are of great clinical significance.
Weight-adjusted waist index (WWI) is considered a novel measure for assessing obesity, which can better differentiate body fat distribution and muscle mass. Compared with magnetic resonance imaging (MRI) and computerized tomography (CT), WWI is less expensive and more acceptable to patients. WWI has become an important reference for the evaluation of systemic and ocular diseases. Although WWI provides excellent predictive value for other chronic diseases4,5,6,7, the relationship between WWI and DR is still unclear, so this study aims to investigate the relationship between the two using data from the National Health and Nutrition Examination Survey (NHANES) to provide new ideas for early prevention and treatment of DR.
Methods
Study population
The current research employs the data obtained from the NHANES to explore the physical health of the US population through questionnaires and physical data measurement to address emerging public health concerns. Through the implementation of stratified multi-stage probability sampling procedures, the sample included is reasonably well represented. By implementing a stratified multi-stage probability sampling procedure, the national population was first stratified by geographic area and demographic characteristics. Within each stratum, Primary Sampling Units (PSUs) are selected first, followed by Secondary Sampling Units (SSUs), and finally, the sampled data are adjusted with weights. These weights take into account sampling design, non-response, and coverage error to make the sample reasonably representative. All NHANES data can be accessed publicly via the official platform: https://www.cdc.gov/nchs/nhanes/. The research was carried out in compliance with the Declaration of Helsinki's guiding principles. The Research Ethics Review Board of the NCHS approved all NHANES study protocols, and written informed consent was obtained from all survey participants. All methods were conducted according to relevant guidelines and regulations.
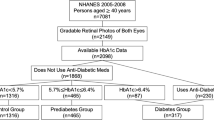
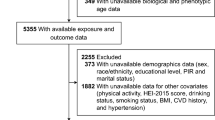
This study comprised a total of 20,497 individuals. To meet the proposed criteria, we eliminated missing weight data (N = 1019;5.0%), missing waist circumference data (N = 2282;11.1%), and missing retinopathy severity class information (N = 11,624;56.7%) from the original sample, as well as those who were not diagnosed with diabetes by a physician in self-report of not being diagnosed with DR at the same time (N = 4344;21.2%), leading us to include a total of 1228 participants in our study (Fig. 1).
Ascertainment of DR
Survey participants aged 40 and above were examined using the Canon Non-Mydriatic Retinal Camera CR6-45NM, which captured 45-degree non-mydriatic digital photos of the retina. Individuals who were blind (with open eyes), had eye infections, or wore eye patches in both eyes were excluded from the retinal imaging component. Each participant will have two fundus images taken of each eye, the first centered on the macula and the second centered on the optic nerve. The grading team includes nine experienced graders, and all technicians have received multi-stage training before data collection, while NCHS staff regularly observe digital imaging exams to review data collection procedures and review grader assessments to ensure reliability during the image collection process. At the University of Wisconsin, two graders independently rated each photograph, and a third grader evaluated the eye if there was disagreement on the pathology between the initial graders. If two out of the three graders failed to agree, an adjudicator made the final decision on the photograph's quality. By looking for the presence of retinal microaneurysms or retinal impression hemorrhages, as well as other retinal lesions (hard exudates, soft exudates, etc.) DR was classified according to the Early Treatment Diabetic Retinopathy Study (ETDRS) grading criteria as absent (grades 10–15), mild nonproliferative DR (NPDR) (grade 20), moderate NPDR (grades 31–43), severe NPDR ( (grades 53–60) and proliferative DR (grades 61–80). When both eyes had retinal images, we evaluated the eye with the more severe retinopathy.
Ascertainment of weight-adjusted-waist index
A new anthropometric measure called the WWI uses body weight and WC to evaluate obesity. It has been discovered that a higher WWI score and a greater degree of obesity are related. Trained health technicians were responsible for obtaining weight and waist circumference information at the MEC. WWI of each individual was computed by taking the waist circumference and dividing it by the square root of the body weight.
