Abstract
A randomized, double-blind, placebo-controlled, 52-week study (no. NCT03068468) evaluated gosuranemab, an anti-tau monoclonal antibody, in the treatment of progressive supranuclear palsy (PSP). In total, 486 participants dosed were assigned to either gosuranemab (n = 321) or placebo (n = 165). Efficacy was not demonstrated on adjusted mean change of PSP Rating Scale score at week 52 between gosuranemab and placebo (10.4 versus 10.6, P = 0.85, primary endpoint), or at secondary endpoints, resulting in discontinuation of the open-label, long-term extension. Unbound N-terminal tau in cerebrospinal fluid decreased by 98% with gosuranemab and increased by 11% with placebo (P < 0.0001). Incidences of adverse events and deaths were similar between groups. This well-powered study suggests that N-terminal tau neutralization does not translate into clinical efficacy.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
To request access to data, please visit http://www.biogenclinicaldatarequest.com. The individual participant data collected during the trial and that support the research proposal will be available to qualified scientific researchers after anonymization and following approval of the research proposal. Anonymization of the datasets is necessary to allow sharing of data ethically and legally, and to maximize their significant social, environmental and economic value while preserving the confidentiality of the individuals who participated in studies conducted by Biogen. An initial status update of the request will take approximately two (2) business days after the request’s submission date. The requester will be notified of the outcome of the request in approximately thirty (30) business days. Source data are provided with this paper.
Change history
17 October 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41591-022-02076-8
References
Boxer, A. L. et al. Advances in progressive supranuclear palsy: new diagnostic criteria, biomarkers, and therapeutic approaches. Lancet Neurol. 16, 552–563 (2017).
Höglinger, G. U. et al. Clinical diagnosis of progressive supranuclear palsy: the movement disorder society criteria. Mov. Disord. 32, 853–864 (2017).
Picillo, M. et al. Motor, cognitive and behavioral differences in MDS PSP phenotypes. J. Neurol. 266, 1727–1735 (2019).
Golbe, L. I. Progressive supranuclear palsy. Semin. Neurol. 34, 151–159 (2014).
Litvan, I. et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele–Richardson–Olszewski syndrome): report of the NINDS-SPSP international workshop. Neurology 47, 1–9 (1996).
Golbe, L. I. & Ohman-Strickland, P. A. A clinical rating scale for progressive supranuclear palsy. Brain 130, 1552–1565 (2007).
Respondek, G. et al. Accuracy of the National Institute for Neurological Disorders and Stroke/Society for Progressive Supranuclear Palsy and neuroprotection and natural history in Parkinson plus syndromes criteria for the diagnosis of progressive supranuclear palsy. Mov. Disord. 28, 504–509 (2013).
Dickson, D. W., Ahmed, Z., Algom, A. A., Tsuboi, Y. & Josephs, K. A. Neuropathology of variants of progressive supranuclear palsy. Curr. Opin. Neurol. 23, 394–400 (2010).
Dickson, D. W. Parkinson’s disease and parkinsonism: neuropathology. Cold Spring Harb. Perspect. Med. 2, a009258 (2012).
Fuster-Matanzo, A., Hernández, F. & Ávila, J. Tau spreading mechanisms; implications for dysfunctional tauopathies. Int. J. Mol. Sci. 19, 645 (2018).
Meredith, J. E. Jr. et al. Characterization of novel CSF tau and ptau biomarkers for Alzheimer’s disease. PLoS One 8, e76523 (2013).
Bright, J. et al. Human secreted tau increases amyloid-beta production. Neurobiol. Aging 36, 693–709 (2015).
Sato, C. et al. Tau kinetics in neurons and the human central nervous system. Neuron 97, 1284–1298 (2018).
Clavaguera, F. et al. Brain homogenates from human tauopathies induce tau inclusions in mouse brain. Proc. Natl Acad. Sci. USA 110, 9535–9540 (2013).
Mocanu, M. M. et al. The potential for beta-structure in the repeat domain of tau protein determines aggregation, synaptic decay, neuronal loss, and coassembly with endogenous tau in inducible mouse models of tauopathy. J. Neurosci. 28, 737–748 (2008).
Sanders, D. W. et al. Distinct tau prion strains propagate in cells and mice and define different tauopathies. Neuron 82, 1271–1288 (2014).
Golonzhka, O. et al. Functional characterization of anti-tau monoclonal antibody BIIB092. Presented at 14th International Conference on Alzheimer’s and Parkinson’s Diseases (26–31 March, 2019, Lisbon, Portugal).
