Abstract
To investigate whether expression-based polygenic risk scores for the insulin receptor gene network (ePRS-IRs) modifiy the association between type of depressive symptoms and health-related quality of life (HRQoL). This cross-sectional study includes 1558 individuals from the Helsinki Birth Cohort Study. Between 2001 and 2004, the Short Form-36 questionnaire was employed to assess mental and physical components of HRQoL and Beck Depression Inventory (BDI) to assess depressive symptoms. Depressive symptoms were categorized into minimal (BDI < 10), non-melancholic and melancholic types of depression. The ePRS-IRs were calculated for the hippocampal (hePRS-IR) and the mesocorticolimbic (mePRS-IR) regions of the brain. General linear regression models adjusted for age, sex, population stratification, lifestyle factors and body mass index were applied to analyze the data. Both types of depressive symptoms were associated with lower HRQoL (p < 0.0001). HePRS-IR modified the association between the types of depression and mental HRQoL (p for interaction = 0.005). Melancholic type of depressive symptoms was associated with higher mental HRQoL compared to the non-melancholic symptoms among individuals with low hePRS-IR (adjusted mean 4.1, 95% CI 0.7–7.4, p = 0.018). However, no such difference was evident in moderate or high hePRS-IR groups as higher hePRS-IR was associated with lower mental HRQoL (B = − 3.4, 95% CI − 5.6 to − 1.2) in individuals with melancholic type of depressive symptoms. No direct associations were detected between the ePRS-IRs and type of depressive symptoms or HRQoL. Variations in the glucose-insulin metabolism can lower HRQoL in individuals with melancholic depressive symptoms.
Similar content being viewed by others
Introduction
The demographic pyramid is changing and as healthcare and technology advances, humans live longer. However, the prevalence of chronic illnesses originating from unhealthy lifestyles are rapidly growing and as people’s life expectancy increases, the ageing population are faced with inevitable physical as well as mental and social challenges, ultimately affecting their health-related quality of life (HRQoL). For example, studies have reported that poorer HRQoL is commonly seen in individuals with diabetes1,2,3 and depression4. In depressed individuals, greatest reduction in HRQoL is found in those suffering from non-melancholic type of depressive symptoms5.
Depression is often long-lasting and lowers social functioning, working ability and overall HRQoL. Depression has a high comorbidity and is strongly associated with a range of conditions including insulin resistance and metabolic syndrome6,7. Previous studies have shown the importance of distinguishing between types of depression. Non-melancholic depression, characterized by mood reactivity, hypersomnia and weight gain, is associated with metabolic and inflammatory diseases8,9,10 more than melancholic type of depression. Melancholic depression, characterized by anhedonia, insomnia and weight loss, seems to mainly affect the central nervous system and does not associate in the same way with systemic processes10,11.
Depression has been linked to changes in the brain12. Central changes include volumetric reduction of the hippocampus, amygdala, insula, and medial prefrontal cortex13,14, areas which are classically associated with memory, emotion regulation and higher cognitive function15. Functionally, aside from altering the levels of numerous neurotransmitters, depression has also been linked to disturbances in glucose metabolism16. While previously it was thought that the brain was insensitive to insulin, we now know that insulin receptors (IR) play a part in numerous processes in the brain, such as learning, memory and depression17,18,19. IRs are more expressed in neurons than in glia cells, and are present in several locations in the brain including the hypothalamus, hippocampus and cerebral cortex20.
The risk of developing depression is influenced by lifestyle choices, environment, and genetics21. One approach to evaluate the genetic risk, is to convert genetic data from genome wide association studies (GWASs) into polygenic risk scores (PRSs)22. PRSs are traditionally calculated as a weighted sum of discovery GWAS based effect sizes of significant single nucleotide polymorphisms (SNPs)23. The traditional PRSs overlook the fact that genes operate in networks and have tissue specific biological functions. To tackle this shortcoming, a recent study developed novel biologically informed genetic scores for mesocorticolimbic and hippocampal insulin receptor-related gene networks. The expression based, brain region specific PRS for the insulin receptor gene network (ePRS-IR) was more strongly associated with Alzheimer’s disease, addiction and childhood impulsivity than the traditional PRSs24.
