Abstract
Epidemiology studies have demonstrated a clear association between obesity and the development of several distinct malignancies, with excessive visceral adiposity being an increasingly prevalent feature in patients with cancer presenting for therapeutic intervention. Clinical trials and meta-analyses have helped to inform effective and safe dosing of traditional systemically administered anticancer agents in adult patients with cancer and obesity, but there remains much debate not only regarding the effect of obesity on the more novel targeted molecular and immune-based therapies, but also about how obesity is best defined and measured clinically. Low muscle mass is associated with poor outcomes in cancer, and body composition studies using biochemical and imaging modalities are helping to fully delineate the importance of both obesity and sarcopenia in clinical outcomes; such studies might also go some way to explaining how obesity can paradoxically be associated with favourable clinical outcomes in certain cancers. As the cancer survivorship period increases and the duration of anticancer treatment lengthens, this Review highlights the challenges facing appropriate treatment selection and emphasizes how a multidisciplinary approach is warranted to manage weight and skeletal muscle loss during and after cancer treatment.
Key points
-
Obesity drives pathological inflammation and simultaneously disrupts ongoing antitumour immune responses.
-
Patients with overweight or obesity and low muscle mass experience more surgical complications, treatment-related toxicities, a higher risk of recurrence and cancer-specific mortality than patients with a BMI in the normal range.
-
Research into dose optimization in patients with cancer and obesity is required, focusing on how body composition and BMI can affect drug distribution, dosing and toxicities.
-
Both muscle mass and quality are important factors to consider when assessing the functional influence of sarcopenia and obesity on toxicities and outcomes following cancer treatment.
-
During cancer treatment, patients with cancer can experience unintentional muscle loss owing to factors including treatment adverse effects, changes in food taste and changes in lifestyle.
-
The interplay of obesity with sex, psychosocial and socioeconomic factors influences access to cancer screening, diagnosis and treatments, ultimately affecting outcomes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Lobstein, T., Brinsden, H. & Neveux, M. World Obesity Atlas 2022. World Obesity Forum https://s3-eu-west-1.amazonaws.com/wof-files/World_Obesity_Atlas_2022.pdf (2022).
World Health Organization. Obesity and overweight. WHO https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (2024).
Gesta, S., Tseng, Y. H. & Kahn, C. R. Developmental origin of fat: tracking obesity to its source. Cell 131 (2), 242–256 (2007).
Shuster, A. et al. The clinical importance of visceral adiposity: a critical review of methods for visceral adipose tissue analysis. Br. J. Radiol. 85 (1009), 1–10 (2012).
van Vliet-Ostaptchouk, J. V. et al. The prevalence of metabolic syndrome and metabolically healthy obesity in Europe: a collaborative analysis of ten large cohort studies. BMC Endocr. Disord. 14, 9 (2014).
Crewe, C., An, Y. A. & Scherer, E. The ominous triad of adipose tissue dysfunction: inflammation, fibrosis, and impaired angiogenesis. J. Clin. Invest. 127 (1), 74–82 (2017).
Avgerinos, K. I. et al. Obesity and cancer risk: emerging biological mechanisms and perspectives. Metabolism 92, 121–135 (2019).
Lauby-Secretan, B. et al. Body fatness and cancer – viewpoint of the IARC Working Group. N. Engl. J. Med. 375 (8), 794–798 (2016). The IARC Working Group concludes that the absence of excess adiposity lowers the risk of most cancers and supports the thesis that intentional weight loss might have a cancer-preventive effect.
Marinac, C. R. et al. Body mass index throughout adulthood, physical activity, and risk of multiple myeloma: a prospective analysis in three large cohorts. Br. J. Cancer 118 (7), 1013–1019 (2018).
Prado, C. M. et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol. 9 (7), 629–635 (2008). This study showed that, in patients with cancer of the respiratory and gastrointestinal tracts, sarcopenic obesity is associated with poorer functional status than obesity without sarcopenia, and identified sarcopenic obesity as an independent predictor of survival.
Cabia, B. et al. A role for novel adipose tissue-secreted factors in obesity-related carcinogenesis. Obes. Rev. 17 (4), 361–376 (2016).
