Abstract
Globally, nearly half of deaths from cirrhosis and chronic liver diseases (CLD) and three-quarters of deaths from hepatocellular carcinoma (HCC) occur in the Asia-Pacific region. Chronic hepatitis B is responsible for the vast majority of liver-related deaths in the region. Metabolic dysfunction-associated steatotic liver disease (MASLD) is the most common form of CLD, affecting an estimated 30% of the adult population. Compared with people of European descent, people from the Asia-Pacific region carry more genetic variants associated with MASLD and its progression. Alcohol is a fast-growing cause of CLD and HCC in Asia as a result of the rising per-capita consumption of alcohol. Drug-induced liver injury is under-recognized and probably has a high prevalence in this region. The epidemiological and outcome data of acute-on-chronic liver failure are heterogeneous, and non-unified definitions across regions contribute to this heterogeneity. CLDs are severely underdiagnosed, and effective treatments and vaccinations are underutilized. In this Review, we highlight trends in the burden of CLD and HCC in the Asia-Pacific region and discuss the rapidly changing aetiologies of liver disease. We examine the multiple gaps in the care cascade and propose mitigating strategies and future directions.
Key points
-
Over 50% of global deaths related to chronic liver disease, cirrhosis, and liver cancer occur in the Asia-Pacific region.
-
The majority of people living with chronic hepatitis B (CHB) infection are undiagnosed or untreated, rendering CHB the key cause of liver-related deaths in the Asia-Pacific region.
-
Differences in genetic makeup, lifestyle and cultures contribute to unique phenotypes of metabolic dysfunction-associated steatotic liver disease in the Asia-Pacific region.
-
Many challenges in tackling chronic liver diseases in the Asia-Pacific region stem from resource limitations, leading to poor accessibility to investigations and treatments.
-
Regulation of alcohol use, enforcement of national strategies for viral hepatitis elimination, and the establishment of pharmacovigilance programmes and disease awareness campaigns might reduce the burden of chronic liver disease in Asia.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
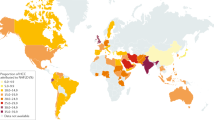
Data availability
Structural databases referred to in Figures and Table 1 can be accessed and downloaded from https://gbd2019.healthdata.org/gbd-results/ (Global Burden of Disease 2019 study), https://data.worldbank.org/indicator/NY.GDP.PCAP.CD and https://population.un.org/wpp/ (gross domestic product per capita). Where data of disease burden for certain countries or regions were not available, the Global Burden of Disease 2019 study results depended on modelling and past trends.
References
Department of Economic and Social Affairs. World Population Prospects 2024. United Nations https://population.un.org/wpp/ (2024).
Global Health Observatory. Global Health Estimates 2020: Life expectancy and leading causes of death and disability. World Health Organization https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death (2020).
Global Health Observatory. Age-standardized rate per 100000 by region. IARC https://gco.iarc.fr/today/en/dataviz (2022).
Rinella, M. E. et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J. Hepatol. 78, 1966–1986 (2023).
Eslam, M. et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J. Hepatol. 73, 202–209 (2020).
Méndez-Sánchez, N. et al. Global multi-stakeholder endorsement of the MAFLD definition. Lancet Gastroenterol. Hepatol. 7, 388–390 (2022).
Song, S. J., Lai, J. C., Wong, G. L., Wong, V. W. & Yip, T. C. Can we use old NAFLD data under the new MASLD definition? J. Hepatol. 80, e54–e56 (2024).
Arora, U., Biswas, S., Aggarwal, S. & Duseja, A. Shalimar. MASLD screening and diagnostic algorithms are interchangeable with existing NAFLD literature. J. Hepatol. 80, e89–e91 (2024).
Miao, L., Ye, S. M. & Zheng, M. H. “Fatty” or “steatotic”: position statement from a linguistic perspective by the Chinese-speaking community. J. Hepatol. https://doi.org/10.1016/j.jhep.2024.05.031 (2024).
Ramírez-Mejía, M. M., Jiménez-Gutiérrez, C., Eslam, M., George, J. & Méndez-Sánchez, N. Breaking new ground: MASLD vs. MAFLD – which holds the key for risk stratification? Hepatol. Int. 18, 168–178 (2024).
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017 Lancet 392 1789 1858 (2018).
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222 (2020).
World Health Organization. Roadmap for health and well-being in Central Asia (2022–2025) (WHO, 2022).
Institute for Health Metrics and Evaluation. Global Burden of Disease Study 2021 (GBD 2021): Results (IHME, 2022).
Lan, Y. et al. The burden of liver cirrhosis and underlying etiologies: results from the Global Burden of Disease Study 2019. Hepatol. Commun. 7, e0026 (2023).
Tan, D. et al. Global epidemiology of cirrhosis: changing etiological basis and comparable burden of nonalcoholic steatohepatitis between males and females. Dig. Dis. 41, 900–912 (2023).
Paik, J. et al. The global burden of liver cancer (LC) and chronic liver diseases (CLD) is driven by non-alcoholic steatohepatitis (NASH) and alcohol liver disease (ALD) [abstract GS008] J. Hepatol. 77, (Suppl. 1) 5–7 (2022).
Philips, C. A., Augustine, P., Rajesh, S., Y, P. K. & Madhu, D. Complementary and alternative medicine-related drug-induced liver injury in Asia. J. Clin. Transl. Hepatol. 7, 263–274 (2019).
Devarbhavi, H. et al. Drug-induced acute-on-chronic liver failure in Asian patients. Am. J. Gastroenterol. 114, 929–937 (2019).
Sherman, M. Hepatocellular carcinoma: epidemiology, risk factors, and screening. Semin. Liver Dis. 25, 143–154 (2005).
Hsu, Y. C., Huang, D. Q. & Nguyen, M. H. Global burden of hepatitis B virus: current status, missed opportunities and a call for action. Nat. Rev. Gastroenterol. Hepatol. 20, 524–537 (2023).