Thus far studies have focused on the well-established bidirectional relationship between insulin resistance and depression25. Less is known about the function of the insulin receptor and its effect on depression and HRQoL. The aim of this study is to investigate whether individual differences in the expression of the insulin receptor gene network can modify the relationship between type of depressive symptoms and HRQoL by employing ePRS-IRs.
Research design and methods
Participants
The Helsinki Birth Cohort Study (HBCS) consists of 13,345 individuals born between 1934 and 1944 at the Helsinki University Central Hospital or the Helsinki City Maternity Hospital26. As children, they attended welfare clinics and by1971, they received a unique personal identification number, as did all individuals of the Finnish population27. A baseline clinical examination, involving 2003 randomly selected cohort members, was conducted between 2001 and 2004. After excluding individuals with missing information, 1939 had sufficient information on depressive symptoms and 1930 on HRQoL After deleting duplicates, multiallelic SNPs and ambiguous SNPs, a biologically informed ePRS for the insulin receptor was computed for 1558 of those individuals. The study follows the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of Epidemiology and Public Health of the Hospital District of Helsinki and Uusimaa and that of the National Public Health Institute, Helsinki. All participants gave a written, informed consent.
Health-related quality of life (HRQoL)
HRQoL was assessed using the validated 36-Item Short Form Health Survey (SF 36) version 1.0 questionnaire28. The SF 36 consists of the following eight domains: physical functioning (10 items), role limitations caused by physical health problems (4 items), role limitations caused by emotional health problems (3 items), bodily pain (2 items), general health (5 items), vitality (4 items), mental health (5 items) and social functioning (2 items). Scores for each item ranged from 0 (lowest perceived functioning) to 100 (highest perceived functioning). Based on these scores, physical and mental health component summary (PCS and MCS) scores were calculated using the US reference population (1990) to standardize the eight domains and for factor score coefficients. The summary scores were standardized using a mean of 50 and a standard deviation of 10. The psychometric properties of the Finnish SF-36 have been well validated29.The average age at the time of completing the questionnaire was 61.5 years (SD 2.9).
Depression
Depression symptoms were screened for using the validated 21-item Beck Depression Inventory questionnaire (BDI). Each item was rated by the subjects from 0 to 3 according to how they felt at the moment. Items were summarized as a total BDI score, which can vary between 0 and 63. Scores 10 or higher were considered to indicate depression, as previously suggested30. The subjects with increased depressive symptoms were divided into melancholic and non-melancholic types of depression by comparing the means of summary scores of melancholic and non-melancholic items in BDI. Melancholic items were based on the Diagnostic and Statistical Manual for Mental Disorders (DSM-IV)-defined criteria31. Melancholic symptoms in the BDI included change of sleeping and appetite, feelings of guilt, irritability, loss of interest, loss of pleasure, past failure, punishment feelings and sadness9,32,33,34. Other items in BDI questionnaire were considered the non-melancholic. Subjects were classified to have melancholic type of depression if the mean of the melancholic summary scores were higher than that of the non-melancholic and vice versa. In the case of equal mean of summary scores, subjects were categorized into melancholic subgroups. The Finnish version of the BDI has been reported as reliable and well validated35,36.
Covariates
At the baseline clinical examination, subjects answered questions about their current health situation and lifestyle characteristics. Anthropometrics including weight and height were measured with stadiometers (KaWe) and medical scales (SECA alpha 770), respectively. BMI was calculated as weight in kilograms divided with height in meters squared. Systolic and diastolic blood pressure was measured by a mercury sphygmomanometer from the right arm while the subject was sitting and was recorded as the mean of two successive readings. Smoking was coded as never, former and current, and alcohol use was coded as never or having quit, less than once a week or weekly. Highest attained socioeconomic status, obtained from Statistics Finland, was coded as high official, low official, self-employed and manual workers based on the original classification system37. The cohort members’ past 12-month leisure-time physical activity was assessed using a validated leisure-time physical activity (LTPA) questionnaire; the Kuopio Ischemic Heart Disease Risk Factor Study (KIHD)38. Leisure-time physical activity was measured in metabolic equivalents of task39, which were multiplied with time (hours) and frequency to calculate MET-hours, as previously suggested40. Cohort members were also asked using validated questionnaires about chronic diseases and conditions, including diabetes, cardiovascular conditions (congestive heart failure, arrhythmias, claudication, angina pectoris, previous heart attack and stroke), lung diseases (asthma, emphysema and chronic bronchitis), musculoskeletal disorders (rheumatoid arthritis, osteoporosis) and presence of cancer. The presence of comorbidities was coded as none, one or two or more. Blood samples were obtained to measure levels of total cholesterol, high-density lipoprotein (HDL) cholesterol and triglycerides. A standardized 2-h 75 g oral glucose tolerance test (OGTT) was performed and the World Health Organization (WHO) 2006 criteria41, self-reported, register linkage or usage of medication for diabetes were applied for diagnosing diabetes. Individuals who met the WHO 2006 criteria for impaired glucose tolerance or impaired fasting glucose were grouped together and called prediabetes. Glucose and insulin levels were measured at fasting as well as at 30 min and 2 h. Insulin resistance was determined by the homeostasis model assessment (HOMA), calculated by the formula: (fasting glucose x fasting insulin)/22.542.