Maurizi, G. et al. Adipocytes properties and crosstalk with immune system in obesity-related inflammation. J. Cell Physiol. 233 (1), 88–97 (2018).
Nishimura, S. et al. CD8+ effector T cells contribute to macrophage recruitment and adipose tissue inflammation in obesity. Nat. Med. 15 (8), 914–920 (2009).
O’Rourke, R. W. et al. Systemic NK cell ablation attenuates intra-abdominal adipose tissue macrophage infiltration in murine obesity. Obesity 22 (10), 2109–2114 (2014).
Pecht, T. et al. Peripheral blood leucocyte subclasses as potential biomarkers of adipose tissue inflammation and obesity subphenotypes in humans. Obes. Rev. 15 (4), 322–337 (2014).
Wensveen, F. M. et al. The “big bang” in obese fat: events initiating obesity-induced adipose tissue inflammation. Eur. J. Immunol. 45 (9), 2446–2456 (2015).
Conroy, M. J. et al. Parallel profiles of inflammatory and effector memory T cells in visceral fat and liver of obesity-associated cancer patients. Inflammation 39 (5), 1729–1736 (2016).
Conroy, M. J. et al. Identifying a novel role for fractalkine (CX3CL1) in memory CD8+ T cell accumulation in the omentum of obesity-associated cancer patients. Front Immunol. 9, 1867 (2018).
Mylod, E. et al. The omentum in obesity-associated cancer: a hindrance to effective natural killer cell migration towards tumour which can be overcome by CX3CR1 antagonism. Cancers 14, 64 (2021).
Smit, C. et al. Obesity and drug pharmacology: a review of the influence of obesity on pharmacokinetic and pharmacodynamic parameters. Expert Opin. Drug Metab. Toxicol. 14 (3), 275–285 (2018).
European Medicines Agency. Reflection paper on investigation of pharmacokinetics and pharmacodynamics in the obese population. Citeline https://pink.citeline.com/-/media/supporting-documents/pink-sheet/2018/03/ema_24_wc500242971.pdf (2018).
Food & Drug Administration. Project Optimus. FDA https://www.fda.gov/about-fda/oncology-center-excellence/project-optimus. (2024).
Field, K. M. et al. Chemotherapy dosing strategies in the obese, elderly, and thin patient: results of a nationwide survey. J. Oncol. Pract. 4 (3), 108–113 (2008).
Griggs, J. J. et al. Appropriate chemotherapy dosing for obese adult patients with cancer: American Society of Clinical Oncology clinical practice guideline. J. Clin. Oncol. 30 (13), 1553–1561 (2012).
Lyman, G. H. Impact of chemotherapy dose intensity on cancer patient outcomes. J. Natl Compr. Canc Netw. 7 (1), 99–108 (2009).
Pinkel, D. The use of body surface area as a criterion of drug dosage in cancer chemotherapy. Cancer Res. 18 (7), 853–856 (1958).
Hunter, R. J. et al. Dosing chemotherapy in obese patients: actual versus assigned body surface area (BSA). Cancer Treat. Rev. 35 (1), 69–78 (2009).
Griggs, J. J. et al. Appropriate systemic therapy dosing for obese adult patients with cancer: ASCO guideline update. J. Clin. Oncol. 39 (18), 2037–2048 (2021). Updated ASCO guidelines on dosing for chemotherapy, targeted therapies and immunotherapies for adult patients with cancer and obesity.
Rossi, T. et al. Obesity and dose of anti-cancer therapy: are we sure to be on the right track in the precision medicine era? Front. Med. 8, 725346 (2021).
Araujo, D. et al. Oncology phase I trial design and conduct: time for a change – MDICT Guidelines 2022. Ann. Oncol. 34 (1), 48–60 (2023).
Murphy, R., Halford, S. & Symeonides, S. N. Project Optimus, an FDA initiative: considerations for cancer drug development internationally, from an academic perspective. Front. Oncol. 13, 1144056 (2023).
Slawinski, C. G. V. et al. Obesity and cancer treatment outcomes: interpreting the complex evidence. Clin. Oncol. 32 (9), 591–608 (2020).
Shayne, M., Harvey, R. D. & Lyman, G. H. Prophylaxis and treatment strategies for optimizing chemotherapy relative dose intensity. Expert Rev. Anticancer Ther. 21 (10), 1145–1159 (2021).
