Abstract
Antidepressants are widely prescribed, but their efficacy relative to placebo is modest, in part because the clinical diagnosis of major depression encompasses biologically heterogeneous conditions. Here, we sought to identify a neurobiological signature of response to antidepressant treatment as compared to placebo. We designed a latent-space machine-learning algorithm tailored for resting-state electroencephalography (EEG) and applied it to data from the largest imaging-coupled, placebo-controlled antidepressant study (n = 309). Symptom improvement was robustly predicted in a manner both specific for the antidepressant sertraline (versus placebo) and generalizable across different study sites and EEG equipment. This sertraline-predictive EEG signature generalized to two depression samples, wherein it reflected general antidepressant medication responsivity and related differentially to a repetitive transcranial magnetic stimulation treatment outcome. Furthermore, we found that the sertraline resting-state EEG signature indexed prefrontal neural responsivity, as measured by concurrent transcranial magnetic stimulation and EEG. Our findings advance the neurobiological understanding of antidepressant treatment through an EEG-tailored computational model and provide a clinical avenue for personalized treatment of depression.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The EMBARC data are publicly available through the National Institute of Mental Health (NIMH) Data Archive (https://nda.nih.gov/edit_collection.html?id=2199).
Code availability
Code for SELSER is available for noncommercial use only at altoneuroscience.com. For commercial use, please contact Alto Neuroscience at info@altoneuroscience.com.
References
Drysdale, A. T. et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat. Med. 23, 28–38 (2017).
Cipriani, A. et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet 391, 1357–1366 (2018).
Fournier, J. C. et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA 303, 47–53 (2010).
Khan, A. & Brown, W. A. Antidepressants versus placebo in major depression: an overview. World Psychiatry 14, 294–300 (2015).
Kirsch, I. The Emperor’s New Drugs: Exploding the Antidepressant Myth (Random House, 2009).
Kirsch, I. et al. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the food and drug administration. PLoS Med. 5, e45 (2008).
Wade, E. C. & Iosifescu, D. V. Using electroencephalography for treatment guidance in major depressive disorder. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 1, 411–422 (2016).
Widge, A. S. et al. Electroencephalographic biomarkers for treatment response prediction in major depressive Illness: a meta-analysis. Am. J. Psychiatry 2018, 17121358 (2018).
Olbrich, S. & Arns, M. EEG biomarkers in major depressive disorder: discriminative power and prediction of treatment response. Int. Rev. Psychiatry 25, 604–618 (2013).
Jaworska, N., de la Salle, S., Ibrahim, M.-H., Blier, P. & Knott, V. Leveraging machine-learning approaches for predicting antidepressant treatment response using electroencephalography (EEG) and clinical data. Front. Psychiatry 9, 768 (2019).
Pizzagalli, D. A. et al. Pretreatment rostral anterior cingulate cortex theta activity in relation to symptom improvement in depression: a randomized clinical trial. JAMA Psychiatry 75, 547–554 (2018).
Korb, A. S., Hunter, A. M., Cook, I. A. & Leuchter, A. F. Rostral anterior cingulate cortex theta current density and response to antidepressants and placebo in major depression. Clin. Neurophysiol. 120, 1313–1319 (2009).
Leuchter, A. F., Cook, I. A., Witte, E. A., Morgan, M. & Abrams, M. Changes in brain function of depressed subjects during treatment with placebo. Am. J. Psychiatry 159, 122–129 (2002).
Nunez, P.L. & Srinivasan, R. Electric Fields of the Brain: The Neurophysics of EEG (Oxford Univ. Press, 2006).
Müller, K.-R. et al. Machine learning for real-time single-trial EEG-analysis: from brain–computer interfacing to mental state monitoring. J. Neurosci. Methods 167, 82–90 (2008).
Wu, W., Nagarajan, S. & Chen, Z. Bayesian machine learning: EEG/MEG signal processing measurements. IEEE Signal Process. Mag. 33, 14–36 (2016).
Schirrmeister, R. T. et al. Deep learning with convolutional neural networks for EEG decoding and visualization. Hum. Brain Mapp. 38, 5391–5420 (2017).
Haufe, S. et al. On the interpretation of weight vectors of linear models in multivariate neuroimaging. Neuroimage 87, 96–110 (2014).
Boyd, S. & Vandenberghe, L. Convex Optimization (Cambridge Univ. Press, 2004).