Czerkowicz, J. et al. Pharmacokinetic and target engagement analysis of anti-tau antibody gosuranemab [BIIB092] in cynomolgus monkey central nervous system fluid compartments. Alzheimers Dement. 15, 1288–1289 (2019).
Qureshi, I. A. et al. A randomized, single ascending dose study of intravenous BIIB092 in healthy participants. Alzheimers Dement. 4, 746–755 (2018).
Boxer, A. L. et al. Safety of the tau-directed monoclonal antibody BIIB092 in progressive supranuclear palsy: a randomised, placebo-controlled, multiple ascending dose phase 1b trial. Lancet Neurol. 18, 549–558 (2019).
Boxer, A. L. et al. Davunetide in patients with progressive supranuclear palsy: a randomised, double-blind, placebo-controlled phase 2/3 trial. Lancet Neurol. 13, 676–685 (2014).
Papapetropoulos, S., Singer, C., McCorquodale, D., Gonzalez, J. & Mash, D. C. Cause, seasonality of death and co-morbidities in progressive supranuclear palsy (PSP). Parkinsonism Relat. Disord. 11, 459–463 (2005).
Höglinger, G. U. et al. Longitudinal magnetic resonance imaging in progressive supranuclear palsy: a new combined score for clinical trials. Mov. Disord. 32, 842–852 (2017).
Whitwell, J. L. et al. Radiological biomarkers for diagnosis in PSP: where are we and where do we need to be? Mov. Disord. 32, 955–971 (2017).
Josephs, K. A. et al. Modeling trajectories of regional volume loss in progressive supranuclear palsy. Mov. Disord. 28, 1117–1124 (2013).
Tsai, R. M. et al. Clinical correlates of longitudinal brain atrophy in progressive supranuclear palsy. Parkinsonism Relat. Disord. 28, 29–35 (2016).
Tolosa, E. et al. A phase 2 trial of the GSK-3 inhibitor tideglusib in progressive supranuclear palsy. Mov. Disord. 29, 470–478 (2014).
Doble, A. The pharmacology and mechanism of action of riluzole. Neurology 47, S233–S241 (1996).
Bensimon, G. et al. Riluzole treatment, survival and diagnostic criteria in Parkinson plus disorders: the NNIPPS study. Brain 132, 156–171 (2009).
Vaswani, P. A. & Olsen, A. L. Immunotherapy in progressive supranuclear palsy. Curr. Opin. Neurol. 33, 527–533 (2020).
Schrag, A. et al. Measuring quality of life in PSP: the PSP-QoL. Neurology 67, 39–44 (2006).
Goetz, C. G. et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov. Disord. 23, 2129–2170 (2008).
Shoeibi, A. et al. Are the International Parkinson disease and Movement Disorder Society progressive supranuclear palsy (IPMDS-PSP) diagnostic criteria accurate enough to differentiate common PSP phenotypes? Parkinsonism Relat. Disord. 69, 34–39 (2019).
Respondek, G. et al. The phenotypic spectrum of progressive supranuclear palsy: a retrospective multicenter study of 100 definite cases. Mov. Disord. 29, 1758–1766 (2014).
Martínez-Martín, P. et al. Parkinson’s disease severity levels and MDS-Unified Parkinson’s Disease Rating Scale. Parkinsonism Relat. Disord. 21, 50–54 (2015).
Busner, J. & Targum, S. D. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry 4, 28–37 (2007).
Mamarabadi, M., Razjouyan, H. & Golbe, L. I. Is the latency from progressive supranuclear palsy onset to diagnosis improving? Mov. Disord. Clin. Pract. 5, 603–606 (2018).
Armstrong, R. A. Visual signs and symptoms of progressive supranuclear palsy. Clin. Exp. Optom. 94, 150–160 (2011).
Respondek, G. et al. Which ante mortem clinical features predict progressive supranuclear palsy pathology? Mov. Disord. 32, 995–1005 (2017).
Ali, F. et al. Sensitivity and specificity of diagnostic criteria for progressive supranuclear palsy. Mov. Disord. 34, 1144–1153 (2019).
Höglinger, G. U. et al. Identification of common variants influencing risk of the tauopathy progressive supranuclear palsy. Nat. Genet. 43, 699–705 (2011).
Sopko, R. et al. Characterization of tau binding by gosuranemab. Neurobiol. Dis. 146, 105120 (2020).
Bright, J. et al. Human secreted tau increases amyloid-beta production. Neurobiol. Aging 36, 693–709 (2015).