Nielson, C. M. et al. Relative dose intensity of chemotherapy and survival in patients with advanced stage solid tumor cancer: a systematic review and meta-analysis. Oncologist 26 (9), e1609–e1618 (2021).
Kjeldsted, E. et al. Patient-related characteristics associated with treatment modifications and suboptimal relative dose intensity of neoadjuvant chemotherapy in patients with breast cancer – a retrospective study. Cancers 15, 2483 (2023).
Martin, A. L. et al. Impact of obesity on chemotherapy dosing of carboplatin and survival of women with ovarian cancer. Br. J. Cancer 128 (12), 2236–2242 (2023).
Liu, Y. et al. Host obesity alters the ovarian tumor immune microenvironment and impacts response to standard of care chemotherapy. J. Exp. Clin. Cancer Res. 42 (1), 165 (2023).
Garibaldi, C. et al. Recent advances in radiation oncology. Ecancermedicalscience 11, 785 (2017).
Hu, M. B. et al. Obesity has multifaceted impact on biochemical recurrence of prostate cancer: a dose-response meta-analysis of 36,927 patients. Med. Oncol. 31 (2), 829 (2014).
Wang, L. S. et al. Impact of obesity on outcomes after definitive dose-escalated intensity-modulated radiotherapy for localized prostate cancer. Cancer 121 (17), 3010–3017 (2015).
Ross, K. H. et al. Obesity and cancer treatment efficacy: existing challenges and opportunities. Cancer 125 (10), 1588–1592 (2019).
Winters, E. & Poole, C. Challenges and impact of patient obesity in radiation therapy practice. Radiography 26 (3), e158–e163 (2020).
Dandapani, S. V. et al. Radiation-associated toxicities in obese women with endometrial cancer: more than just BMI? ScientificWorldJournal 2015, 483208 (2015).
Hu, J. J. et al. Association between inflammatory biomarker C-reactive protein and radiotherapy-induced early adverse skin reactions in a multiracial/ethnic breast cancer population. J. Clin. Oncol. 36 (24), 2473–2482 (2018).
McCall, N. S. et al. Onco-metabolism: defining the prognostic significance of obesity and diabetes in women with brain metastases from breast cancer. Breast Cancer Res. Treat. 172 (1), 221–230 (2018).
Sabol, R. A. et al. Obesity-altered adipose stem cells promote radiation resistance of estrogen receptor positive breast cancer through paracrine signaling. Int. J. Mol. Sci. 21, 2722 (2020).
Mongan, A. M. et al. Visceral adipose tissue modulates radiosensitivity in oesophageal adenocarcinoma. Int. J. Med. Sci. 16 (4), 519–528 (2019).
Hicks, D. F. et al. Impact of obesity on outcomes for patients with head and neck cancer. Oral. Oncol. 83, 11–17 (2018).
Garland, M. et al. The impact of obesity on outcomes for patients undergoing mastectomy using the ACS-NSQIP data set. Breast Cancer Res. Treat. 168 (3), 723–726 (2018).
Zhou, C. J. et al. Metabolic syndrome, as defined based on parameters including visceral fat area, predicts complications after surgery for rectal cancer. Obes. Surg. 30 (1), 319–326 (2020).
Bouwman, F. et al. The impact of BMI on surgical complications and outcomes in endometrial cancer surgery – an institutional study and systematic review of the literature. Gynecol. Oncol. 139 (2), 369–376 (2015).
Nakauchi, M. et al. Association of obesity with worse operative and oncologic outcomes for patients undergoing gastric cancer resection. Ann. Surg. Oncol. 28 (12), 7040–7050 (2021).
Kamiya, H. et al. Obesity paradox as a new insight from postoperative complications in gastric cancer. Sci. Rep. 13 (1), 10116 (2023).
Bajawi, M. et al. Impact of CT-measured sarcopenic obesity on postoperative outcomes following colon cancer surgery. Langenbecks Arch. Surg. 409 (1), 42 (2024).
Juez, L. D. et al. Impact of sarcopenic obesity on long-term cancer outcomes and postoperative complications after gastrectomy for gastric cancer. J. Gastrointest. Surg. 27 (1), 35–46 (2023).