Covariates
Covariates in our study included gender, age, race, education level, poverty-income ratio, Smoked at least 100 cigarettes in life, HbA1c, and hypertension status. Those who responded ‘yes’ to the question, "Were you told by a doctor or other health professional that you had hypertension, also called high blood pressure? " were used to define hypertension. People who answered "Yes" to the question "Has your doctor told you that you have diabetes?" were defined as people with diabetes (excluding gestational diabetes). On the website www.cdc.gov/nchs/nhanes/, the public can access all the detailed measurement procedures for the research variables.
Statistical analyses
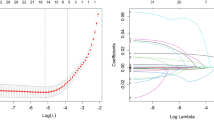
An examination of the association between WWI and DR was conducted by way of multiple logistic regression analysis. The initial model, Model 1, did not control for covariates, while Model 2 adjusted for vital demographic variables, such as age, gender, and race. Model 3 was tailored to account for all covariates scrutinized in this inquiry. To gauge the robustness of the outcomes, a sensitivity analysis was conducted by transforming WWI from a continuous variable to a categorical variable, identifying WWI by quartiles. In addition, subgroup analyses were conducted according to gender, age, and hypertension status to further examine the variables that influence the relationship between WWI and DR. Smoothed curve fitting was performed to find nonlinear associations and saturation effects between WWI and DR. Finally, to find the optimal diagnostic index, we also compared the WWI with the area under the curve (AUC) of the receiver operating characteristic (ROC) for obesity indices such as weight, WHtR, and ABSI. The study set a significance level of 0.05 and was assessed through R (http://www.r-project.org) and EmpowerStats (http://www.empowerstats.com)8.
Results
Baseline characteristics
This study had 1228 individuals in total, 48.62% of whom were female and 51.38% of whom were male. Of these, 683 were patients with diabetic retinopathy, which is about 55.62% of the total number of patients. The quartiles of the WWI were quartile 1 (9.35–10.98), quartile 2 (10.98–11.52), quartile 3 (11.52–11.97) and quartile 4 (11.97–15.39). We found statistically significant differences between WWI quartiles for age, gender, race, education level, HbA1c, poverty income ratio, and hypertension status (all P < 0.05) (Table 1). Compared to the lowest quartile of WWI, the highest quartile of WWI was more likely to be older women with lower educational attainment, and poverty income ratio. There were also higher levels of HbA1c and a higher prevalence of hypertension.
The association between the weight-adjusted-waist index and DR
The correlation between WWI and DR is demonstrated in Table 2. Based on the aforementioned correlation, we have attempted to examine how WWI affected the probability of DR in the research. Specifically, each additional unit in WWI reduces an individual's chances of DR by 31%, a number derived from analysis of the fully adjusted results model. Sensitivity analyses showed that the likelihood of DR was 54% lower in the highest quartile group of WWI compared to the lowest quartile group of WWI and that this negative correlation persisted even after adjusting for all covariates included in the study.
Subgroup analysis
We conducted a stratified analysis by gender, race, and hypertension to further study the variables influencing the association between WWI and the prevalence of DR (Table 3). The results of the subgroup analyses showed that the inverse association between WWI and DR remained significant among men, those without hypertension, and those aged 40 to 59 years, despite accounting for all covariates. Furthermore, in the subgroups stratified by gender, WWI was linearly associated with DR in the male population but not in the female population (Fig. 2). The two-stage linear regression model revealed a U-shaped relationship between WWI and DR in the female population, with an inflection point of 11.49 (Table 4). Specifically, on the left side of the inflection point, WWI was negatively correlated with DR [OR (95% CI) = 0.43 (0.26, 0.71)], and on the right side of the inflection point, WWI was not significantly correlated with DR [OR (95% CI) = 1.20 (0.82, 1.74)].
ROC analysis
The predictive power of WWI for DR was tested by ROC analysis and compared with other indices assessing obesity. For DR risk, the AUC values were WHtR (0.606), WWI (0.592), BMI (0.590), weight (0.563), and ABSI (0.539). The results showed that WWI had a better predictive ability for DR compared to BMI, ABSI, and weight (Fig. 3).