Gómez-Ramos, A., Díaz-Hernández, M., Cuadros, R., Hernández, F. & Avila, J. Extracellular tau is toxic to neuronal cells. FEBS Lett. 580, 4842–4850 (2006).
Gómez-Ramos, A., Díaz-Hernández, M., Rubio, A., Miras-Portugal, M. T. & Avila, J. Extracellular tau promotes intracellular calcium increase through M1 and M3 muscarinic receptors in neuronal cells. Mol. Cell. Neurosci. 37, 673–681 (2008).
Gibbons, G. S., Lee, V. M. Y. & Trojanowski, J. Q. Mechanisms of cell-to-cell transmission of pathological tau: a review. JAMA Neurol. 76, 101–108 (2019).
Yamada, K. Extracellular tau and its potential role in the propagation of tau pathology. Front. Neurosci. 11, 667 (2017).
Courade, J. P. et al. Epitope determines efficacy of therapeutic anti-tau antibodies in a functional assay with human Alzheimer tau. Acta Neuropathol. 136, 729–745 (2018).
Guo, J. L. et al. Unique pathological tau conformers from Alzheimer’s brains transmit tau pathology in nontransgenic mice. J. Exp. Med. 213, 2635–2654 (2016).
Czerkowicz, J. et al. Anti-tau antibody BIIB092 binds secreted tau in preclinical models and Alzheimer’s disease cerebrospinal fluid. Alzheimers Dement. 14, P1441 (2018); https://alz-journals.onlinelibrary.wiley.com/doi/10.1016/j.jalz.2018.06.2423
Scheres, S. H., Zhang, W., Falcon, B. & Goedert, M. Cryo-EM structures of tau filaments. Curr. Opin. Struct. Biol. 64, 17–25 (2020).
Höglinger, G. U. et al. Safety and efficacy of tilavonemab in progressive supranuclear palsy: a phase 2, randomised, placebo-controlled trial. Lancet Neurol. 20, 182–192 (2021).
Hall, S. et al. Cerebrospinal fluid concentrations of inflammatory markers in Parkinson’s disease and atypical parkinsonian disorders. Sci. Rep. 8, 13276 (2018).
Hall, S. et al. Accuracy of a panel of 5 cerebrospinal fluid biomarkers in the differential diagnosis of patients with dementia and/or parkinsonian disorders. Arch. Neurol. 69, 1445–1452 (2012).
Wagshal, D. et al. Divergent CSF τ alterations in two common tauopathies: Alzheimer’s disease and progressive supranuclear palsy. J. Neurol. Neurosurg. Psychiatry 86, 244–250 (2015).
Kovacs, G. G. Invited review: neuropathology of tauopathies: principles and practice. Neuropathol. Appl. Neurobiol. 41, 3–23 (2015).
Shoeibi, A., Olfati, N. & Litvan, I. Preclinical, phase I, and phase II investigational clinical trials for treatment of progressive supranuclear palsy. Expert Opin. Investig. Drugs 27, 349–361 (2018).
Grimm, M. J. et al. Movement Disorder Society-Endorsed PSP Study Group. Clinical conditions ‘suggestive of progressive supranuclear palsy’—diagnostic performance. Mov. Disord. https://doi.org/10.1002/mds.28263 (2020).
D’Elia, L. F., Satz, P., Uchiyama, C. L. & White, T. Color Trails Test. Professional Manual (Psychological Assessment Resources, 1996).
Wolz, R., Aljabar, P., Hajnal, J. V., Hammers, A. & Rueckert, D. LEAP: learning embeddings for atlas propagation. Neuroimage 49, 1316–1325 (2010).
Guy, W. ECDEU Assessment Manual for Psychopharmacology (US Department of Health, Education, and Welfare, 1976).
Karantzoulis, S., Novitski, J., Gold, M. & Randolph, C. The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS): utility in detection and characterization of mild cognitive impairment due to Alzheimer’s disease. Arch. Clin. Neuropsychol. 28, 837–844 (2013).
Dal Bello-Haas, V., Klassen, L., Sheppard, M. S. & Metcalfe, A. Psychometric properties of activity, self-efficacy, and quality-of-life measures in individuals with Parkinson disease. Physiother. Can. 63, 47–57 (2011).
Miller, E. Verbal fluency as a function of a measure of verbal intelligence and in relation to different types of cerebral pathology. Br. J. Clin. Psychol. 23, 53–57 (1984).
Stamelou, M. et al. Power calculations and placebo effect for future clinical trials in progressive supranuclear palsy. Mov. Disord. 31, 742–747 (2016).