Bell, A. J. & Sejnowski, T. J. An information-maximization approach to blind separation and blind deconvolution. Neural Comput. 7, 1129–1159 (1995).
Trivedi, M. H. et al. Establishing moderators and biosignatures of antidepressant response in clinical care (EMBARC): rationale and design. J. Psychiatr. Res. 78, 11–23 (2016).
Fonzo, G. A. et al. Brain regulation of emotional conflict differentiates response to antidepressants versus placebo in depression. Nat. Hum. Behav. 3, 1319–1331 (2019).
Bruder, G. E. et al. Electroencephalographic α measures predict therapeutic response to a selective serotonin reuptake inhibitor antidepressant: pre-and post-treatment findings. Biol. Psychiatry 63, 1171–1177 (2008).
Tipping, M. E. Sparse Bayesian learning and the relevance vector machine. J. Mach. Learn. Res. 1, 211–244 (2001).
Grin-Yatsenko, V. A., Baas, I., Ponomarev, V. A. & Kropotov, J. D. Independent component approach to the analysis of EEG recordings at early stages of depressive disorders. Clin. Neurophysiol. 121, 281–289 (2010).
Pozzi, D., Golimstock, A., Petracchi, M., García, H. & Starkstein, S. Quantified electroencephalographic changes in depressed patients with and without dementia. Biol. Psychiatry 38, 677–683 (1995).
Iosifescu, D. V. et al. Frontal EEG predictors of treatment outcome in major depressive disorders. Eur. Neuropsychopharmacol. 19, 772–777 (2009).
Arns, M., Drinkenburg, W. H., Fitzgerald, P. B. & Kenemans, J. L. Neurophysiological predictors of non-response to rTMS in depression. Brain Stimul. 5, 569–576 (2012).
Tipping, M. E. & Bishop, C. M. Probabilistic principal component analysis. J. R. Stat. Soc. B 61, 611–622 (1999).
Trivedi, M. H. et al. Comprehensive phenotyping of depression disease trajectory and risk: rationale and design of Texas Resilience Against Depression study (T-RAD). J. Psychiatric Res. 122, 22–32 (2020).
Hill, A. T., Rogasch, N. C., Fitzgerald, P. B. & Hoy, K. E. TMS-EEG: a window into the neurophysiological effects of transcranial electrical stimulation in non-motor brain regions. Neurosci. Biobehav. Rev. 64, 175–184 (2016).
Chen, A. C. et al. Causal interactions between fronto-parietal central executive and default-mode networks in humans. Proc. Natl Acad. Sci. USA 110, 19944–19949 (2013).
Donse, L., Padberg, F., Sack, A. T., Rush, A. J. & Arns, M. Simultaneous rTMS and psychotherapy in major depressive disorder: clinical outcomes and predictors from a large naturalistic study. Brain Stimul. 11, 337–345 (2018).
Krepel, N. et al. Non-replication of neurophysiological predictors of non-response to rTMS in depression and neurophysiological data-sharing proposal. Brain Stimul. 11, 639–641 (2018).
Leuchter, A. F. et al. Comparative effectiveness of biomarkers and clinical indicators for predicting outcomes of SSRI treatment in major depressive disorder: results of the BRITE-MD study. Psychiatry Res. 169, 124–131 (2009).
Klimesch, W., Sauseng, P. & Hanslmayr, S. EEG α oscillations: the inhibition–timing hypothesis. Brain Res. Rev. 53, 63–88 (2007).
Jensen, O. & Mazaheri, A. Shaping functional architecture by oscillatory α activity: gating by inhibition. Front. Hum. Neurosci. 4, 186 (2010).
Arns, M. et al. EEG α asymmetry as a gender-specific predictor of outcome to acute treatment with different antidepressant medications in the randomized iSPOT-D study. Clin. Neurophysiol. 127, 509–519 (2016).
Lehtonen, J. & Lehtinen, I. α rhythm and uniform visual field in man. Electroencephalogr. Clin. Neurophysiol. 32, 139–147 (1972).
Hari, R. & Salmelin, R. Human cortical oscillations: a neuromagnetic view through the skull. Trends Neurosci. 20, 44–49 (1997).
Ramoser, H., Müller-Gerking, J. & Pfurtscheller, G. Optimal spatial filtering of single trial EEG during imagined hand movement. IEEE Trans. Rehabil. Eng. 8, 441–446 (2000).
Kraemer, H. C. Messages for clinicians: moderators and mediators of treatment outcome in randomized clinical trials. Am. J. Psychiatry 173, 672–679 (2016).