Wang et al. Sarcopenic obesity and therapeutic outcomes in gastrointestinal surgical oncology: a meta-analysis. Front. Nutr. 9, 921817 (2022).
Malone, E. R. et al. Molecular profiling for precision cancer therapies. Genome Med. 12 (1), 8 (2020).
Chatelut, E. et al. Unraveling the complexity of therapeutic drug monitoring for monoclonal antibody therapies to individualize dose in oncology. Pharm. Res. Perspect. 9 (2), e00757 (2021).
Erstad, B. L. & Davis, L. E. Fixed versus body-sized-based dosing of monoclonal antibodies. Ann. Pharmacother. 58 (1), 91–95 (2024).
Krasniqi, E. et al. Impact of BMI on HER2+ metastatic breast cancer patients treated with pertuzumab and/or trastuzumab emtansine. Real-world evidence. J. Cell Physiol. 235 (11), 7900–7910 (2020).
Guenancia, C. et al. Obesity as a risk factor for anthracyclines and trastuzumab cardiotoxicity in breast cancer: a systematic review and meta-analysis. J. Clin. Oncol. 34 (26), 3157–3165 (2016).
O’Sullivan, J. et al. Obesity and gastrointestinal cancer: the interrelationship of adipose and tumour microenvironments. Nat. Rev. Gastroenterol. Hepatol. 15 (11), 699–714 (2018).
Slaughter, K. N. et al. Measurements of adiposity as clinical biomarkers for first-line bevacizumab-based chemotherapy in epithelial ovarian cancer. Gynecol. Oncol. 133 (1), 11–15 (2014).
Guiu, B. et al. Visceral fat area is an independent predictive biomarker of outcome after first-line bevacizumab-based treatment in metastatic colorectal cancer. Gut 59 (3), 341–347 (2010). This study in 120 patients with metastatic colorectal cancer who had received bevacizumab showed that higher visceral adipose tissue area is associated with time to progression and poor overall survival.
Cybulska-Stopa, B. et al. Overweight is associated with better prognosis in metastatic colorectal cancer patients treated with bevacizumab plus FOLFOX chemotherapy. Contemp. Oncol. 24 (1), 34–41 (2020).
Goetz, M. et al. MONARCH 3: abemaciclib as initial therapy for advanced breast cancer. J. Clin. Oncol. 35 (32), 3638–3646 (2017).
Franzoi, M. A. et al. Computed tomography-based analyses of baseline body composition parameters and changes in breast cancer patients under treatment with CDK 4/6 inhibitors. Breast Cancer Res. Treat. 181 (1), 199–209 (2020).
Pfeiler, G. et al. Impact of BMI in patients with early hormone receptor-positive breast cancer receiving endocrine therapy with or without palbociclib in the PALLAS trial. J. Clin. Oncol. 41, 5118–5130 (2023).
Franzoi, M. A. et al. Clinical implications of body mass index in metastatic breast cancer patients treated with abemaciclib and endocrine therapy. J. Natl Cancer Inst. 113 (4), 462–470 (2021).
Hanker, A. B., Sudhan, D. R. & Arteaga, C. L. Overcoming endocrine resistance in breast cancer. Cancer Cell 37 (4), 496–513 (2020).
Ewertz, M. et al. Effect of obesity on prognosis after early-stage breast cancer. J. Clin. Oncol. 29 (1), 25–31 (2011).
Fedele et al. BMI variation increases recurrence risk in women with early-stage breast cancer. Future Oncol. 10 (15), 2459–2468 (2014).
Barone, I. et al. Obesity and endocrine therapy resistance in breast cancer: mechanistic insights and perspectives. Obes. Rev. 23 (2), e13358 (2022).
Chetta & Zadra, G. Metabolic reprogramming as an emerging mechanism of resistance to endocrine therapies in prostate cancer. Cancer Drug Resist. 4 (1), 143–162 (2021).
Stoykova, G. E. & Schlaepfer, I. R. Lipid Metabolism and endocrine resistance in prostate cancer, and new opportunities for therapy. Int. J. Mol. Sci. 20, 2626 (2019).