Acknowledgements
We thank Biogen (Cambridge, MA, USA), who sponsored this study and provided medical writing and editorial support for the development of this publication. We thank S. Douthwaite and M. Mandle (Excel Medical Affairs, Fairfield, CT, USA), who wrote the first draft of the manuscript based on input from the authors, and J. Parker (Excel Medical Affairs, Horsham, UK), who copyedited and styled the manuscript according to journal requirements. Biogen reviewed and provided feedback on the paper to the authors. All authors had full access to the study data, contributed to data interpretation and manuscript development, provided final approval for submission and take responsibility for data completeness and accuracy. The corresponding author had final responsibility for the decision to submit for publication. We thank the patients with PSP who participated in the PASSPORT trial, their families, the PASSPORT study group investigators and the clinical research centers where the study occurred. This research was carried out in part by the National Institutes for Health Research (NIHR) UCLH Clinical Research Facility in the United Kingdom. We also thank T. Olsson and M. Tighe for their contributions to the study design, and V. Kurnala (lead statistical programmer for the study) for his contribution to data analysis.
Author information
Authors and Affiliations
Consortia
Contributions
T.D. performed data analysis, interpretation and writing of the manuscript. A.L.B. carried out study design, data collection, data analysis, data interpretation, participant recruitment and writing of the report. L.I.G. oversaw development and implementation of the primary endpoint instrument, study design, participant recruitment, data collection, data interpretation, writing of the report and approval of the final version of the manuscript. G.U.H. performed study design, participant recruitment, data collection, data interpretation, writing of the report and approval of the final version of the manuscript. H.R.M. carried out study design, data collection, data interpretation, participant recruitment and critical review of the report. I.L. was responsible for study design, data collection, data interpretation, participant recruitment and critical review of the report. A.E.L. performed study design, data analysis, data interpretation, review of the manuscript and approval of the final version of the manuscript. J.-C.C. oversaw study design, data collection, data interpretation, participant recruitment and reviewing the manuscript. I.A. was responsible for study design, participant recruitment, data collection, data interpretation and reviewing of the manuscript. M.G. carried out study design, statistical analysis plan design, data collection, data interpretation and writing of the report. L.Y. was responsible for data analysis, data interpretation and writing of the manuscript. B.T.-M. performed data analysis, data interpretation and writing of the manuscript. J.K. carried out data analysis, data interpretation and writing of the report. K.H. oversaw data analysis, data interpretation and writing of the report. K.K. undertook data analysis, data interpretation and writing of the manuscript. M.J.W. performed data collection, data analysis, data interpretation and writing of the report. D.L.G. carried out study design, data analysis, data interpretation and writing of the manuscript. L.G. performed clinical operations and reviewing the manuscript. J.O. was responsible for data analysis, data interpretation and writing of the manuscript. S.B.H. undertook data analysis, interpretation and writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
A.L.B. reports consultancies for AGTC, Alector, Arkuda, Arvinas, Asceneuron, AZTherapies, Bioage, GSK, Humana, Lundbeck, Ono, Roche, Samumed, Sangamo, Stealth Therapeutics, Third Rock, Transposon, UCB and Wave, and research support from the Association for Frontotemporal Degeneration, Biogen, Bluefield Project to Cure Frontotemporal Dementia, Eli Lilly, Eisai, National Institutes of Health (grant nos. U19AG063911, U54NS092089 and R01AG031278) and Tau Research Consortium. L.I.G. reports consultancies for AbbVie, AlzProtect, Asceneuron, Biogen, CurePSP, Martin, Mitochon, Mitsubishi Tanabe, Pinteon, Retrotope, Roche, Stealth BioTherapeutics and UCB, and research support from AbbVie, American Parkinson’s Disease Association and Biogen. G.U.H. reports consultancies for AbbVie, AlzProtect, Asceneuron, Biogen, Biohaven, Lundbeck, Novartis, Roche, Sanofi and UCB; honoraria for scientific presentations from AbbVie, Bayer Vital, Bial, Biogen, Bristol-Myers Squibb, Roche, Teva, UCB and Zambon; research