Nguyen, K. H. & Gordon, L. G. Cost-effectiveness of repetitive transcranial magnetic stimulation versus antidepressant therapy for treatment-resistant depression. Value Health 18, 597–604 (2015).
Voigt, J., Carpenter, L. & Leuchter, A. Cost effectiveness analysis comparing repetitive transcranial magnetic stimulation to antidepressant medications after a first treatment failure for major depressive disorder in newly diagnosed patients: a lifetime analysis. PLoS ONE 12, e0186950 (2017).
O’Reardon, J. P. et al. Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multisite randomized controlled trial. Biol. Psychiatry 62, 1208–1216 (2007).
George, M. S. et al. Daily left prefrontal transcranial magnetic stimulation therapy for major depressive disorder: a sham-controlled randomized trial. Arch. Gen. Psychiatry 67, 507–516 (2010).
Williams, L. M., Debattista, C., Duchemin, A., Schatzberg, A. & Nemeroff, C. Childhood trauma predicts antidepressant response in adults with major depression: data from the randomized international study to predict optimized treatment for depression. Transl. Psychiatry 6, e799 (2016).
Liston, C. et al. Default mode network mechanisms of transcranial magnetic stimulation in depression. Biol. Psychiatry 76, 517–526 (2014).
Sani, O. G. et al. Mood variations decoded from multi-site intracranial human brain activity. Nat. Biotechnol. 36, 954–961 (2018).
van Buuren, S. & Groothuis-Oudshoorn, K. Mice: multivariate imputation by chained equations in R. J. Stat. Softw. 45, 1–67 (2011).
Etkin, A., Egner, T., Peraza, D. M., Kandel, E. R. & Hirsch, J. Resolving emotional conflict: a role for the rostral anterior cingulate cortex in modulating activity in the amygdala. Neuron 51, 871–882 (2006).
Etkin, A., Buchel, C. & Gross, J. J. The neural bases of emotion regulation. Nat. Rev. Neurosci. 16, 693–700 (2015).
Egner, T. & Hirsch, J. Cognitive control mechanisms resolve conflict through cortical amplification of task-relevant information. Nat. Neurosci. 8, 1784–1790 (2005).
Jenkinson, M., Beckmann, C. F., Behrens, T. E., Woolrich, M. W. & Smith, S. M. FSL. Neuroimage 62, 782–790 (2012).
Friston, K. J. et al. Statistical parametric maps in functional imaging: a general linear approach. Hum. Brain Mapp. 2, 189–210 (1995).
Wu, W. et al. ARTIST: a fully automated artifact rejection algorithm for single‐pulse TMS‐EEG data. Hum. Brain Mapp. 39, 1607–1625 (2018).
Lovibond, P. F. & Lovibond, S. H. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety inventories. Behav. Res. Ther. 33, 335–343 (1995).
Tomioka, R. & Müller, K.-R. A regularized discriminative framework for EEG analysis with application to brain–computer interface. Neuroimage 49, 415–432 (2010).
Srebro, N. & Jaakkola, T. Weighted low-rank approximations. in Proc. 20th International Conference on Machine Learning (ICML-03) 720–727 (AAAI Press, 2003).
Candès, E. J., Li, X., Ma, Y. & Wright, J. Robust principal-component analysis? J. ACM 58, 11 (2011).
Parikh, N. & Boyd, S. Proximal algorithms. Found. Trends Mach. Learn. 1, 127–239 (2014).
Gramfort, A., Papadopoulo, T., Olivi, E. & Clerc, M. OpenMEEG: opensource software for quasistatic bioelectromagnetics. Biomed. Eng. Online 9, 45 (2010).
Fischl, B. FreeSurfer. Neuroimage 62, 774–781 (2012).
Pascual-Marqui, R. D. Standardized low-resolution brain electromagnetic tomography (sLORETA): technical details. Method. Find. Exp. Clin. Pharmacol. 24, 5–12 (2002).
Hunter, A. M., Leuchter, A. F., Morgan, M. L. & Cook, I. A. Changes in brain function (quantitative EEG cordance) during placebo lead-in and treatment outcomes in clinical trials for major depression. Am. J. Psychiatry 163, 1426–1432 (2006).
Makeig, S., Bell, A. J., Jung, T.-P. & Sejnowski, T. J. Independent component analysis of electroencephalographic data. in Advances in Neural Information Processing Systems Vol. 8 (eds Touretzky, D. et al.) (MIT Press, 1996).