Polaris Observatory Collaborators Global prevalence, cascade of care, and prophylaxis coverage of hepatitis B in 2022: a modelling study Lancet Gastroenterol. Hepatol. 8, 879–907 (2023).
Hyams, K. C. Risks of chronicity following acute hepatitis B virus infection: a review. Clin. Infect. Dis. 20, 992–1000 (1995).
Syangbo, A. et al. Associations between the prevalence of chronic hepatitis B among people who inject drugs and country-level characteristics: an ecological analysis. Drug Alcohol Rev. 42, 569–581 (2023).
GBD Hepatitis B Collaborators. Global, regional, and national burden of hepatitis B, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol. Hepatol. 7, 796–829 (2022).
Schmit, N., Nayagam, S., Thursz, M. R. & Hallett, T. B. The global burden of chronic hepatitis B virus infection: comparison of country-level prevalence estimates from four research groups. Int. J. Epidemiol. 50, 560–569 (2021).
Simonetti, J. et al. Clearance of hepatitis B surface antigen and risk of hepatocellular carcinoma in a cohort chronically infected with hepatitis B virus. Hepatology 51, 1531–1537 (2010).
Polaris Observatory HCV Collaborators Global change in hepatitis C virus prevalence and cascade of care between 2015 and 2020: a modelling study Lancet Gastroenterol. Hepatol. 7 396 415 (2022).
Goel, A., Rewari, B. B., Sharma, M., Konath, N. M. & Aggarwal, R. Seroprevalence and burden of hepatitis C virus infection in WHO South-East Asia region: a systematic review. J. Gastroenterol. Hepatol. 37, 964–972 (2022).
Degenhardt, L. et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob. Health 5, e1192–e1207 (2017).
Magri, M. C. et al. Hepatitis C among people who inject drugs (PWID) in Latin America and the Caribbean: a meta-analysis of prevalence over three decades. J. Stud. Alcohol Drugs 84, 118–127 (2023).
Wiessing, L. et al. Hepatitis C virus infection epidemiology among people who inject drugs in Europe: a systematic review of data for scaling up treatment and prevention. PLoS ONE 9, e103345 (2014).
Aghaei, A. M. et al. Prevalence of injecting drug use and HIV, hepatitis B, and hepatitis C in people who inject drugs in the Eastern Mediterranean region: a systematic review and meta-analysis. Lancet Glob. Health 11, e1225–e1237 (2023).
Jaacks, L. M. et al. The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol. 7, 231–240 (2019).
Younossi, Z. M. et al. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology 77, 1335–1347 (2023).
Li, J. et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999-2019: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 4, 389–398 (2019).
Riazi, K. et al. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 7, 851–861 (2022).
Le, M. H. et al. 2019 global NAFLD prevalence: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 20, 2809–2817.e28 (2022).
Wu, Y. et al. The epidemiology of NAFLD in mainland China with analysis by adjusted gross regional domestic product: a meta-analysis. Hepatol. Int. 14, 259–269 (2020).
Younossi, Z. M. et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: a systematic review and meta-analysis. J. Hepatol. 71, 793–801 (2019).
Quek, J. et al. Global prevalence of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in the overweight and obese population: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 8, 20–30 (2023).
Zhou, F. et al. Unexpected rapid increase in the burden of NAFLD in China from 2008 to 2018: a systematic review and meta-analysis. Hepatology 70, 1119–1133 (2019).
Chan, W. K. et al. Clinical features and treatment of nonalcoholic fatty liver disease across the Asia Pacific region – the GO ASIA initiative. Aliment. Pharmacol. Ther. 47, 816–825 (2018).
Wei, J. L. et al. Prevalence and severity of nonalcoholic fatty liver disease in non-obese patients: a population study using proton-magnetic resonance spectroscopy. Am. J. Gastroenterol. 110, 1306–1314 (2015).
Young, S. et al. Prevalence and profile of nonalcoholic fatty liver disease in lean adults: systematic review and meta-analysis. Hepatol. Commun. 4, 953–972 (2020).
Fracanzani, A. L. et al. Liver and cardiovascular damage in patients with lean nonalcoholic fatty liver disease, and association with visceral obesity. Clin. Gastroenterol. Hepatol. 15, 1604–1611,e1 (2017).
Sookoian, S. & Pirola, C. J. Systematic review with meta-analysis: the significance of histological disease severity in lean patients with nonalcoholic fatty liver disease. Aliment. Pharmacol. Ther. 47, 16–25 (2018).
Ye, Q. et al. Global prevalence, incidence, and outcomes of non-obese or lean non-alcoholic fatty liver disease: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 5, 739–752 (2020).
Hagstrom, H. et al. Risk for development of severe liver disease in lean patients with nonalcoholic fatty liver disease: a long-term follow-up study. Hepatol. Commun. 2, 48–57 (2018).
Lear, S. A. et al. Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M-CHAT). Am. J. Clin. Nutr. 86, 353–359 (2007).
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363, 157–163 (2004).
Estes, C. et al. Modelling NAFLD disease burden in four Asian regions – 2019-2030. Aliment. Pharmacol. Ther. 51, 801–811 (2020).
Tan, E. K. et al. Liver transplant waitlist outcomes and the allocation of hepatocellular carcinoma model for end-stage liver disease exception points at a low-volume center. Transpl. Proc. 50, 3564–3570 (2018).
Paik, J. M., Golabi, P., Younossi, Y., Mishra, A. & Younossi, Z. M. Changes in the global burden of chronic liver diseases from 2012 to 2017: the growing impact of NAFLD. Hepatology 72, 1605–1616 (2020).
GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016 Lancet 392, 1015–1035 (2018).
World Health Organization Global status report on alcohol and health 2018 (WHO, 2018).
World Health Organization. Global status report on alcohol and health 2014 (WHO, 2014).