Labbe, D. et al. High-fat diet fuels prostate cancer progression by rewiring the metabolome and amplifying the MYC program. Nat. Commun. 10 (1), 4358 (2019).
Vidal, A. C. et al. Obese patients with castration-resistant prostate cancer may be at a lower risk of all-cause mortality: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) database. BJU Int. 122 (1), 76–82 (2018).
Bernstein, L. et al. Tamoxifen therapy for breast cancer and endometrial cancer risk. J. Natl Cancer Inst. 91 (19), 1654–1662 (1999).
Sharma et al. Immune checkpoint therapy – current perspectives and future directions. Cell 186 (8), 1652–1669 (2023).
Cortellini, A. et al. A multicenter study of body mass index in cancer patients treated with anti-PD-1/PD-L1 immune checkpoint inhibitors: when overweight becomes favorable. J. Immunother. Cancer 7 (1), 57 (2019).
Yoo, S. K. et al. Outcomes among patients with or without obesity and with cancer following treatment with immune checkpoint blockade. JAMA Netw. Open 5 (2), e220448 (2022).
Kichenadasse, G. et al. Association between body mass index and overall survival with immune checkpoint inhibitor therapy for advanced non-small cell lung cancer. JAMA Oncol. 6 (4), 512–518 (2020).
An, Y. et al. Association between body mass index and survival outcomes for cancer patients treated with immune checkpoint inhibitors: a systematic review and meta-analysis. J. Transl. Med. 18 (1), 235 (2020).
Ahmed, M. et al. Association between body mass index, dosing strategy, and efficacy of immune checkpoint inhibitors. J. Immunother. Cancer 9, e002349 (2021). A study in 297 patients suggests that patients with a BMI >25 kg/m2 show improved progression-free survival if weight-based dosing, rather than fixed dosing, is used for immune checkpoint inhibitor treatment.
Xu, H. et al. The prognostic role of obesity is independent of sex in cancer patients treated with immune checkpoint inhibitors: a pooled analysis of 4090 cancer patients. Int. Immunopharmacol. 74, 105745 (2019).
Trinkner et al. Survival and immunotoxicities in association with sex-specific body composition patterns of cancer patients undergoing immune-checkpoint inhibitor therapy – a systematic review and meta-analysis. Eur. J. Cancer 184, 151–171 (2023).
Roccuzzo, G. et al. Obesity and immune-checkpoint inhibitors in advanced melanoma: a meta-analysis of survival outcomes from clinical studies. Semin Cancer Biol. 91, 27–34 (2023).
Guzman-Prado, Y., Ben Shimol, J. & Samson, O. Body mass index and immune-related adverse events in patients on immune checkpoint inhibitor therapies: a systematic review and meta-analysis. Cancer Immunol. Immunother. 70 (1), 89–100 (2021).
Pollack, R. et al. Immune checkpoint inhibitor-induced thyroid dysfunction is associated with higher body mass index. J. Clin. Endocrinol. Metab. 105, dgaa458 (2020).
McQuade, J. L. et al. Association of body mass index with the safety profile of nivolumab with or without ipilimumab. JAMA Oncol. 9 (1), 102–111 (2023).
Zhang, D. et al. Association between body mass index and immune-related adverse events (irAEs) among advanced-stage cancer patients receiving immune checkpoint inhibitors: a pan-cancer analysis. Cancers 13, 6109 (2021).
Ged, Y. et al. Associations between pretreatment body composition features and clinical outcomes among patients with metastatic clear cell renal cell carcinoma treated with immune checkpoint blockade. Clin. Cancer Res. 28, 5180–5189 (2022).
Daly, L. E. et al. The impact of body composition parameters on ipilimumab toxicity and survival in patients with metastatic melanoma. Br. J. Cancer 116 (3), 310–317 (2017).
Heidelberger, V. et al. Sarcopenic overweight is associated with early acute limiting toxicity of anti-PD1 checkpoint inhibitors in melanoma patients. Invest N. Drugs 35 (4), 436–441 (2017).
Hirsch, L. et al. The impact of body composition parameters on severe toxicity of nivolumab. Eur. J. Cancer 124, 170–177 (2020).
Crombe, A. et al. Impact of CT-based body composition parameters at baseline, their early changes and response in metastatic cancer patients treated with immune checkpoint inhibitors. Eur. J. Radiol. 133, 109340 (2020).