Ghosh-Dastidar, S., Adeli, H. & Dadmehr, N. Principal component analysis-enhanced cosine radial basis function neural network for robust epilepsy and seizure detection. IEEE Trans. Biomed. Eng. 55, 512–518 (2008).
Cichocki, A. & Amari, S. Adaptive Blind Signal and Image Processing: Learning Algorithms and Applications, Vol. 1 (John Wiley & Sons, 2002).
Witten, I.H., Frank, E., Hall, M.A. & Pal, C.J. Data Mining: Practical Machine Learning Tools and Techniques (Morgan Kaufmann, 2016).
Schaefer, A. et al. Local-global parcellation of the human cerebral cortex from intrinsic functional connectivity MRI. Cereb. Cortex 28, 3095–3114 (2018).
Acknowledgements
We thank C.J. Keller and S. Kim. The EMBARC study was supported by the National Institute of Mental Health of the National Institutes of Health (NIH) under award nos, U01MH092221 (M.H.T.) and U01MH092250 (P.J.M., R.V.P. and M.M.W.). Data from the second depressed cohort were acquired under R01MH103324 (A.E.) and Big Idea in Neuroscience research funds from the Stanford Neurosciences Institute (A.E.). This work was also funded in part by the Hersh Foundation (M.H.T.). A.E. and W.W. were additionally funded by NIH grant no. DP1 MH116506. W.W. was also funded by National Key Research and Development Plan of China (grant no. 2017YFB1002505) and the National Natural Science Foundation of China (grant nos. 61876063 and 61836003).
Author information
Authors and Affiliations
Contributions
W.W. contributed to the analysis and interpretation of the data and the drafting and revision of the manuscript. Y.Z. and J.J. contributed to the analysis and interpretation of the data and drafting of the manuscript. M.V.L. and G.A.F. contributed to the drafting and revision of the manuscript. C.E.R, C.C., C.C.F., N.K., C.A.C., R.W., R.T., H.M.T., K.M., T.L.C., K.S., M.K.J. and J.M.T. contributed to the conduct of the study, analysis and interpretation of the data, and revision of the manuscript. T.D., P.A., P.J.M., M.M.W. and M.F. contributed to the design and conduct of the study. D.A.P., M.A. and M.H.T. contributed to the design and conduct of the study, and the drafting and revision of the manuscript. A.E. contributed to the design and conduct of the study, the analysis and interpretation of the data and the drafting and revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
A.E. (lifetime disclosure) has been receiving salary and equity from Alto Neuroscience since 1 November 2019, to which the pending patent for SELSER has been licensed from Stanford. He holds equity in Mindstrong Health, Akili Interactive and Sizung for unrelated work, has received research funding from the National Institute of Mental Health, Department of Veterans Affairs, Cohen Veterans Bioscience, Brain and Behavior Research Foundation, Dana Foundation, Brain Resource Inc. and the Stanford Neurosciences Institute and consulted for Cervel, Takaeda, Posit Science, Acadia, Otsuka, Lundbeck and Janssen. Over the past 3 years, D.A.P. has received consulting fees from Alkermes, BlackThorn Therapeutics, Boehreinger Ingelheim, Posit Science and Takeda Pharmaceuticals. He has received funding from NIMH, the Dana Foundation and Brain and Behavior Research Foundation. T.D.’s research has been funded by NIH, NIMH, National Alliance for Research on Schizophrenia & Depression, TSA, IOCDF, Tufts University, DBDAT and Otsuka Pharmaceuticals. He has received honoraria, consultation fees and/or royalties from the MGH Psychiatry Academy, BrainCells Inc., Clintara, LLC, Inc., Systems Research and Applications Corporation, Boston University, the Catalan Agency for Health Technology Assessment and Research, the National Association of Social Workers Massachusetts, the Massachusetts Medical Society, Tufts University, National Institute of Drug Abuse, NIMH, Oxford University Press, Guilford Press and Rutledge. He has also participated in