Singh, S. K., Kumar, S. Nature, pattern, and changes in alcohol consumption among men in India: insights from NFHS-4 and NFHS-5 J. Ethn. Subst. Abuse, 1–20 https://doi.org/10.1080/15332640.2022.2160853 (2022).
Sharma, M. et al. The pattern of alcohol use in alcohol-related cirrhosis in Indian patients: AUDIT Indian liver study. J. Clin. Exp. Hepatol. 13, 437–446 (2023).
[No authors listed] 2006 Proceedings of the International symposium on alcoholic liver and pancreatic diseases and cirrhosis, 18-19 May 2006, Marina del Rey, California, USA J. Gastroenterol. Hepatol. 21, (Suppl. 3), S1-110 (2006).
Benegal, V. India: alcohol and public health. Addiction 100, 1051–1056 (2005).
Ceni, E., Mello, T. & Galli, A. Pathogenesis of alcoholic liver disease: role of oxidative metabolism. World J. Gastroenterol. 20, 17756–17772 (2014).
Chang, J. S., Hsiao, J. R. & Chen, C. H. ALDH2 polymorphism and alcohol-related cancers in Asians: a public health perspective. J. Biomed. Sci. 24, 19 (2017).
Li, H. et al. Refined geographic distribution of the oriental ALDH2*504Lys (nee 487Lys) variant. Ann. Hum. Genet. 73, 335–345 (2009).
Huang, D. Q., Mathurin, P., Cortez-Pinto, H. & Loomba, R. Global epidemiology of alcohol-associated cirrhosis and HCC: trends, projections and risk factors. Nat. Rev. Gastroenterol. Hepatol. 20, 37–49 (2023).
Devarbhavi, H. et al. Drug-induced liver injury: Asia Pacific Association of Study of Liver consensus guidelines. Hepatol. Int. 15, 258–282 (2021).
Sgro, C. et al. Incidence of drug-induced hepatic injuries: a French population-based study. Hepatology 36, 451–455 (2002).
Suk, K. T. et al. A prospective nationwide study of drug-induced liver injury in Korea. Am. J. Gastroenterol. 107, 1380–1387 (2012).
Shen, T. et al. Incidence and etiology of drug-induced liver injury in mainland China. Gastroenterology 156, 2230–2241.e11 (2019).
Roytman, M. M., Poerzgen, P. & Navarro, V. Botanicals and hepatotoxicity. Clin. Pharmacol. Ther. 104, 458–469 (2018).
Philips, C. A. et al. A single‐center experience on outcomes of complementary and alternative medicine use among patients with cirrhosis. Hepatol. Commun. 3, 1001–1012 (2019).
World Health Organization. Global tuberculosis report 2019 (WHO, 2019).
Saukkonen, J. J. et al. An official ATS statement: hepatotoxicity of antituberculosis therapy. Am. J. Respir. Crit. Care Med. 174, 935–952 (2006).
Philips, C. A., Theruvath, A. H., Ravindran, R. & Augustine, P. Complementary and alternative medicines and liver disease. Hepatol. Commun. 8, e0417 (2024).
Fontana, R. J. et al. AASLD practice guidance on drug, herbal, and dietary supplement-induced liver injury. Hepatology 77, 1036–1065 (2023).
Jindal, A. & Sarin, S. K. Epidemiology of liver failure in Asia-Pacific region. Liver Int. 42, 2093–2109 (2022).
Hao, K. et al. 2014 RUCAM scale-based diagnosis, clinical features and prognosis of 140 cases of drug-induced liver injury [Chinese] Zhonghua Gan Zang Bing Za Zhi 22, 938-941 (2014).
Lei, X. et al. Liver damage associated with Polygonum multiflorum Thunb.: a systematic review of case reports and case series. Evid. Based Complement. Altern. Med. 2015, 459749 (2015).
Yuen, M. F. et al. Traditional Chinese medicine causing hepatotoxicity in patients with chronic hepatitis B infection: a 1-year prospective study. Aliment. Pharmacol. Ther. 24, 1179–1186 (2006).
Navarro, V. J. et al. Liver injury from herbal and dietary supplements. Hepatology 65, 363–373 (2017).
Huang, D. Q. et al. Global epidemiology of cirrhosis – aetiology, trends and predictions. Nat. Rev. Gastroenterol. Hepatol. 20, 388–398 (2023).
Asrani, S. K., Devarbhavi, H., Eaton, J. & Kamath, P. S. Burden of liver diseases in the world. J. Hepatol. 70, 151–171 (2019).
GBD 2017 Cirrhosis Collaborators. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 5, 245–266 (2020).
Asrani, S. K., Larson, J. J., Yawn, B., Therneau, T. M. & Kim, W. R. Underestimation of liver-related mortality in the United States. Gastroenterology 145, 375–382.e2 (2013).
de Franchis, R. et al. Baveno VII – renewing consensus in portal hypertension. J. Hepatol. 76, 959–974 (2022).
Loomba, R. et al. Liver stiffness thresholds to predict disease progression and clinical outcomes in bridging fibrosis and cirrhosis. Gut 72, 581–589 (2023).
Lin, H. et al. Risk and predictors of hepatic decompensation in grey zone patients by the Baveno VII criteria: a competing risk analysis. Aliment. Pharmacol. Ther. 58, 920–928 (2023).
Wong, Y. J. et al. Baveno-VII criteria to predict decompensation and initiate non-selective beta-blocker in compensated advanced chronic liver disease patients. Clin. Mol. Hepatol. 29, 135–145 (2023).
Song, B. G. et al. Validation of non-invasive diagnosis of CSPH in patients with compensated advanced chronic liver disease according to Baveno VII. Liver Int. 43, 1966–1974 (2023).
Trebicka, J. et al. The PREDICT study uncovers three clinical courses of acutely decompensated cirrhosis that have distinct pathophysiology. J. Hepatol. 73, 842–854 (2020).
Luo, J. et al. Acute-on-chronic liver failure: far to go – a review. Crit. Care 27, 259 (2023).