Polygenic risk score (PRS)
Genotyping and ePRS-IR calculation was performed as previously described24. DNA was extracted from blood samples and genotyping was performed with the modified Illumina 610 k chip by the Wellcome Trust Sanger Institute, Cambridge, UK, according to standard protocols. Genomic coverage was extended by imputation using the 1000 Genomes Phase I integrated variant set (v3/April 2012; NCBI build 37/hg19) as the reference sample and IMPUTE2 software. Before imputing, quality control filters were applied. Specifically, SNP clustering probability for each genotype was set at > 95%, call rate at > 95% for individuals and markers (99% for markers with minor allele frequency (MAF) < 5%), MAF was set at > 1%, and the p value for the Hardy–Weinberg Equilibrium exact test p > 1 × 10–6. Moreover, heterozygosity, gender check and relatedness checks were performed and any discrepancies removed. The total number of SNPs in the imputed data was 39282668.
For the ePRS calculation, lists of genes co-expressed with the insulin receptor in the mesocorticolimbic system or hippocampus were created. In the original work24, a polygenic risk score for the insulin receptor (PRS-IR) was calculated using SNPs from these gene networks and the association betas from a discovery GWAS (ADHD in the mesocorticolimbic score43 and Alzheimer in the hippocampal score44). In the current study on HBCS, instead of weighing the SNPs by the association with ADHD or Alzheimer, these linkage disequilibria clumped SNPs were weighted with the betas from the Genotype-Tissue Expression (GTeX), a resource database and tissue bank for examining the relationship between genetic variation and gene expression in human tissues. The final lists of SNPs included 16,556 independent functional SNPs for mesocorticolimbic ePRS (from 263 genes) and 30,652 SNPs (from 498 genes) for the hippocampal ePRS. Final ePRSs were obtained by summation over all SNPs accounting for the sign of correlation coefficient between the genes and insulin receptor gene expression in the different regions. Thus, variations in the score used in the current study represent variations in the expression of the insulin receptor gene network in the specific brain region. In other words, a higher score indicates a higher expression of the insulin receptor gene network. The selection of the SNPs within a given clumping window was based on the lowest p-value. As a result, biologically informed mesocorticolimbic (mePRS-IR) and hippocampal (hePRS-IR) specific insulin receptor polygenic risk scores were calculated. For the analyses the PRS-IRs were standardized and reported both as a continuous and a categorical variable (0 = low = < − 0.5 SD, 1 = moderate = − 0.5 to 0.5 SD, and 2 = high = > 0.5 SD).
Statistical analysis
The data are reported in means (standard deviation or 95% confidence intervals), medians (interquartile range) or in counts (percentage). The baseline characteristics were analysed with analysis of variance for continuous variables and chi-square test for categorical variables. General linear models (GLM) allowed us to assess the association between components of HRQoL, types of depression, mePRS-IR, hePRS-IR. GLM were also applied to investigate the depression type by PRS-IRs interaction effect on HRQoL. The regression models were adjusted for age, sex, smoking, alcohol usage, socioeconomic status (SES), presence of chronic diseases, BMI, LTPA and population stratification45,46, as well as for significant interactions between covariates and depression types on HRQoL when applicable. In the case of not meeting the assumptions (e.g. non-normal distribution) bootstrap style analyses (10,000 replications) were applied when analysing the baseline characteristics as well as when applying general linear models. Multinomial logistic regression with bootstrap style analyses (1500 repetitions) was applied to investigate the association between the depression subgroups. Significance level of 0.005 was applied when testing associations between the hePRS-IRs and subgroups of HRQoL. In all other analyses p value of 0.05 was used for statistical significance. Statistical analyses were carried out using Stata/MP version 16.1 (Stata Corporation, College Station, TX, USA).