Kim, L. H. et al. A systematic review and meta-analysis of the significance of body mass index on kidney cancer outcomes. J. Urol. 205 (2), 346–355 (2021).
Shahjehan, F. et al. Body mass index and long-term outcomes in patients with colorectal cancer. Front. Oncol. 8, 620 (2018).
Simkens, L. H. et al. Influence of body mass index on outcome in advanced colorectal cancer patients receiving chemotherapy with or without targeted therapy. Eur. J. Cancer 47 (17), 2560–2567 (2011). This study showed that BMI is an independent prognostic factor for better overall survival in patients with advanced colorectal cancer receiving chemotherapy (CAIRO trial); however, no significant association between BMI and overall survival was seen in patients receiving chemotherapy plus targeted therapy in the follow-up study (CAIRO2).
Caan, B. J., Cespedes Feliciano, E. M. & Kroenke, C. H. The importance of body composition in explaining the overweight paradox in cancer-counterpoint. Cancer Res. 78 (8), 1906–1912 (2018).
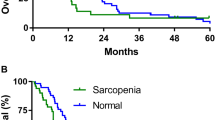
Gao, Q. et al. Prevalence and prognostic value of sarcopenic obesity in patients with cancer: a systematic review and meta-analysis. Nutrition 101, 111704 (2022).
Vecchie, A. et al. Obesity phenotypes and their paradoxical association with cardiovascular diseases. Eur. J. Intern. Med. 48, 6–17 (2018).
Winn, M. et al. Metabolic obesity phenotypes and obesity-related cancer risk in the National Health and Nutrition Examination Survey. Endocrinol. Diabetes Metab. 6 (4), e433 (2023).
Bluher, M. Metabolically healthy obesity. Endocr. Rev. 41, bnaa004 (2020).
Agius, R., Pace, N. & Fava, S. Phenotyping obesity: a focus on metabolically healthy obesity and metabolically unhealthy normal weight. Diabetes Metab. Res. Rev. 40 (2), e3725 (2024).
Zheng, X. et al. The association between metabolic status and risk of cancer among patients with obesity: metabolically healthy obesity vs. metabolically unhealthy obesity. Front. Nutr. 9, 783660 (2022).
Cespedes Feliciano, E. M., Kroenke, C. H. & Caan, B. J. The obesity paradox in cancer: how important is muscle? Annu. Rev. Nutr. 38, 357–379 (2018).
Plurphanswat, N. & Rodu, B. The association of smoking and demographic characteristics on body mass index and obesity among adults in the U.S., 1999-2012. BMC Obes. 1, 18 (2014).
Chao, A. M. et al. Tobacco smoking, eating behaviors, and body weight: a review. Curr. Addict. Rep. 6, 191–199 (2019).
Ezzatvar, Y. et al. Cardiorespiratory fitness and all-cause mortality in adults diagnosed with cancer systematic review and meta-analysis. Scand. J. Med. Sci. Sports 31 (9), 1745–1752 (2021).
Schmid, D. & Leitzmann, M. F. Cardiorespiratory fitness as predictor of cancer mortality: a systematic review and meta-analysis. Ann. Oncol. 26 (2), 272–278 (2015).
Kearney, N. et al. Feasibility metrics of exercise interventions during chemotherapy: a systematic review. Crit. Rev. Oncol. Hematol. 195, 104272 (2024).
Yang, L., Alice, A. & Friedenreich, C. M. Physical activity for cancer prehabilitation: a scoping review. Crit. Rev. Oncol. Hematol. 196, 104319 (2024).
Yang, L. et al. Effects of exercise on cancer treatment efficacy: a systematic review of preclinical and clinical studies. Cancer Res. 81 (19), 4889–4895 (2021).
Bullard, T. et al. A systematic review and meta-analysis of adherence to physical activity interventions among three chronic conditions: cancer, cardiovascular disease, and diabetes. BMC Public Health 19 (1), 636 (2019).
Shachar, S. S. et al. Prognostic value of sarcopenia in adults with solid tumours: a meta-analysis and systematic review. Eur. J. Cancer 57, 58–67 (2016).