Sarin, S. K. et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific Association for the Study of the Liver (APASL): an update. Hepatol. Int. 13, 353–390 (2019).
Qin, G. et al. Population-representative incidence of acute-on-chronic liver failure: a prospective cross-sectional study. J. Clin. Gastroenterol. 50, 670–675 (2016).
Chetwood, J. D. et al. Epidemiology, characteristics, and outcomes of patients with acute-on-chronic liver failure in Australia. J. Gastroenterol. Hepatol. 38, 1325–1332 (2023).
Kulkarni, A. V. et al. Early diagnosis and prevention of infections in cirrhosis. Semin. Liver Dis. 42, 293–312 (2022).
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Global Cancer Observatory. Cancer Today. Lyon, France: International Agency for Research on Cancer https://gco.iarc.who.int/today (2022).
Sim, Y. K. et al. Real-world data on the diagnosis, treatment, and management of hepatocellular carcinoma in the Asia-Pacific: the INSIGHT study Liver Cancer 13, 298–313 (2023).
Huang, D. Q. et al. Changing global epidemiology of liver cancer from 2010 to 2019: NASH is the fastest growing cause of liver cancer. Cell Metab. 34, 969–977.e2 (2022).
Australian Institute of Health and Welfare. Cancer in Australia 2017. Cancer Series No. 101. Australian Institute of Health and Welfare www.aihw.gov.au/getmedia/3da1f3c2-30f0-4475-8aed-1f19f8e16d48/20066-cancer-2017.pdf.aspx?inline=true (2017).
Chang, M. H. et al. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. Taiwan Childhood Hepatoma Study Group. N. Engl. J. Med. 336, 1855–1859 (1997).
World Health Organization. Hepatitis B vaccination coverage. WHO https://www.who.int/news-room/fact-sheets/detail/immunization-coverage (2022).
Chen, C. J., Wang, L. Y. & Yu, M. W. Epidemiology of hepatitis B virus infection in the Asia-Pacific region. J. Gastroenterol. Hepatol. 15, E3–E6 (2000).
Le, L. V. et al. Progress towards achieving viral hepatitis B and C elimination in the Asia and Pacific region: results from modelling and global reporting. Liver Int. 42, 1930–1934 (2022).
Razavi-Shearer, D. et al. The disease burden of hepatitis B and hepatitis C from 2015 to 2030: the long and winding road [abstract OS050] J. Hepatol. 77, (Suppl. 1) 43 (2022).
Huang, Y. T. et al. Lifetime risk and sex difference of hepatocellular carcinoma among patients with chronic hepatitis B and C. J. Clin. Oncol. 29, 3643–3650 (2011).
Wong, G. L. et al. An aging population of chronic hepatitis B with increasing comorbidities: a territory-wide study from 2000 to 2017. Hepatology 71, 444–455 (2020).
Tseng, C. H., Hsu, Y. C., Ho, H. J., Nguyen, M. H. & Wu, C. Y. Increasing age and nonliver comorbidities in patients with chronic hepatitis B in Taiwan: a nationwide population-based analysis. Dig. Dis. 39, 266–274 (2021).
Kudaravalli, S. et al. Sex and ethnic disparities in hepatitis B evaluation and treatment across the world. J. Hepatol. 81, 33–41 (2024).
Huang, D. Q. et al. Antiviral therapy utilization and 10-year outcomes in resected hepatitis B virus- and hepatitis C virus-related hepatocellular carcinoma. J. Clin. Oncol. 42, 790–799 (2024).
Nguyen, V. H. et al. Characteristics and treatment rate of patients with hepatitis C virus infection in the direct-acting antiviral era and during the COVID-19 pandemic in the United States. JAMA Netw. Open. 5, e2245424 (2022).
Ogawa, E. et al. Association of direct-acting antiviral therapy with liver and nonliver complications and long-term mortality in patients with chronic hepatitis C. JAMA Intern. Med. 183, 97–105 (2023).
Paik, J. M. et al. The burden of nonalcoholic fatty liver disease (NAFLD) is rapidly growing in every region of the world from 1990 to 2019. Hepatol. Commun. 7, e0251 (2023).
Estes, C. et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030. J. Hepatol. 69, 896–904 (2018).
Manthey, J. et al. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: a modelling study. Lancet 393, 2493–2502 (2019).
World Health Organization. Health situation in South-East Asia region 2001–2007 (WHO, 2008).
Li, M. et al. Mapping the incidence of drug-induced liver injury: a systematic review and meta-analysis. J. Dig. Dis. 24, 332–339 (2023).
Wong, M. C. S. et al. The changing epidemiology of liver diseases in the Asia-Pacific region. Nat. Rev. Gastroenterol. Hepatol. 16, 57–73 (2019).
Alaama, A. S. et al. Progress towards elimination of viral hepatitis by 2030 in the WHO Eastern Mediterranean Region, 2019. Lancet Gastroenterol. Hepatol. 7, 862–870 (2022).
Sarin, S. K. et al. Liver diseases in the Asia-Pacific region: a Lancet Gastroenterology & Hepatology Commission. Lancet Gastroenterol. Hepatol. 5, 167–228 (2020).
Xu, H., Xiao, P., Zhang, F., Liu, T. & Gao, Y. Epidemic characteristics of alcohol-related liver disease in Asia from 2000 to 2020: a systematic review and meta-analysis. Liver Int. 42, 1991–1998 (2022).
Bajaj, J. S. et al. Global disparities in mortality and liver transplantation in hospitalised patients with cirrhosis: a prospective cohort study for the CLEARED Consortium. Lancet Gastroenterol. Hepatol. 8, 611–622 (2023).
Tan, E. X.-X. et al. Impact of COVID-19 on liver transplantation in Hong Kong and Singapore: a modelling study. Lancet Reg. Health West. Pac. 16, 100262 (2021).