Results
Our study comprised 1558 subjects, of which 876 (56.2%) were women. The mean age of the participants at the time of the examination was 61.5 years (SD 2.9 for all). Table 1 shows the characteristics of the cohort members according to type of depressive symptoms. Individuals with symptoms of non-melancholic depression suffered more frequently from multiple chronic disease and had higher BMI and blood pressure than individuals with normal BDI score or melancholic type of depressive symptoms.
Both non-melancholic and melancholic depression were associated with lower HRQoL (p < 0.001) (Table 2). A nominally significant association was found between the general health and hePRS-IR (p = 0.04). However, after correcting for multiple testing this association was no longer (Bonferroni corrected p value = 0.40) and no association was found between the hePRS-IR or mePRS-IR and the eight items of HRQoL, MCS, and PCS (Table 3) or type of depression (Table 4, 5). The hePRS-IR was associated with 2 h glucose and insulin concentrations in the OGTT (p values = 0.02 and 0.002, respectively; Table 6), but not with HOMA.
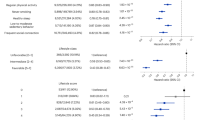
Figures 1 and 2 demonstrate the significant interaction between type of depressive symptoms and hePRS-IR on MCS when analysing hePRS-IR as categorical variable (p for interaction = 0.005), respectively as a continuous variable (p for interaction = 0.008). Regardless of the he-PRS-IR status, both non-melancholic and melancholic were associated with lower MCS compared to the BDI < 10 group (Fig. 1). However, in individuals with low hePRS-IR, melancholic depression was associated with higher MCS (4.1 95% CI 0.7–7.4, p = 0.018) compared to non-melancholic group. No such difference was detected among individuals with moderate or high hePRS-IR groups (p ≥ 0.18) (Fig. 1) as MCS decreased linearly in the melancholic group when applying either categorical (p < 0.001, Fig. 1) or continuous hePRS-IR (p = 0.003, Fig. 2).
The association of the types of depression and mental component score of the SF-36 according to the high/medium/low scores of the biologically informed hippocampal polygenic risk score for the insulin receptor gene network (hePRS-IR). Model adjusted for age, sex and population stratification, smoking, alcohol usage, socioeconomic class, body mass index, leisure-time physical activity and comorbidities. MCS mental component score of the SF-36, hePRS-IR biologically informed hippocampal polygenic risk score for insulin receptor, SD standard deviation, BDI Beck Depression Inventory, BDI < 10 no depression, NMEL non-melancholic depression, Mel Melancholic depression.
Association between the biologically informed hippocampal polygenic risk score for the insulin receptor gene network (hePRS-IR) and mental component score of the SF-36 (MCS) in individuals with no, non-melancholic or melancholic depressive symptoms. Confidence intervals and P-values were based on the bootstrap style method of 10,000 repetitions. (a) BDI < 10. (b) Non-melancholic depressive symptoms. (c) Melancholic depressive symptoms. Model adjusted for age, sex and population stratification, smoking, alcohol usage, socioeconomic class, body mass index, leisure-time physical activity and comorbidities. MCS mental component score of SF-36, BDI Beck Depression Inventory, hePRS-IR biologically informed hippocampal polygenic risk score for insulin receptor, SD standard deviation.
Further adjustment for glucose regulation status did not substantially alter the found association or interactions (p for interaction = 0.009 for continuous hePRS-IR and p for interaction = 0.006 for categorical hePRS-IR).
Our analyses detected no significant association between type of depression by ePRS-IR interaction on PCS (p > 0.05) nor between type of depression and continuous or categorical mePRS-IR on MCS or PCS (p > 0.05).