Severinsen, M. C. K. & Pedersen, B. K. Muscle-organ crosstalk: the emerging roles of myokines. Endocr. Rev. 41 (4), 594–609 (2020).
Garneau, L. & Aguer, C. Role of myokines in the development of skeletal muscle insulin resistance and related metabolic defects in type 2 diabetes. Diabetes Metab. 45 (6), 505–516 (2019).
Rier, H. N. et al. The prevalence and prognostic value of low muscle mass in cancer patients: a review of the literature. Oncologist 21 (11), 1396–1409 (2016).
Martin, L. et al. Diagnostic criteria for the classification of cancer-associated weight loss. J. Clin. Oncol. 33 (1), 90–99 (2015).
Mayoral, L. et al. Obesity subtypes, related biomarkers & heterogeneity. Indian J. Med. Res. 151 (1), 11–21 (2020).
Kim, J., Han, S. H. & Kim, H. I. Detection of sarcopenic obesity and prediction of long-term survival in patients with gastric cancer using preoperative computed tomography and machine learning. J. Surg. Oncol. 124 (8), 1347–1355 (2021).
Donini, L. M. et al. Obesity or BMI paradox? Beneath the tip of the iceberg. Front. Nutr. 7, 53 (2020).
Muscaritoli, M., Molfino, A. & Rossi Fanelli, F. Muscle depletion and the prediction of chemotherapy toxicity. Intern Emerg. Med. 8 (5), 373–375 (2013).
Ryan, A. M. et al. Effects of weight loss and sarcopenia on response to chemotherapy, quality of life, and survival. Nutrition 67–68, 110539 (2019). This review shows that low muscle mass and poor muscle quality in patients with cancer are associated with low tolerance of chemotherapy, low quality of life, high risk of postoperative complications and poor survival.
Prado, C. M. et al. Sarcopenia as a determinant of chemotherapy toxicity and time to tumor progression in metastatic breast cancer patients receiving capecitabine treatment. Clin. Cancer Res. 15 (8), 2920–2926 (2009).
Ataseven, B. et al. Skeletal muscle attenuation (sarcopenia) predicts reduced overall survival in patients with advanced epithelial ovarian cancer undergoing primary debulking surgery. Ann. Surg. Oncol. 25 (11), 3372–3379 (2018).
Rier, H. N. et al. Low muscle attenuation is a prognostic factor for survival in metastatic breast cancer patients treated with first line palliative chemotherapy. Breast 31, 9–15 (2017).
Akahori, T. et al. Prognostic significance of muscle attenuation in pancreatic cancer patients treated with neoadjuvant chemoradiotherapy. World J. Surg. 39 (12), 2975–2982 (2015).
Berkel, A. E. M. et al. Patient’s skeletal muscle radiation attenuation and sarcopenic obesity are associated with postoperative morbidity after neoadjuvant chemoradiation and resection for rectal cancer. Dig. Surg. 36 (5), 376–383 (2019).
Sanda, M. G. et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N. Engl. J. Med. 358 (12), 1250–1261 (2008).
Jansen, L. et al. Quality of life among long-term (≥5 years) colorectal cancer survivors – systematic review. Eur. J. Cancer 46 (16), 2879–2888 (2010).
Zamboni, W. C. et al. Effect of obesity on the pharmacokinetics and pharmacodynamics of anticancer agents. J. Clin. Pharmacol. 63(S2), S85–S102 (2023).
Kenkhuis, M. F. et al. Increases in adipose tissue and muscle function are longitudinally associated with better quality of life in colorectal cancer survivors. Sci. Rep. 11 (1), 12440 (2021).
Tyrovolas, S. et al. Factors associated with skeletal muscle mass, sarcopenia, and sarcopenic obesity in older adults: a multi-continent study. J. Cachexia Sarcopenia Muscle 7 (3), 312–321 (2016).
Renehan, A. G., Alam, N. N. & Sperrin, M. Interaction between co-morbidities and cancer survival. Eur. J. Epidemiol. 34 (11), 1103–1105 (2019).
Atkins, J. L. & Wannamathee, S. G. Sarcopenic obesity in ageing: cardiovascular outcomes and mortality. Br. J. Nutr. 124 (10), 1102–1113 (2020).