Discussion
A cross-sectional research was conducted, wherein only those individuals who met the nadir criteria, a total of 1228 in number, were deemed eligible and subsequently enlisted. A significant relationship has been shown between a higher WWI index and a lower incidence of DR. Furthermore, a subgroup analysis by gender evinced a curvilinear connection between WWI and DR within the female demographic.
With the growing number of obese people worldwide and the increasing incidence of diseases due to obesity, the economic burden of obesity-related health care continues to increase. Studies show that obesity increases the prevalence of several ailments9,10,11,12. Therefore, more and more indicators are used to assess obesity. The conventional anthropometric measurements utilized in gauging obesity, comprising of BMI and WC, possess inherent limitations about their inability to discriminate between muscle mass and adipose tissue13. This has led many studies based on BMI to propose the "obesity paradox"14,15,16.
The idea of the obesity paradox posits that individuals who are overweight or obese may have a better prognosis than their counterparts of average weight17. A similar phenomenon has been observed in studies using WC18. Park et al. proposed a new obesity index in 2018 and found that WWI was more accurately expressed for morbidity and mortality from obesity-related diseases5. In a study involving 1946 adults, Kim et al. discovered a positive correlation between WWI and the accumulation of belly fat, while conversely observing a negative correlation with abdominal muscle, and this association was not affected by race19. This provides a strong rationale for WWI as a more valid index of obesity.
This study found that WWI was negatively associated with DR, and this association remained even after adjusting for all covariates. This shows a similar trend to previous studies, as Man et al. found that high levels of BMI were protective against DR [OR (95% CI) = 0.46 (0.23, 0.93)], with a 9% reduction in the prevalence of DR for each unit increase in BMI level after adjusting for all covariates [OR (95% CI) = 0.91 ( 0.86, 0.97)]20. Compared with previous studies, this study innovatively used WWI as an indicator to assess the association between obesity and DR, and we further investigated the association between WWI and DR in different populations through subgroup analysis. Specifically, our study not only found a negative association between WWI and DR but also found that the relationship between DR and WWI was gender-specific through subgroup analysis by gender. DR and WWI showed a linear relationship in the male population and a U-shaped relationship in the female population, with an inflection point of 11.46 found by a two-stage linear regression model. This difference has been observed in many previous studies21,22. There are several explanations for this difference, which on the one hand may be related to the way lipids are distributed and stored. It has been found that women's fat is highly malleable and tends to be deposited in the thighs and buttocks more often than men23. On the other hand, it may be related to the metabolism of free fatty acids (FFA). People with diabetes usually have higher levels of FFA, and these fatty acids interfere with insulin signaling, leading to insulin resistance, which in turn affects the development of DR24. Previous studies have found that FFA is metabolized more efficiently in subcutaneous adipose tissue in women compared to men25. In addition, it is interesting to note that on the left side of the inflection point, when WWI was the same, women were less likely to have DR than men. This may be due to the fact that estrogen plays an important role in lipid metabolism and has a protective effect26.
The precise causal relationship between WWI and diabetic retinopathy remains unclear. Several potential pathophysiological pathways may explain this association. First of all, obese people have higher levels of C-peptide27, which has been found to enhance the activity of Na+-K+-ATPase, improve the deformation of erythrocytes in patients with diabetes, and thus enhance microvascular function28. In addition, an animal study found that the capillary filtration coefficient (CFC) of rats injected with C-peptide significantly increased, causing vasodilation and improving microvascular blood flow29, and C-peptide also encouraged the generation of nitric oxide (NO) to enhance endothelial cell activity30,31. Secondly, weight loss occurs due to increased catabolism in patients with diabetes. The majority of individuals diagnosed with DR typically have a prolonged history of diabetes and experience substantial weight loss, which could potentially contribute to the inverse relationship32.
Despite the discovery of a negative correlation between WWI and DR by this particular research, it cannot be assumed that a higher WWI is more beneficial. Previous research has repeatedly demonstrated a substantial correlation between obesity and a higher likelihood of a variety of health problems33. Therefore, close attention should be paid to the body composition of patients in clinical practice to maintain an appropriate fat content. At the same time, the prevention and control of DR in the lean-weight population should not be neglected.