Discussion
Our findings indicate that higher hippocampal expression of the insulin receptor gene network is associated with lower mental HRQoL specifically in individuals with symptoms of melancholic depression, suggesting that individual differences in the function of the hippocampal insulin receptor gene network can possibly play a role in the relationship between type of depressive symptoms and HRQoL. No evidence of such modifying effect was found for the physical component of HRQoL nor by the mePRS-IR. This lowering effect decreased as the gene expression score decreased, and HRQoL did not distinguishably differ between melancholic and non-melancholic depressive type in individuals with low ePRS-IR. Lower ePRS-IR in itself showed no association with decreased HRQoL nor with any of the two types of depressive symptoms.
The hePRS-IR displayed a significant association with 2 h glucose and insulin concentrations in the OGTT. None of the ePRS-IRs were associated with HOMA. Thus, we showed that the ePRS-IRs measure what they were intended to when they were created, i.e. variations in the glucose insulin metabolism. As such, the application of the ePRSs allowed us to investigate the role of variations in insulin metabolism in specific tissues in individuals regardless of insulin resistance status.
Insulin is considered to be a cognitive modulator47 and disturbances in glucose and insulin metabolism are linked to several psychiatric conditions, including depression16. As established earlier, the ePRS-IRs measure variation in insulin glucose metabolism and not metabolic states such as insulin resistance. This could explain the lack of direct association between the ePRS-IRs and depressive symptoms. Both types of depression were associated with lowered HRQoL regardless of genetic markers for different expression of the insulin receptor gene network. However, individuals with melancholic, but not non-melancholic, depressive symptoms showed a clear descending trend in HRQoL with the hePRS-IR. Previous studies have shown an association between non-melancholic depression and peripheral insulin resistance and metabolic syndrome10,11, while brain insulin sensitivity has been shown to correspond with favourable body fat distribution and weight loss48. The lack of association between non-melancholic depressive symptoms and the ePRS-IRs is compliant with the ePRS-IRs not being associated with HOMA. Individuals with melancholic depression have been found to suffer less frequently from metabolic diseases associated with insulin resistance compared to non-melancholic depression8, which could explain the role of high expression of the insulin receptor gene network on HRQoL in our study.
HRQoL is lower among individuals with peripheral insulin resistance49. According to our results, HRQoL did not display direct association with either of the ePRS-IRs, which suggests that the insulin receptor gene network does not affect HRQoL the same way insulin resistance does. HRQoL has repeatedly been demonstrated to be lowered in depressed individuals50, as was the case in our study. Although the modification of the hePRS-IR was associated with further decreased HRQoL in the melancholic depressive subtype, both subtypes have significantly lower HRQoL compared to the individuals with BDI score < 10.
The modification by a high genetic risk score in depressed individuals was detected only by the hePRS-IR whereas the mePRS-IR did not affect HRQoL. Moreover, only the hePRS-IR was associated with worse glucose metabolism. Studies have suggested that changes in the hippocampal region of the brain play part in the pathophysiology of depression13,14. The mesocorticolimbic region of the brain has previously been considered to be associated primarily with other neuropsychiatric disorders such as ADHD and addiction51. In light of these studies, it can be argued that any modification by high expression of the insulin receptor gene network in depressed individuals would be observed in those with high hePRS-IR, as our results suggest.
The strengths of our study involve the use of the well-characterized HBCS and the use of both clinical and registered-based data in producing our results, as well as the validated SF-36 for assessing HRQoL and the standardized BDI questionnaire for assessing depression. Moreover, the biologically informed ePRS-IR employ whole gene networks instead of single genes, SNPs or discovery GWAS based PRSs to predict risk. However, our cohort is from a homogenous, restricted area in Finland and the findings from this study might therefore have to be cautiously implemented in other populations. Concerning the application of our findings, ePRSs are best utilized in combination with environmental and clinical risk factors when interpreting an individual’s lifetime risk of disease.
In conclusion, a high expression of the insulin receptor gene network is associated with lower mental HRQoL in individuals with symptoms of melancholic depression, suggesting that differences in the function of the insulin receptor share an association with the relationship between type of depressive symptoms and HRQoL.
Data availability
The data analyzed during the current study are available from the corresponding author on reasonable request.
References
Rubin, R. R. & Peyrot, M. Quality of life and diabetes. Diabetes Metab. Res. Rev. 15, 205–218 (1999).