Kumar, P. et al. Severe acute respiratory syndrome coronavirus 2-related acute-on-chronic liver failure. J. Clin. Exp. Hepatol. 11, 404–406 (2021).
Görgülü, E. et al. Acute-on-chronic liver failure (ACLF) precipitated by severe alcoholic hepatitis: another collateral damage of the COVID-19 pandemic? Gut 71, 1036–1038 (2022).
Bertuccio, P. et al. Global trends and predictions in hepatocellular carcinoma mortality. J. Hepatol. 67, 302–309 (2017).
Chen, J. G. et al. Reduced aflatoxin exposure presages decline in liver cancer mortality in an endemic region of China. Cancer Prev. Res. 6, 1038–1045 (2013).
Fan, J. H. et al. Attributable causes of liver cancer mortality and incidence in China. Asian Pac. J. Cancer Prev. 14, 7251–7256 (2013).
Arnold, M. et al. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology 159, 335–349 (2020).
Liu, Y. & Liu, L. Changes in the epidemiology of hepatocellular carcinoma in Asia. Cancers 14, 4473 (2022).
Petrick, J. L. et al. International trends in hepatocellular carcinoma incidence, 1978–2012. Int. J. Cancer 147, 317–330 (2020).
Yip, T. C. F., Lee, H. W., Chan, W. K., Wong, G. L. H. & Wong, V. W. S. Asian perspective on NAFLD-associated HCC. J. Hepatol. 76, 726–734 (2022).
Koh, J. H. et al. NAFLD and NAFLD-related HCC in Asia: burden and surveillance. J. Clin. Exp. Hepatol. 14, 101213 (2024).
Huang, D. Q., El-Serag, H. B. & Loomba, R. Global epidemiology of NAFLD-related HCC: trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 18, 223–238 (2021).
Rui, F. et al. Development of a machine learning-based model to predict hepatic inflammation in chronic hepatitis B patients with concurrent hepatic steatosis: a cohort study. EClinicalMedicine 68, 102419 (2024).
Chan, A. W. H. et al. Concurrent fatty liver increases risk of hepatocellular carcinoma among patients with chronic hepatitis B. J. Gastroenterol. Hepatol. 32, 667–676 (2017).
Cho, E. J. et al. Relative etiological role of prior hepatitis B virus infection and nonalcoholic fatty liver disease in the development of non-B non-C hepatocellular carcinoma in a hepatitis B-endemic area. Digestion 84, 17–22 (2011).
Tateishi, R. et al. A nationwide survey on non-B, non-C hepatocellular carcinoma in Japan: 2011-2015 update. J. Gastroenterol. 54, 367–376 (2019).
Omata, M. et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol. Int. 11, 317–370 (2017).
Bhatti, A. B. H. et al. Hepatocellular carcinoma in Pakistan: national trends and global perspective. Gastroenterol. Res. Pract. 2016, 5942306 (2016).
Global Burden of Disease Liver Cancer Collaboration. et al. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: results from the Global Burden of Disease Study 2015. JAMA Oncol. 3, 1683–1691 (2017).
World Health Organization. Guidelines for the prevention, diagnosis, care and treatment for people with chronic hepatitis B infection. WHO www.who.int/publications/i/item/9789240090903 (2024).
Pan, C. Q. et al. Tenofovir to prevent hepatitis B transmission in mothers with high viral load. N. Engl. J. Med. 374, 2324–2334 (2016).
World Health Organization. Global hepatitis report 2024: action for access in low- and middle-income countries. WHO www.who.int/publications/i/item/9789240091672 (2024).
European Association for the Study of the Liver EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J. Hepatol. 67 370–398 (2017).
Terrault, N. A. et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology 67, 1560–1599 (2018).
Lau, G. et al. APASL clinical practice guideline on hepatitis B reactivation related to the use of immunosuppressive therapy. Hepatol. Int. 15, 1031–1048 (2021).
Tan, E. X. et al. Upper limit of normal ALT levels in health and metabolic diseases: pooled analysis of 423,355 individuals with bootstrap modelling. Aliment. Pharmacol. Ther. 59, 984–992 (2024).
Kudaravalli, S., Kam, L. Y., Huang, D. Q., Cheung, R. & Nguyen, M. H. Utilization of antiviral therapy for patients with hepatitis B-related hepatocellular carcinoma: a nationwide real-world US study. Clin. Gastroenterol. Hepatol. 21, 3305–3313.e4 (2023).
Huang, D. Q. et al. Natural history and hepatocellular carcinoma risk in untreated chronic hepatitis B patients with indeterminate phase. Clin. Gastroenterol. Hepatol. 20, 1803–1812.e5 (2022).
Sinn, D. H., Kim, S. E., Kim, B. K., Kim, J. H. & Choi, M. S. The risk of hepatocellular carcinoma among chronic hepatitis B virus-infected patients outside current treatment criteria. J. Viral Hepat. 26, 1465–1472 (2019).
Huang, D. Q. et al. Liver complications in untreated treatment-ineligible versus treated treatment-eligible patients with hepatitis B. Dig. Dis. 41, 115–123 (2022).
Hsu, Y. C. et al. Once-daily tenofovir disoproxil fumarate in treatment-naive Taiwanese patients with chronic hepatitis B and minimally raised alanine aminotransferase (TORCH-B): a multicentre, double-blind, placebo-controlled, parallel-group, randomised trial. Lancet Infect. Dis. 21, 823–833 (2021).
Hsu, Y. C. et al. Inhibition of viral replication reduces transcriptionally active distinct hepatitis B virus integrations with implications on host gene dysregulation. Gastroenterology 162, 1160–1170.e1 (2022).
Lim, Y. S. et al. Impact of expanding hepatitis B treatment guidelines: a modelling and economic impact analysis. Aliment. Pharmacol. Ther. 56, 519–528 (2022).
Huang, D. Q. et al. Antiviral therapy substantially reduces HCC risk in patients with chronic hepatitis B infection in the indeterminate phase. Hepatology 78, 1558–1568 (2023).