The study has several strengths. First of all, the research sample is more representative since it is based on the NHANES database and incorporates data from a nationwide population sample, and it was designed to account for important covariates. However, the study still has some shortcomings. As a cross-sectional study, we could not determine the causal relationship between WWI and DR. In addition, the study was country and race-specific and it is unclear whether these findings can be validated across other countries and races.
Conclusion
In conclusion, this study found that higher WWI was associated with a lower prevalence of DR and provides a rationale for the possible influence of gender differences in fat distribution on the association with DR prevalence. However, further research is required to corroborate our findings since the pathophysiology of DR is complicated.
Data availability
Publicly available datasets were analyzed in this study. This data can be found here: www.cdc.gov/nchs/nhanes/.
Abbreviations
- DR:
-
Diabetic retinopathy
- WWI:
-
Weight-adjusted waist index
- NHANES:
-
National Health and Nutrition Examination Survey
- WC:
-
Waist circumference
- BMI:
-
Body mass index
- CT:
-
Computerized tomography
- MRI:
-
Magnetic resonance imaging
- ROC:
-
Receiver operating characteristic curve
- CI:
-
Confidence interval
- OR:
-
Odd ratio
References
Guariguata, L. et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res. Clin. Pract. 103, 137–149 (2014).
Dirani, M. et al. Are obesity and anthropometry risk factors for diabetic retinopathy? The diabetes management project. Investig. Ophthalmol. Vis. Sci. 52, 4416–4421 (2011).
Zhou, Y.A.-O., Lu, Q., Zhang, M., Yang, L. & Shen, X. The U-shape relationship between triglyceride-glucose index and the risk of diabetic retinopathy among the US population. J. Pers. Med. 13, 495. https://doi.org/10.3390/jpm13030495 (2023).
Li, Q. et al. Association of weight-adjusted-waist index with incident hypertension: The Rural Chinese Cohort Study. Nutr. Metab. Cardiovasc. Dis. 30, 1732–1741 (2020).
Ding, C. et al. Association of weight-adjusted-waist index with all-cause and cardiovascular mortality in China: A prospective cohort study. Nutr. Metab. Cardiovasc. Dis. 32, 1210–1217 (2022).
Yu, S. et al. Weight-adjusted-waist index predicts newly diagnosed diabetes in Chinese rural adults. J. Clin. Med. 12(4), 1620. https://doi.org/10.3390/jcm12041620 (2023).
Xie, F., Xiao, Y., Li, X. & Wu, Y. Association between the weight-adjusted-waist index and abdominal aortic calcification in United States adults: Results from the national health and nutrition examination survey 2013–2014. Front. Cardiovasc. Med. 9, 948194 (2022).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2015).
Williams, E. P., Mesidor, M., Winters, K., Dubbert, P. M. & Wyatt, S. B. Overweight and obesity: Prevalence, consequences, and causes of a growing public health problem. Curr. Obes. Rep. 4, 363–370 (2015).
Guh, D. P. et al. The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health 9, 1–20 (2009).
Wallace, A.A.-O. et al. Obesity and chronic kidney disease in US adults with type 1 and type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 107, 1247–1256 (2022).
Faulkner, J. L. Obesity-associated cardiovascular risk in women: Hypertension and heart failure. Clin. Sci. 135, 1523–1544 (2021).
Romero-Corral, A. et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int. J. Obes. 32, 959–966 (2008).
Kim, N. H. et al. Body mass index and mortality in the general population and in subjects with chronic disease in Korea: A nationwide cohort study (2002–2010). PLoS ONE 10, e0139924 (2015).
Carnethon, M. R. et al. Association of weight status with mortality in adults with incident diabetes. JAMA 308, 581–590 (2012).
Uretsky, S. et al. Obesity paradox in patients with hypertension and coronary artery disease. Am. J. Med. 120, 863–870 (2007).
Antonopoulos, A. S., Oikonomou, E. K., Antoniades, C. & Tousoulis, D. From the BMI paradox to the obesity paradox: The obesity-mortality association in coronary heart disease. Obes. Rev. 17, 989–1000 (2016).