Schanner, C., Falck, A., Keskitalo, A. & Hautala, N. Health-related quality of life of Finnish patients with diabetes. Scand. J. Public Health 44, 765–771. https://doi.org/10.1177/1403494816666732 (2016).
Liu, X. et al. Anxiety and depression in diabetes care: Longitudinal associations with health-related quality of life. Sci. Rep. 10, 8307. https://doi.org/10.1038/s41598-020-57647-x (2020).
Papakostas, G. I. et al. Quality of life assessments in major depressive disorder: A review of the literature. Gen. Hosp. Psychiatry 26, 13–17. https://doi.org/10.1016/j.genhosppsych.2003.07.004 (2004).
Selenius, J. S. et al. Impaired glucose regulation, depressive symptoms, and health-related quality of life. BMJ Open Diabetes Res. Care 8, e001568. https://doi.org/10.1136/bmjdrc-2020-001568 (2020).
Anderson, R. J., Freedland, K. E., Clouse, R. E. & Lustman, P. J. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care 24, 1069–1078 (2001).
Kan, C. et al. A systematic review and meta-analysis of the association between depression and insulin resistance. Diabetes Care 36, 480–489. https://doi.org/10.2337/dc12-1442 (2013).
Takeuchi, T., Nakao, M., Kachi, Y. & Yano, E. Association of metabolic syndrome with atypical features of depression in Japanese people. Psychiatry Clin. Neurosci. 67, 532–539. https://doi.org/10.1111/pcn.12104 (2013).
Seppala, J. et al. Prevalence of metabolic syndrome in subjects with melancholic and non-melancholic depressive symptoms. A Finnish population-based study. J. Affect. Disord. 136, 543–549. https://doi.org/10.1016/j.jad.2011.10.032 (2012).
Penninx, B. W., Milaneschi, Y., Lamers, F. & Vogelzangs, N. Understanding the somatic consequences of depression: Biological mechanisms and the role of depression symptom profile. BMC Med. 11, 129. https://doi.org/10.1186/1741-7015-11-129 (2013).
Lamers, F. et al. Evidence for a differential role of HPA-axis function, inflammation and metabolic syndrome in melancholic versus atypical depression. Mol. Psychiatry 18, 692–699. https://doi.org/10.1038/mp.2012.144 (2013).
Liu, W. et al. The role of neural plasticity in depression: From hippocampus to prefrontal cortex. Neural Plast. 2017, 6871089. https://doi.org/10.1155/2017/6871089 (2017).
Stratmann, M. et al. Insular and hippocampal gray matter volume reductions in patients with major depressive disorder. PLoS One 9, e102692–e102692. https://doi.org/10.1371/journal.pone.0102692 (2014).
Belleau, E. L., Treadway, M. T. & Pizzagalli, D. A. The Impact of stress and major depressive disorder on hippocampal and medial prefrontal cortex morphology. Biol. Psychiatr. 85, 443–453. https://doi.org/10.1016/j.biopsych.2018.09.031 (2019).
Pandya, M., Altinay, M., Malone, D. A. Jr. & Anand, A. Where in the brain is depression?. Curr. Psychiatry Rep. 14, 634–642. https://doi.org/10.1007/s11920-012-0322-7 (2012).
Zou, X. H., Sun, L. H., Yang, W., Li, B. J. & Cui, R. J. Potential role of insulin on the pathogenesis of depression. Cell Prolif. 53, e12806. https://doi.org/10.1111/cpr.12806 (2020).
Dou, J.-T., Chen, M., Dufour, F., Alkon, D. L. & Zhao, W.-Q. Insulin receptor signaling in long-term memory consolidation following spatial learning. Learn. Mem. 12, 646–655. https://doi.org/10.1101/lm.88005 (2005).
Akhtar, A. & Sah, S. P. Insulin signaling pathway and related molecules: Role in neurodegeneration and Alzheimer’s disease. Neurochem. Int. 135, 104707. https://doi.org/10.1016/j.neuint.2020.104707 (2020).
Frangou, S. et al. Insulin resistance: Genetic associations with depression and cognition in population based cohorts. Exp. Neurol. 316, 20–26. https://doi.org/10.1016/j.expneurol.2019.04.001 (2019).