research funded by DARPA, NIH, NIA, Agency for Healthcare Research and Quality, PCORI, Janssen Pharmaceuticals, The Forest Research Institute, Shire Development Inc., Medtronic, Cyberonics, Northstar and Takeda. P.M. has received funding from the National Institute of Mental Health, New York State Department of Mental Hygiene, Research Foundation for Mental Hygiene (New York State), Forest Research Laboratories, Sunovion Pharmaceuticals and Naurex Pharmaceuticals (now Allergan). In the past 2 years, M.W. received funding from the NIMH, the National Institute on Drug Abuse, the National Alliance for Research on Schizophrenia and Depression, the Sackler Foundation, the Templeton Foundation; and receives royalties from the Oxford University Press, Perseus Press, the American Psychiatric Association Press and MultiHealth Systems. M.F. has received research support from Abbot Laboratories; Alkermes, Inc.; American Cyanamid; Aspect Medical Systems; AstraZeneca; Avanir Pharmaceuticals; BioResearch; BrainCells Inc.; Bristol-Myers Squibb; CeNeRx BioPharma; Cephalon; Clintara, LLC; Cerecor; Covance; Covidien; Eli Lilly and Company; EnVivo Pharmaceuticals, Inc.; Euthymics Bioscience, Inc.; Forest Pharmaceuticals, Inc.; Ganeden Biotech, Inc.; GlaxoSmithKline; Harvard Clinical Research Institute; Hoffman-LaRoche; Icon Clinical Research; i3 Innovus/Ingenix; Janssen R&D, LLC; Jed Foundation; Johnson & Johnson Pharmaceutical Research & Development; Lichtwer Pharma GmbH; Lorex Pharmaceuticals; Lundbeck Inc.; MedAvante; Methylation Sciences Inc.; National Alliance for Research on Schizophrenia & Depression; National Center for Complementary and Alternative Medicine; National Institute of Drug Abuse; NIMH; Neuralstem, Inc.; Novartis AG; Organon Pharmaceuticals; PamLab, LLC.; Pfizer Inc.; Pharmacia-Upjohn; Pharmaceutical Research Associates., Inc.; Pharmavite LLC; PharmoRx Therapeutics; Photothera; Reckitt Benckiser; Roche Pharmaceuticals; RCT Logic, LLC (formerly Clinical Trials Solutions, LLC); Sanofi-Aventis US LLC; Shire; Solvay Pharmaceuticals, Inc.; Stanley Medical Research Institute; Synthelabo; Tal Medical; and Wyeth-Ayerst Laboratories. He has served as advisor or consultant to Abbott Laboratories; Acadia; Affectis Pharmaceuticals AG; Alkermes, Inc.; Amarin Pharma Inc.; Aspect Medical Systems; AstraZeneca; Auspex Pharmaceuticals; Avanir Pharmaceuticals; AXSOME Therapeutics; Bayer AG; Best Practice Project Management, Inc.; Biogen; BioMarin Pharmaceuticals, Inc.; Biovail Corporation; BrainCells Inc; Bristol-Myers Squibb; CeNeRx BioPharma; Cephalon, Inc.; Cerecor; CNS Response, Inc.; Compellis Pharmaceuticals; Cypress Pharmaceutical, Inc.; DiagnoSearch Life Sciences (P) Ltd.; Dinippon Sumitomo Pharma Co. Inc.; Dov Pharmaceuticals, Inc.; Edgemont Pharmaceuticals, Inc.; Eisai Inc.; Eli Lilly and Company; EnVivo Pharmaceuticals, Inc.; ePharmaSolutions; EPIX Pharmaceuticals, Inc.; Euthymics Bioscience, Inc.; Fabre-Kramer Pharmaceuticals, Inc.; Forest Pharmaceuticals, Inc.; Forum Pharmaceuticals; GenOmind, LLC; GlaxoSmithKline; Grunenthal GmbH; i3 Innovus/Ingenis; Intracellular; Janssen Pharmaceutica; Jazz Pharmaceuticals, Inc.; Johnson & Johnson Pharmaceutical Research & Development, LLC; Knoll Pharmaceuticals Corp.; Labopharm Inc.; Lorex Pharmaceuticals; Lundbeck Inc.; MedAvante, Inc.; Merck & Co., Inc.; MSI Methylation Sciences, Inc.; Naurex, Inc.; Nestle Health Sciences; Neuralstem, Inc.; Neuronetics, Inc.; NextWave Pharmaceuticals; Novartis AG; Nutrition 21; Orexigen Therapeutics, Inc.; Organon Pharmaceuticals; Osmotica; Otsuka Pharmaceuticals; Pamlab, LLC.; Pfizer Inc.; PharmaStar; Pharmavite LLC.; PharmoRx Therapeutics; Precision Human Biolaboratory; Prexa Pharmaceuticals, Inc.; Puretech Ventures; PsychoGenics; Psylin Neurosciences, Inc.; RCT Logic, LLC Formerly Clinical Trials Solutions, LLC; Rexahn Pharmaceuticals, Inc.; Ridge