You, H. et al. Guidelines for the prevention and treatment of chronic hepatitis B (version 2022). J. Clin. Transl. Hepatol. 11, 1425–1442 (2023).
Martinello, M., Solomon, S. S., Terrault, N. A. & Dore, G. J. Hepatitis C. Lancet 402, 1085–1096 (2023).
Wait, S. et al. Hepatitis B and hepatitis C in southeast and southern Asia: challenges for governments. Lancet Gastroenterol. Hepatol. 1, 248–255 (2016).
Lazarus, J. V., Wiktor, S., Colombo, M., Thursz, M. & Foundation, E. I. L. Micro-elimination – a path to global elimination of hepatitis C. J. Hepatol. 67, 665–666 (2017).
Grebely, J. et al. Single-visit hepatitis C point-of-care testing, linkage to nursing care, and peer-supported treatment among people with recent injecting drug use at a peer-led needle and syringe program: The TEMPO Pilot Study. Int. J. Drug Policy 114, 103982 (2023).
Huang, C. F., Chen, G. J., Hung, C. C. & Yu, M. L. HCV microelimination for high-risk special populations. J. Infect. Dis. 228, S168–s179 (2023).
Dhiman, R. K. et al. Outcomes of real-world integrated HCV microelimination for people who inject drugs: an expansion of the Punjab model. eClinicalMedicine 41, 101148 (2021).
Doyle, J. S. et al. Microelimination of hepatitis C among people with human immunodeficiency virus coinfection: declining incidence and prevalence accompanying a multicenter treatment scale-up trial. Clin. Infect. Dis. 73, e2164–e2172 (2021).
Huang, C. I. et al. A people-centered decentralized outreach model toward HCV micro-elimination in hyperendemic areas: COMPACT study in SARS Co-V2 pandemic. J. Microbiol. Immunol. Infect. 56, 586–597 (2023).
Papaluca, T. et al. Outcomes of treatment for hepatitis C in prisoners using a nurse-led, statewide model of care. J. Hepatol. 70, 839–846 (2019).
Wong, Y. J. et al. The impact of unrestricted access to direct-acting antiviral among incarcerated hepatitis C virus-infected patients. Clin. Mol. Hepatol. 27, 474–485 (2021).
Mak, L. Y. et al. Conquering hepatitis via micro-elimination (CHIME) program for chronic hepatitis C infection in high-risk populations in Hong Kong: final results [abstract 1818-A] Hepatology 78, (Suppl. 677-678) (2023).
Sanyal, A. J. et al. Prospective study of outcomes in adults with nonalcoholic fatty liver disease. N. Engl. J. Med. 385, 1559–1569 (2021).
Harrison, S. A. et al. A phase 3, randomized, controlled trial of resmetirom in NASH with liver fibrosis. N. Engl. J. Med. 390, 497–509 (2024).
Tan, C.-K., Goh, G. B.-B., Youn, J., Yu, J. C.-K. & Singh, S. Public awareness and knowledge of liver health and diseases in Singapore. J. Gastroenterol. Hepatol. 36, 2292–2302 (2021).
Gracen, L. et al. An exploration of barriers and facilitators to implementing a nonalcoholic fatty liver disease pathway for people with type 2 diabetes in primary care. Diabet. Med. 39, e14799 (2022).
Younossi, Z. M. et al. Global survey of stigma among physicians and patients with nonalcoholic fatty liver disease. J. Hepatol. 80, 419–430 (2024).
Serra-Burriel, M. et al. Development, validation, and prognostic evaluation of a risk score for long-term liver-related outcomes in the general population: a multicohort study. Lancet 402, 988–996 (2023).
Noureddin, M. MASH clinical trials and drugs pipeline: an impending Tsunami. Hepatology https://doi.org/10.1097/HEP.0000000000000860 (2024).
Lim, W. H. et al. Meta-analysis: prevalence and impact of alcohol abstinence in alcohol-associated cirrhosis. Aliment. Pharmacol. Ther. 59, 730–741 (2024).
Allen, L. N. et al. Socioeconomic status and alcohol use in low- and lower-middle income countries: a systematic review. Alcohol 70, 23–31 (2018).
Wyper, G. M. A. et al. Evaluating the impact of alcohol minimum unit pricing on deaths and hospitalisations in Scotland: a controlled interrupted time series study. Lancet 401, 1361–1370 (2023).
Hu, A. et al. The transition of alcohol control in China 1990-2019: impacts and recommendations. Int. J. Drug Policy 105, 103698 (2022).
Sornpaisarn, B. et al. Alcohol consumption and attributable harm in middle-income South-East Asian countries: epidemiology and policy options. Int. J. Drug Policy 83, 102856 (2020).
Im, G. Y. et al. Provider attitudes and practices for alcohol screening, treatment, and education in patients with liver disease: a survey from the American Association for the Study of Liver Diseases alcohol-associated liver disease special interest group. Clin. Gastroenterol. Hepatol. 19, 2407–2416.e8 (2021).
World Health Organization. Global report on traditional and complementary medicine. WHO iris.who.int/bitstream/handle/10665/312342/9789241515436-eng.pdf?sequence=1 (2019).
Mao, Y. et al. Chinese guideline for the diagnosis and treatment of drug-induced liver injury: an update. Hepatol. Int. 18, 384–419 (2024).
Labenz, C. et al. Structured early detection of asymptomatic liver cirrhosis: results of the population-based liver screening program SEAL. J. Hepatol. 77, 695–701 (2022).
Ishtiaq, A., Shah, S., Iftikhar, S., Baig-Ansari, N. & Ashraf, H. Relationship of FIB-4 index with transient elastography in chronic hepatitis C patients having APRI ≥0.5 – ≤2 in a resource-limited setting in Pakistan. J. Fam. Med. Prim. Care 9, 5564–5573 (2020).