Pomytkin, I. et al. Insulin receptor in the brain: Mechanisms of activation and the role in the CNS pathology and treatment. CNS Neurosci. Ther. 24, 763–774. https://doi.org/10.1111/cns.12866 (2018).
Moazzam-Jazi, M., Najd Hassan Bonab, L., Zahedi, A. S. & Daneshpour, M. S. High genetic burden of type 2 diabetes can promote the high prevalence of disease: A longitudinal cohort study in Iran. Sci. Rep. 10, 14006. https://doi.org/10.1038/s41598-020-70725-4 (2020).
Lewis, C. M. & Vassos, E. Polygenic risk scores: From research tools to clinical instruments. Genome Med. 12, 44. https://doi.org/10.1186/s13073-020-00742-5 (2020).
Choi, S. W., Heng Mak, T. S. & O’Reilly, P. F. A guide to performing Polygenic Risk Score analyses. biorxiv https://doi.org/10.1101/416545 (2018).
Hari Dass, S. A. et al. A biologically-informed polygenic score identifies endophenotypes and clinical conditions associated with the insulin receptor function on specific brain regions. EBioMedicine 42, 188–202. https://doi.org/10.1016/j.ebiom.2019.03.051 (2019).
Mezuk, B., Eaton, W. W., Albrecht, S. & Golden, S. H. Depression and type 2 diabetes over the lifespan: A meta-analysis. Diabetes Care 31, 2383–2390. https://doi.org/10.2337/dc08-0985 (2008).
von Bondorff, M. B. et al. Early life origins of all-cause and cause-specific disability pension: Findings from the Helsinki Birth Cohort Study. PLoS One 10, e0122134. https://doi.org/10.1371/journal.pone.0122134 (2015).
Eriksson, J. G., Kajantie, E., Lampl, M. & Osmond, C. Trajectories of body mass index amongst children who develop type 2 diabetes as adults. J. Intern. Med. 278, 219–226. https://doi.org/10.1111/joim.12354 (2015).
Ware, J. E. Jr. & Sherbourne, C. D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 30, 473–483 (1992).
Aalto, A.-M., Aro, A. R. & Teperi, J. RAND-36 as a measure of Health-Related Quality of Life. Reliability, construct validity and reference values in the Finnish general population. Stakes Res. Rep. 101, 2 (1999).
Beck, A. T., Steer, R. A. & Garbin, M. G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 8, 77–100. https://doi.org/10.1016/0272-7358(88)90050-5 (1988).
Sheehan, D. V. et al. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 5920, 22–33 (1998).
Vanhala, M., Jokelainen, J., Keinanen-Kiukaanniemi, S., Kumpusalo, E. & Koponen, H. Depressive symptoms predispose females to metabolic syndrome: A 7-year follow-up study. Acta Psychiatr. Scand. 119, 137–142. https://doi.org/10.1111/j.1600-0447.2008.01283.x (2009).
Sheehan, D. V. & Lecrubie, L. The Mini-International Neuropsychiatric Interview (MINI) (University of South Florida, Institute for Research in Psychiatry; Paris: INSERM‐Hopital de la Salpetriere, 1994).
Steer, R. A., Ball, R., Ranieri, W. F. & Beck, A. T. Dimensions of the Beck Depression Inventory-II in clinically depressed outpatients. J. Clin. Psychol. 55, 117–128 (1999).
Viinamäki, H. et al. Is the Beck Depression Inventory suitable for screening major depression in different phases of the disease?. Nord J. Psychiatry 58, 49–53. https://doi.org/10.1080/08039480310000798 (2004).
Wang, Y. P. & Gorenstein, C. Psychometric properties of the Beck Depression Inventory-II: A comprehensive review. Braz. J. Psychiatry 35, 416–431. https://doi.org/10.1590/1516-4446-2012-1048 (2013).
Central Statistical Office of Finland. Classification of Socio-economic Group: Handbooks 17. Helsinki. (1989).
Lakka, T. A. et al. Relation of leisure-time physical activity and cardiorespiratory fitness to the risk of acute myocardial infarction. N. Engl. J. Med. 330, 1549–1554. https://doi.org/10.1056/nejm199406023302201 (1994).