Clark, A. L., Fonarow, G. C. & Horwich, T. B. Waist circumference, body mass index, and survival in systolic heart failure: The obesity paradox revisited. J. Cardiac Fail. 17, 374–380 (2011).
Kim, N. H., Park, Y., Kim, N. H. & Kim, S. G. Weight-adjusted waist index reflects fat and muscle mass in the opposite direction in older adults. Age Ageing. 50, 780–786 (2021).
Man, R. E. et al. Differential association of generalized and abdominal obesity with diabetic retinopathy in Asian patients with type 2 diabetes. JAMA Ophthalmol. 134, 251–257 (2016).
Shankar, A. et al. Association between body mass index and chronic kidney disease in men and women: Population-based study of Malay adults in Singapore. Nephrol. Dial. Transpl. 23, 1910–1918 (2008).
Qin, Z. et al. The association between weight-adjusted-waist index and increased urinary albumin excretion in adults: A population-based study. Front. Nutr. 9, 941926 (2022).
Frühbeck, G. Bariatric and metabolic surgery: A shift in eligibility and success criteria. Nat. Rev. Endocrinol. 11(8), 465–477 (2015).
Jensen, M. D., Haymond, M. W., Rizza, R. A., Cryer, P. E. & Miles, J. M. Influence of body fat distribution on free fatty acid metabolism in obesity. J. Clin. Investig. 83, 1168–1173 (1989).
Mittendorfer, B., Magkos, F., Fabbrini, E., Mohammed, B. S. & Klein, S. Relationship between body fat mass and free fatty acid kinetics in men and women. Obesity 17, 1872–1877 (2009).
Rettberg, J. R., Yao, J. & Brinton, R. D. Estrogen: A master regulator of bioenergetic systems in the brain and body. Front. Neuroendocrinol. 35, 8–30 (2014).
Ahrén, J., Ahrén, B. & Wierup, N. Increased β-cell volume in mice fed a high-fat diet: A dynamic study over 12 months. Islets. 2, 353–356 (2010).
Forst, T., Kunt, T., Wilhelm, B., Weber, M. M. & Pfützner, A. Role of C-Peptide in the regulation of microvascular blood flow. Exp. Diabetes Res. 2008, 176245 (2008).
Lindström, K., Johansson, C., Johnsson, E. & Haraldsson, B. Acute effects of C-peptide on the microvasculature of isolated perfused skeletal muscles and kidneys in rat. Acta Physiol. Scand. 156, 19–25 (1996).
Wallerath, T. et al. Stimulation of endothelial nitric oxide synthase by proinsulin C-peptide. Nitric Oxide. 9, 95–102 (2003).
Kunt, T. et al. The effect of human proinsulin C-peptide on erythrocyte deformability in patients with Type I diabetes mellitus. Diabetologia. 42, 465–471 (1999).
Chan, J. C. Y. et al. Differential effect of body mass index on the incidence of diabetes and diabetic retinopathy in two Asian populations. Nutr. Diabetes. 8(1), 16 (2018).
Calle, E. E., Rodriguez, C., Walker-Thurmond, K. & Thun, M. J. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N. Engl. J. Med. 348, 1625–1638 (2003).
Acknowledgements
Thanks to all the subjects who participated in this study
Funding
Shandong Province Taishan Scholars Project Special (tsqn202211354), Qian Qiuhai National Famous Elderly Chinese Medicine Experts Inheritance Workshop (National TCM Human Education Letter [2022] No. 75).
Author information
Authors and Affiliations
Contributions
X.L. and M.C. designed the research. X.L. collected, analyzed the data, and drafted the manuscript. X.L., M.C., and Y.H. revised the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, X., Huang, Y. & Chen, M. Correlation of weight-adjusted waist index with diabetic retinopathy in US adults aged ≥ 40 years: the NHANES 2005–2008. Sci Rep 14, 19369 (2024). https://doi.org/10.1038/s41598-024-69404-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69404-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.