Diagnostics, Inc.; Roche; Sanofi-Aventis US LLC.; Sepracor Inc.; Servier Laboratories; Schering-Plough Corporation; Solvay Pharmaceuticals, Inc.; Somaxon Pharmaceuticals, Inc.; Somerset Pharmaceuticals, Inc.; Sunovion Pharmaceuticals; Supernus Pharmaceuticals, Inc.; Synthelabo; Taisho Pharmaceutical; Takeda Pharmaceutical Company Limited; Tal Medical, Inc.; Tetragenex Pharmaceuticals, Inc.; TransForm Pharmaceuticals, Inc.; Transcept Pharmaceuticals, Inc.; Vanda Pharmaceuticals, Inc.; and VistaGen. He has received speaking or publishing fees from Adamed, Co; Advanced Meeting Partners; American Psychiatric Association; American Society of Clinical Psychopharmacology; AstraZeneca; Belvoir Media Group; Boehringer Ingelheim GmbH; Bristol-Myers Squibb; Cephalon, Inc.; CME Institute/Physicians Postgraduate Press, Inc.; Eli Lilly and Company; Forest Pharmaceuticals, Inc.; GlaxoSmithKline; Imedex, LLC; MGH Psychiatry Academy/Primedia; MGH Psychiatry Academy/Reed Elsevier; Novartis AG; Organon Pharmaceuticals; Pfizer Inc.; PharmaStar; United BioSource, Corp.; and Wyeth-Ayerst Laboratories. He has equity holdings in Compellis and PsyBrain, Inc.; he has a patent for Sequential Parallel Comparison Design, which is licensed by MGH to Pharmaceutical Product Development, LLC (PPD); and a patent application for a combination of Ketamine plus Scopolamine in Major Depressive Disorder, licensed by MGH to Biohaven; and he receives copyright royalties for the MGH Cognitive & Physical Functioning Questionnaire, Sexual Functioning Inventory, ATRQ, Discontinuation-Emergent Signs & Symptoms, Symptoms of Depression Questionnaire, and SAFER; Lippincott, Williams & Wilkins; Wolkers Kluwer; and World Scientific Publishing Co. Pte. Ltd. M.H.T. is or has been an advisor/consultant and received fees from (lifetime disclosure): Abbott Laboratories, Inc., Abdi Ibrahim, Akzo (Organon Pharmaceuticals Inc.), Alkermes, AstraZeneca, Axon Advisors, Bristol-Myers Squibb Company, Cephalon, Inc., Cerecor, CME Institute of Physicians, Concert Pharmaceuticals, Inc., Eli Lilly & Company, Evotec, Fabre-Kramer Pharmaceuticals, Inc., Forest Pharmaceuticals, GlaxoSmithKline, Janssen Global Services, LLC, Janssen Pharmaceutica Products, LP, Johnson & Johnson PRD, Libby, Lundbeck, Meade Johnson, MedAvante, Medtronic, Merck, Mitsubishi Tanabe Pharma Development America, Inc., Naurex, Neuronetics, Otsuka Pharmaceuticals, Pamlab, Parke-Davis Pharmaceuticals, Inc., Pfizer Inc., PgxHealth, Phoenix Marketing Solutions, Rexahn Pharmaceuticals, Ridge Diagnostics, Roche Products Ltd., Sepracor, SHIRE Development, Sierra, SK Life and Science, Sunovion, Takeda, Tal Medical/Puretech Venture, Targacept, Transcept, VantagePoint, Vivus and Wyeth-Ayerst Laboratories. In addition, he has received grants/research support from: Agency for Healthcare Research and Quality, Cyberonics, Inc., National Alliance for Research in Schizophrenia and Depression, National Institute of Mental Health and the National Institute on Drug Abuse. J.M.T. currently owns stock in Merck and Gilead Sciences and within the past 36 months has previously owned stock in Johnson & Johnson. M.A. holds options from Brain Resource, is Director and Owner of Research Institute Brainclinics, has equity in neuroCare Group and is co-inventor on four patent applications (A61B5/0402; US2007/0299323, A1; WO2010/139361 A1) related to EEG, neuromodulation and psychophysiology, but does not own these nor receives any proceeds related to these patents; he receives Research Institute Brainclinics funding from Brain Resource and neuroCare Group and equipment support from Deymed, neuroConn and Magventure. All other authors report no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Integrated supplementary information
Supplementary Figure 1 EMBARC CONSORT Flow Diagram for the patients included in the treatment prediction analyses.