Alberti, K. G. & Zimmet, P. Z. Definition, diagnosis and classification of diabetes mellitus and its complications Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabetic Med. J. Brit. Diabetic Assoc. 15, 539–553. https://doi.org/10.1002/(sici)1096-9136(199807)15:7%3c539::Aid-dia668%3e3.0.Co;2-s (1998).
Wasenius, N. et al. Unfavorable influence of structured exercise program on total leisure-time physical activity. Scand. J. Med. Sci. Sports 24, 404–413. https://doi.org/10.1111/sms.12015 (2014).
World Health Organization. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia (World Health Organization, 2006).
Matthews, D. R. et al. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419. https://doi.org/10.1007/bf00280883 (1985).
Neale, B. M. et al. Meta-analysis of genome-wide association studies of attention-deficit/hyperactivity disorder. J. Am. Acad. Child Adolesc. Psychiatry 49, 884–897. https://doi.org/10.1016/j.jaac.2010.06.008 (2010).
Lambert, J.-C. et al. Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer’s disease. Nat. Genet. 45, 1452–1458. https://doi.org/10.1038/ng.2802 (2013).
Price, A. L. et al. Principal components analysis corrects for stratification in genome-wide association studies. Nat. Genet. 38, 904–909. https://doi.org/10.1038/ng1847 (2006).
Patterson, N., Price, A. L. & Reich, D. Population structure and eigenanalysis. PLoS Genet. 2, e190–e190. https://doi.org/10.1371/journal.pgen.0020190 (2006).
McNay, E. C. & Recknagel, A. K. Brain insulin signaling: A key component of cognitive processes and a potential basis for cognitive impairment in type 2 diabetes. Neurobiol. Learn. Mem. 96, 432–442. https://doi.org/10.1016/j.nlm.2011.08.005 (2011).
Kullmann, S. et al. Brain insulin sensitivity is linked to adiposity and body fat distribution. Nat. Commun. 11, 1841–1841. https://doi.org/10.1038/s41467-020-15686-y (2020).
Schlotz, W. et al. Specific associations of insulin resistance with impaired health-related quality of life in the Hertfordshire Cohort Study. Q. Life Res. Int. J. Qual. Life Aspects Treat. Care Rehabil. 16, 429–436. https://doi.org/10.1007/s11136-006-9129-5 (2007).
Sivertsen, H., Bjørkløf, G. H., Engedal, K., Selbæk, G. & Helvik, A. S. Depression and quality of life in older persons: A review. Dement. Geriatr. Cogn. Disord. 40, 311–339. https://doi.org/10.1159/000437299 (2015).
Sharma, A. & Couture, J. A review of the pathophysiology, etiology, and treatment of attention-deficit hyperactivity disorder (ADHD). Ann. Pharmacother. 48, 209–225. https://doi.org/10.1177/1060028013510699 (2014).
Acknowledgements
The authors would like to express their gratitude to the participants in the Helsinki Birth Cohort Study. Also special thanks for the funding of the HBCS to the Finnish Foundation for Cardiovascular Research, Finnish Foundation for Diabetes Research, Juho Vainio Foundation, Academy of Finland, Novo Nordisk Foundation, Signe and Ane Gyllenberg Foundation, Samfundet Folkhälsan, Finska Läkaresällskapet, Liv och Hälsa, European Commission FP7 (DORIAN) Grant Agreement No. 278603 and EU H2020-PHC-2014-DynaHealth Grant No. 633595 and EU Horizon 2020 Award 733206 LIFECYCLE. Silveira PP is supported by Canadian Institutes of Health Research (CIHR, PJT-166066, PI Silveira PP).
Author information
Authors and Affiliations
Contributions
J.S. and N.W. researched data, contributed to discussion, and J.S wrote the manuscript. P.S. and J.L. researched data, contributed to discussion and reviewed/edited the manuscript. M.S., H.K., M.B. and E.K. contributed to discussion and reviewed/edited the manuscript. J.E. contributed to discussion and reviewed/edited the manuscript. All authors contributed substantially to the conception and design or analysis and interpretation of data and the drafting of the article or critical revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Selenius, J.S., Silveira, P.P., Salonen, M. et al. The relationship between health-related quality of life and melancholic depressive symptoms is modified by brain insulin receptor gene network. Sci Rep 11, 21588 (2021). https://doi.org/10.1038/s41598-021-00631-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-00631-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.