Lai, M. & Afdhal, N. H. Liver fibrosis determination. Gastroenterol. Clin. North. Am. 48, 281–289 (2019).
Kaplan, D. E. et al. AASLD Practice Guidance on risk stratification and management of portal hypertension and varices in cirrhosis. Hepatology 79, 1180–1211 (2023).
Rana, R. et al. Evaluating the practice of prescribing beta-blockers in compensated cirrhosis by gastroenterologists in the Asia Pacific Region. J. Clin. Exp. Hepatol. 13, 380–383 (2023).
Ozturk, N. B. et al. Liver transplantation in developing countries. Hepatol. Forum 3, 103–107 (2022).
Rela, M. & Rammohan, A. Why are there so many liver transplants from living donors in Asia and so few in Europe and the US? J. Hepatol. 75, 975–980 (2021).
Kim, D. S. et al. Asian Pacific Association for the Study of the Liver clinical practice guidelines on liver transplantation. Hepatol. Int. 18, 299–383 (2024).
Cho, Y., Kim, B. H. & Park, J. W. Overview of Asian clinical practice guidelines for the management of hepatocellular carcinoma: an Asian perspective comparison. Clin. Mol. Hepatol. 29, 252–262 (2023).
Kulkarni, A. V. & Sarin, S. K. Acute-on-chronic liver failure – steps for harmonization of the definition! J. Hepatol. https://doi.org/10.1016/j.jhep.2024.03.036 (2024).
World Health Organization. Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021: accountability for the global health sector strategies 2016–2021: Actions for Impact. WHO www.who.int/publications/i/item/9789240027077 (2021).
Dang, H. et al. Cure with interferon-free direct-acting antiviral is associated with increased survival in patients with hepatitis C virus-related hepatocellular carcinoma from both East and West. Hepatology 71, 1910–1922 (2020).
Chan, T. T. et al. Positive hepatitis B core antibody is associated with cirrhosis and hepatocellular carcinoma in nonalcoholic fatty liver disease. Am. J. Gastroenterol. 115, 867–875 (2020).
Singal, A. G. et al. HCC surveillance improves early detection, curative treatment receipt, and survival in patients with cirrhosis: a meta-analysis. J. Hepatol. 77, 128–139 (2022).
Zhao, C. et al. Poor adherence to hepatocellular carcinoma surveillance: a systematic review and meta-analysis of a complex issue. Liver Int. 38, 503–514 (2018).
Wolf, E., Rich, N. E., Marrero, J. A., Parikh, N. D. & Singal, A. G. Use of hepatocellular carcinoma surveillance in patients with cirrhosis: a systematic review and meta-analysis. Hepatology 73, 713–725 (2021).
Huang, D. Q. et al. Hepatocellular carcinoma surveillance – utilization, barriers and the impact of changing aetiology. Nat. Rev. Gastroenterol. Hepatol. 20, 797–809 (2023).
Chang, S. S. et al. Factors associated with nonadherence to surveillance for hepatocellular carcinoma among patients with hepatic C virus cirrhosis, 2000-2015. Medicine 101, e31907 (2022).
Trapani, D. et al. Distribution of the workforce involved in cancer care: a systematic review of the literature. ESMO Open. 6, 100292 (2021).
Metreau, E., Young, K. E. & Eapen, S. G. World Bank Group country classifications by income level for 2024–2025 (World Bank, 2024).
Mathew, A. Global survey of clinical oncology workforce. J. Glob. Oncol. 4, 1–12 (2018).
Fundytus, A. et al. Access to cancer medicines deemed essential by oncologists in 82 countries: an international, cross-sectional survey. Lancet Oncol. 22, 1367–1377 (2021).
Lewis, S. et al. Stereotactic body radiation therapy for hepatocellular carcinoma: from infancy to ongoing maturity. JHEP Rep. 4, 100498 (2022).
Abu Awwad, D. et al. Current and projected gaps in the availability of radiotherapy in the Asia-Pacific region: a country income-group analysis. Lancet Oncol. 25, 225–234 (2024).
Finn, R. S. et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N. Engl. J. Med. 382, 1894–1905 (2020).
Cheng, A. L. et al. Updated efficacy and safety data from IMbrave150: Atezolizumab plus bevacizumab vs. sorafenib for unresectable hepatocellular carcinoma. J. Hepatol. 76, 862–873 (2022).
Tan, D. J. H. et al. Survival trends in sorafenib for advanced hepatocellular carcinoma: a reconstructed individual patient data meta-analysis of randomized trials. Liver Cancer 12, 445–456 (2023).
Vogel, A., Martinelli, E. Updated treatment recommendations for hepatocellular carcinoma (HCC) from the ESMO Clinical Practice Guidelines Ann. Oncol. 32 801–805 (2023).
Hofmarcher, T., Keel, G. & Lindgren, P. Cancer care and access to cancer drugs in Asia-Pacific. Swedish Institute for Health Economics ihe.se/en/rapport/cancer-care-and-access-to-cancer-drugs-in-asia-pacific/ (2021).
Loong, H. H., Tan, D. S. W. & Shimizu, T. Challenges and insights of early phase oncology drug development in the Asia-Pacific region. Chin. Clin. Oncol. 8, 26 (2019).
Vista Health. Eliminating Asia’s silent emergency: hepatocellular carcinoma and hepatitis white paper. APAC Liver Disease Alliance https://liverwell.org.au/wp-content/uploads/2023/07/Hepatitis-and-HCC-Elimination-in-APAC_White-Paper_Summary.pdf (2023).
Barrios, C. et al. Barriers in access to oncology drugs – a global crisis. Nat. Rev. Clin. Oncol. 20, 7–15 (2023).
Eniu, A. et al. Cancer medicines in Asia and Asia-Pacific: what is available, and is it effective enough? ESMO Open. 4, e000483 (2019).
World Health Organization. Social determinants of health. WHO www.who.int/health-topics/social-determinants-of-health#tab=tab_1 (2024).