For this analysis, patients were included (1) regardless of their HAMD17 score, and (2) if they had resting-state EEG data of sufficient quality.
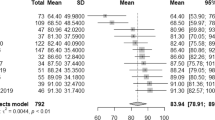
Supplementary Figure 2 Illustration of SERLSER training and evaluation using 10-fold stratified cross-validation.
Study sites were Columbia University (CU), University of Texas Southwestern Medical Center (TX), University of Michigan (UM) and Massachusetts General Hospital (MG). Data were randomly partitioned into 10 subsets, such that each subset containing an approximately equal number of subjects from each of the four study sites. A subset was left out as the test data, and the remaining 9 subsets were used as the training data. The process was then repeated 10 times, where each of the 10 subsets was used exactly once as the test data. As a result, each subject had a predicted HAMD17 score change. The prediction performance was then quantified by the Pearson’s correlation coefficient and root mean square error (r.m.s.e.) between the cross-validated prediction of the HAMD17 score change and the true HAMD17 score change.
Supplementary Figure 3 Singular values associated with alpha SELSER latent signals for the sertraline arm of EMBARC.
From left to right, the latent signals are sorted according to decreasing singular values (note that the singular values are the absolute values of the eigenvalues for a symmetric matrix). The alpha rsEEG data from all the participants in the sertraline arm were used to train the SELSER model.
Supplementary Figure 4 Prediction of outcome specific to sertraline (n = 109) using SELSER trained on resting eyes open alpha-frequency range data of different lengths.
Prediction performance was assessed with 10 × 10 stratified cross-validation prediction. (a) 1.5 minutes/block. Pearson’s r = 0.58, p = 3.1 × 10−11 based on the one-sided test against the alternative hypothesis that r > 0. (b) 1 minute/block. Pearson’s r = 0.44, p = 1.06 × 10−6 based on the one-sided test against the alternative hypothesis that r > 0. (c) 30 seconds/block. Pearson’s r = 0.34, p = 1.42 × 10−4 based on the one-sided test against the alternative hypothesis that r > 0.
Supplementary Figure 5 Prediction of outcome specific to sertraline (n = 109) using SELSER trained on resting eyes open alpha-frequency range data of different blocks.
Prediction performance was assessed with 10 × 10 stratified cross-validation prediction. (a) Block 1. Pearson’s r = 0.47, p = 1.07 × 10−7 based on the one-sided test against the alternative hypothesis that r > 0. (b) Block 2. Pearson’s r = 0.35, p = 1.14 × 10−4 based on the one-sided test against the alternative hypothesis that r > 0. (c) Block 1 prediction vs. block 2 prediction. Pearson’s r = 0.58, p = 5.23 × 10−11 based on the one-sided test against the alternative hypothesis that r > 0.
Supplementary Figure 6 Scalp and cortical spatial patterns of the placebo (PBO) alpha SELSER latent signals (n = 119).
(a, c) Spatial patterns of the SELSER latent signals for the resting eyes open (REO) condition, with the most positive (β = 556.50.31; left) and negative (β = -773.49; right) regression weights, respectively. (b, d) Spatial patterns of the SELSER latent signals for the resting eyes closed (REC) condition, with the most positive (β = 840.85; left) and negative (β = -801.23; right) regression weights, respectively.
Supplementary Figure 7 Treatment stratification using the rsEEG predictive signature.
Patients in each arm were partitioned into the low and high groups by applying a median split on the cross-validated predicted HAMD17 score changes for sertraline response. n = 109 for the sertraline arm, and 119 for the placebo arm. Each dot represents one patient. For each box, the central line depicts the median, the box extends vertically between the 25th and 75th percentiles, and the whiskers extend to the most extreme date that are not considered outliers. Dashed line indicates 50% change in the true HAMD17 score. SER = sertraline, PBO = placebo.
Supplementary Figure 8 Influence of site correction on leave-study-site-out cross-validation performance (n = 109).
Study sites were Columbia University (CU), University of Texas Southwestern Medical Center (TX), University of Michigan (UM) and Massachusetts General Hospital (MG). Treatment prediction across study sites was assessed by a leave-study-site-out cross-validation on the alpha REO sertraline model. (a) Treatment prediction when site effect was not accounted for. Pearson’s r = 0.34, Bonferroni-corrected p = 2.6 × 10−3 based on the one-sided test against the alternative hypothesis that r > 0. (b) Comparison of root mean square error (r.m.s.e.) without and with site correction.