collaborations with Orion, Prothena and Roche; research support from GE Health, Neuropore, German Research Foundation (DFG; EXC 2145 SyNergy, nos. 390857198, HO2402/6-2 and HO2402/18-1), the German Federal Ministry of Education and Research (BMBF, nos. 01KU1403A and 01EK1605A), the NOMIS foundation (FTLD project), the EU/EFPIA/Innovative Medicines Initiative (2) Joint Undertaking (IMPRIND, grant no. 116060) and VolkswagenStiftung/Lower Saxony Ministry for Science/Petermax-Müller Foundation (Niedersächsisches Vorab). H.R.M. reports consultancies for AbbVie, Biogen, Biohaven, Denali and UCB; employment by North Thames National Institute for Health Research and University College London; lecture fees/honoraria from Biogen, C4X Discovery, Movement Disorders Society, UCB and Wellcome Trust; research grants from CBD Solutions, Cure Parkinson’s Trust, Drake Foundation, Medical Research Council, MND Association, Parkinson’s UK and PSP Association; and being a coapplicant on a patent application related to C9ORF72 (method for diagnosing a neurodegenerative disease (no. PCT/GB2012/052140)). I.L. reports scientific advisory board membership for Corticobasal Degeneration Solutions and Lundbeck; research support from AbbVie, Biogen, Biohaven, EIP-Pharma, Roche, Lewy Body Association, Michael J. Fox Foundation, National Institutes of Health (grant nos. 5P50AG005131-33, 2R01AG038791-06A, U01NS090259, U01NS100610, U01NS80818, R25NS098999, P20GM109025, U19AG063911-1 and 1R21NS114764-01A1) and Parkinson Foundation and Parkinson Study Group; and employment at University of California San Diego and Chief Editor of Frontiers in Neurology. A.E.L. reports advisory board membership for AbbVie, AFFiRis, Biogen, Corticobasal Degeneration Solutions, Janssen, Jazz Pharma, Lilly, Lundbeck, Merck, Paladin, PhotoPharmics, Roche, Sunovion, Sun Pharma and Theravance; honoraria from AbbVie, Sunovion and Sun Pharma; grants from Brain Canada, Canadian Institutes of Health Research, Corticobasal Degeneration Solutions, Edmond J. Safra Philanthropic Foundation, Michael J. Fox Foundation, Ontario Brain Institute, the Parkinson Foundation and Parkinson Society Canada. J.-C.C. reports advisory board membership for Pfizer; consultancies for Air Liquide, AlzProtect, Biogen, Bristol-Myers Squibb, Denali and Theranexus; speaker fees from Biogen and Ever Pharma; research grants from Actelion and Michael J. Fox Foundation; and travel grants from MDS. I.A. reports consultancies for AbbVie and Biogen. M.G. reports consultancies for Biogen and Bristol-Myers Squibb. T.D., L.Y., B.T.-M., K.K., M.J.W., D.L.G., L.G., J.O. and S.B.H. are employees of, and hold stock in, Biogen. J.K. is a former employee of, and holds stock in, Biogen. K.H. reports being an independent physician pharmacovigilance professional at Biogen for the PASSPORT study.
Additional information
Peer review information Nature Medicine thanks Chengjie Xiong and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Jerome Staal was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
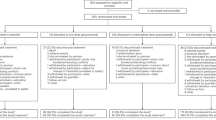
Extended Data Fig. 1 Participant Disposition in the PASSPORT study.
Percentages are based on the number of participants who received study drug. *Three participants randomly assigned to placebo received one dose of gosuranemab. †One participant assigned to placebo was not dosed due to abnormal vital signs, and three participants assigned to gosuranemab were not dosed because they failed to meet randomization criteria.
Supplementary information
Supplementary Information
Supplementary Tables 1 and 2 and Fig. 1.
Source data
Source Data Fig. 1
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dam, T., Boxer, A.L., Golbe, L.I. et al. Safety and efficacy of anti-tau monoclonal antibody gosuranemab in progressive supranuclear palsy: a phase 2, randomized, placebo-controlled trial. Nat Med 27, 1451–1457 (2021). https://doi.org/10.1038/s41591-021-01455-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-021-01455-x
This article is cited by
-
The therapeutic landscape of tauopathies: challenges and prospects
Alzheimer's Research & Therapy (2023)
-
TANGO: a placebo-controlled randomized phase 2 study of efficacy and safety of the anti-tau monoclonal antibody gosuranemab in early Alzheimer’s disease
Nature Aging (2023)
-
Tau-targeting therapies for Alzheimer disease: current status and future directions
Nature Reviews Neurology (2023)
-
Analysis of clinical failure of anti-tau and anti-synuclein antibodies in neurodegeneration using a quantitative systems pharmacology model
Scientific Reports (2023)
-
New Approaches to the Treatment of Frontotemporal Dementia
Neurotherapeutics (2023)