Schulz, T. R., Kanhutu, K., Sasadeusz, J., Watkinson, S. & Biggs, B. A. Using telehealth to improve access to hepatitis C treatment in the direct-acting antiviral therapy era. J. Telemed. Telecare 26, 180–185 (2020).
Cuadrado, A. et al. Telemedicine efficiently improves access to hepatitis C management to achieve HCV elimination in the penitentiary setting. Int. J. Drug Policy 88, 103031 (2021).
Markby, J. et al. Feasibility, effectiveness and cost of a decentralized HCV care model among the general population in Delhi, India. Liver Int. 42, 532–540 (2022).
Markby, J. et al. Assessing the impact of simplified HCV care on linkage to care amongst high-risk patients at primary healthcare clinics in Malaysia: a prospective observational study. BMJ Open. 11, e055142 (2021).
Oru, E., Trickey, A., Shirali, R., Kanters, S. & Easterbrook, P. Decentralisation, integration, and task-shifting in hepatitis C virus infection testing and treatment: a global systematic review and meta-analysis. Lancet Glob. Health 9, e431–e445 (2021).
Masoodi, M. et al. Metabolomics and lipidomics in NAFLD: biomarkers and non-invasive diagnostic tests. Nat. Rev. Gastroenterol. Hepatol. 18, 835–856 (2021).
Pirola, C. J. et al. The influence of host genetics on liver microbiome composition in patients with NAFLD. EBioMedicine 76, 103858 (2022).
Trépo, E. & Valenti, L. Update on NAFLD genetics: from new variants to the clinic. J. Hepatol. 72, 1196–1209 (2020).
Sharma, D. & Mandal, P. NAFLD: genetics and its clinical implications. Clin. Res. Hepatol. Gastroenterol. 46, 102003 (2022).
Díaz, L. A. et al. Association between public health policies on alcohol and worldwide cancer, liver disease and cardiovascular disease outcomes. J. Hepatol. 80, 409–418 (2024).
Avila, M. A. et al. Recent advances in alcohol-related liver disease (ALD): summary of a Gut round table meeting. Gut 69, 764–780 (2020).
Ghabril, M. et al. Eight-fold increase in dietary supplement-related liver failure leading to transplant waitlisting over the last quarter century in the United States. Liver Transpl. 28, 169–179 (2022).
Sebastiani, G. et al. Prediction of oesophageal varices in hepatic cirrhosis by simple serum non-invasive markers: results of a multicenter, large-scale study. J. Hepatol. 53, 630–638 (2010).
Yeow, M. et al. Liver transplantation in Singapore: challenges and strategies of low- to mid-volume centers. Transplantation 106, 895–897 (2022).
Fan, R. et al. aMAP risk score predicts hepatocellular carcinoma development in patients with chronic hepatitis. J. Hepatol. 73, 1368–1378 (2020).
Hsu, Y. C. et al. Development of a scoring system to predict hepatocellular carcinoma in Asians on antivirals for chronic hepatitis B. J. Hepatol. 69, 278–285 (2018).
Yang, H. I. et al. Real-world effectiveness from the Asia Pacific Rim Liver Consortium for HBV risk score for the prediction of hepatocellular carcinoma in chronic hepatitis B patients treated with oral antiviral therapy J. Infect. Dis. 221, 389–399 (2020).
Ioannou, G. N. HCC surveillance after SVR in patients with F3/F4 fibrosis. J. Hepatol. 74, 458–465 (2021).
Curran, C. et al. Hepatocellular carcinoma risk scores predict patients under surveillance at low risk of benefit and high risk of harm. Dig. Dis. Sci. 68, 770–777 (2023).
Srivastava, A. et al. Tracking the workforce 2020-2030: making the case for a cancer workforce registry. JCO Glob. Oncol. 7, 925–933 (2021).
Ong, S. K. et al. Mapping recommendations towards an Asian Code Against Cancer (ACAC) as part of the World Code Against Cancer Framework: an Asian National Cancer Centers Alliance (ANCCA) initiative Health Policy 24, 10016 (2024).
Le, M. H. et al. Global incidence of adverse clinical events in non-alcoholic fatty liver disease: a systematic review and meta-analysis. Clin. Mol. Hepatol. 30, 235–246 (2024).
Rinella, M. E. et al. AASLD practice guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology 77, 1797–1835 (2023).
Acknowledgements
The authors are members of the Asian Pacific Association of Gastroenterology (APAGE) Emerging Leaders Committee, and thank APAGE for supporting the formation of this committee.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
L.-Y.M. served on the advisory board for Gilead Sciences and Roche Diagnostics. K.C.Y. was a speaker for Gilead and AbbVie, and received a grant supported by the Educate, Test, Treat! Programme, which was funded in part by Gilead Sciences Inc. R.L. has served as an advisory board member for Gilead Sciences, speaker for GenieBiome, and owns equity in Pfizer. J.C.-T.L. served as a speaker for Gilead Sciences, and served on an advisory board committee for Gilead Sciences and Boehringer Ingelheim. Y.C.H. has received research grants from Gilead Sciences, served on advisory committees for Gilead Sciences and Sysmex, and received lecture fees from Abbvie, Bristol-Myers Squibb, Gilead Sciences, Merck Sharp & Dohme and Novartis. D.Q.H. has served on the advisory board for Gilead Sciences and Roche Diagnostics. The other authors have no competing interests to declare.
Peer review
Peer review information
Nature Reviews Gastroenterology & Hepatology thanks Vincent Chen and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mak, LY., Liu, K., Chirapongsathorn, S. et al. Liver diseases and hepatocellular carcinoma in the Asia-Pacific region: burden, trends, challenges and future directions. Nat Rev Gastroenterol Hepatol (2024). https://doi.org/10.1038/s41575-024-00967-4
Accepted:
Published:
DOI: https://doi.org/10.1038/s41575-024-00967-4