Supplementary Figure 9 Machine learning prediction of treatment outcome using previously-suggested predictive metrics (alpha power, theta power, and theta cordance) and conventional latent space modeling approaches (PCA and ICA) on eyes open rsEEG data of the sertraline arm (n = 109).
10 × 10 stratified cross-validation prediction using the relevance vector machine (RVM) on channel-level alpha power (a; Pearson’s r = -0.07, p = 0.75 based on the one-sided test against the alternative hypothesis that r > 0), theta power (b; Pearson’s r = -0.23, p = 0.99 based on the one-sided test against the alternative hypothesis that r > 0), theta cordance (c; Pearson’s r = -0.16, p = 0.95 based on the one-sided test against the alternative hypothesis that r > 0), alpha power of the PCA-extracted latent signals (d; Pearson’s r = 0.14, p = 0.1 based on the one-sided test against the alternative hypothesis that r > 0), or alpha power of the ICA-extracted latent signals (e; Pearson’s r = -0.04, p = 0.6 based on the one-sided test against the alternative hypothesis that r > 0) do not significantly predict outcome for sertraline.
Supplementary Figure 10 Comparison of different band-power based treatment prediction approaches.
(a) End-to-end prediction with SELSER. All the unknown parameters (spatial filters and linear regression weight coefficients) are optimized in conjunction under a unified objective function via convex optimization. (b) Prediction with ICA/PCA. Spatial filters are optimized via ICA/PCA, and linear regression weight coefficients are optimized via RVM with a linear kernel. (c) Prediction with channel-level band power. EEG band power of each channel is fed directly into the linear regression model, which is optimized via RVM with a linear kernel. S1, S2, and SN refer to Subject 1, Subject 2, and the Nth Subject, respectively. C1, C2, F1, F2 and Pz refer to electrode locations according to the 10/10 international system. (·)2 denotes the square operator, and ∫t denotes the average of a time series over time.
Supplementary Figure 11 Machine learning prediction of treatment outcome from symptoms.
Prediction performance was assessed with 10 × 10 cross-validation prediction using the relevance vector machine (RVM). Included symptom measures were the Spielberger State-Trait Anxiety Inventory, the Quick Inventory of Depressive Symptoms, the Mood and Anxiety Questionnaire, the Childhood Trauma Questionnaire, age, and education. (a) Sertraline arm (n = 109). Pearson’s r = 0.26, p = 3 × 10−3 based on the one-sided test against the alternative hypothesis that r > 0. (b) Placebo arm (n = 119). Pearson’s r = 0.16, p = 0.05 based on the one-sided test against the alternative hypothesis that r > 0.
Supplementary Figure 12 Prediction of outcome specific to sertraline using SELSER trained on resting eyes open alpha-frequency range data of posterior channels (n = 109).
A total of 16 posterior electrodes were included: P1, P2, P3, P4, P5, P6, P7, P8, PO3, PO4, PO7, PO8, POz, O1, O2, and Oz. Prediction performance was assessed with 10 × 10 stratified cross-validation prediction. Pearson’s r = 0.40, p = 8.22 × 10−6 based on the one-sided test against the alternative hypothesis that r > 0. The most positive regression weight is 759.31 and the most negative regression weight is −853.13.
Supplementary information
Supplementary Information
Supplementary Figs. 1–12 and Tables 1–3.
Rights and permissions
About this article
Cite this article
Wu, W., Zhang, Y., Jiang, J. et al. An electroencephalographic signature predicts antidepressant response in major depression. Nat Biotechnol 38, 439–447 (2020). https://doi.org/10.1038/s41587-019-0397-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41587-019-0397-3
This article is cited by
-
Neurosteroids: mechanistic considerations and clinical prospects
Neuropsychopharmacology (2024)
-
No time to lose: the current state of research in rapid-acting psychotherapeutics
Neuropsychopharmacology (2024)
-
Symptom dimensions of resting-state electroencephalographic functional connectivity in autism
Nature Mental Health (2024)
-
Disentanglement of Resting State Brain Networks for Localizing Epileptogenic Zone in Focal Epilepsy
Brain Topography (2024)
-
The evolution of Big Data in neuroscience and neurology
Journal of Big Data (2023)