Jurdana, M. & Cemazar, M. Sarcopenic obesity in cancer. Radiol. Oncol. 58 (1), 1–8 (2024).
Purcell, S. A. et al. Pharmacokinetics of cancer therapeutics and energy balance: the role of diet intake, energy expenditure, and body composition. J. Natl Cancer Inst. Monogr. 2023 (61), 3–11 (2023).
Ulrich, C. M. et al. Energy balance and gastrointestinal cancer: risk, interventions, outcomes and mechanisms. Nat. Rev. Gastroenterol. Hepatol. 15 (11), 683–698 (2018).
Castro-Espin, C. & Agudo, A. The role of diet in prognosis among cancer survivors: a systematic review and meta-analysis of dietary patterns and diet interventions. Nutrients 14, 348 (2022). This review shows that higher adherence to a Mediterranean diet is associated with better survival in patients with prostate and colorectal cancer, and higher diet quality is associated with reduced mortality in patients with breast cancer.
Laviano, A. et al. Safety and tolerability of targeted medical nutrition for cachexia in non-small-cell lung cancer: a randomized, double-blind, controlled pilot trial. Nutr. Cancer 72 (3), 439–450 (2020).
Curtis, A. R. et al. Associations between dietary patterns and malnutrition, low muscle mass and sarcopenia in adults with cancer: a scoping review. Int. J. Environ. Res. Public Health 19, 1769 (2022).
Kiss, N. & Curtis, A. Current insights in nutrition assessment and intervention for malnutrition or muscle loss in people with lung cancer: a narrative review. Adv. Nutr. 13 (6), 2420–2432 (2022).
Carayol, M. et al. Short- and long-term impact of adapted physical activity and diet counseling during adjuvant breast cancer therapy: the “APAD1” randomized controlled trial. BMC Cancer 19 (1), 737 (2019).
Sandhya, L. et al. Randomized double-blind placebo-controlled study of olanzapine for chemotherapy-related anorexia in patients with locally advanced or metastatic gastric, hepatopancreaticobiliary, and lung cancer. J. Clin. Oncol. 41 (14), 2617–2627 (2023).
Aminian, A. et al. Association of bariatric surgery with cancer risk and mortality in adults with obesity. JAMA 327 (24), 2423–2433 (2022).
Schauer, D. et al. Bariatric surgery and the risk of cancer in a large multisite cohort. Ann. Surg. 269 (1), 95–101 (2019).
Sjöström, L. et al. Effects of bariatric surgery on cancer incidence in obese patients in Sweden (Swedish Obese Subjects Study): a prospective, controlled intervention trial. Lancet Oncol. 10 (7), 653–662 (2009).
Jones-Corneille, L. R. et al. Axis I psychopathology in bariatric surgery candidates with and without binge eating disorder: results of structured clinical interviews. Obes. Surg. 22 (3), 389–397 (2012).
Kalarchian, M. A. et al. Psychiatric disorders among bariatric surgery candidates: relationship to obesity and functional health status. Am. J. Psychiatry 164 (2), 328–334 (2007). quiz 374.
Mitchell, J. E. et al. Psychopathology before surgery in the longitudinal assessment of bariatric surgery-3 (LABS-3) psychosocial study. Surg. Obes. Relat. Dis. 8 (5), 533–541 (2012).
Rosenberger, H., Henderson, K. E. & Grilo, C. M. Correlates of body image dissatisfaction in extremely obese female bariatric surgery candidates. Obes. Surg. 16 (10), 1331–1336 (2006).
Carpenter, K. M. et al. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am. J. Public Health 90 (2), 251–257 (2000).
Herpertz, S. et al. Does obesity surgery improve psychosocial functioning? A systematic review. Int. J. Obes. 27 (11), 1300–1314 (2003).
Rosengren, A. et al. Psychosocial factors and obesity in 17 high-, middle- and low-income countries: the Prospective Urban Rural Epidemiologic study. Int. J. Obes. 39 (8), 1217–1223 (2015).
Gomez, D. et al. Impact of obesity on quality of life, psychological distress, and coping on patients with colon cancer. Oncologist 26 (5), e874–e882 (2021).
Franck, J. E. et al. The determinants of cervical cancer screening uptake in women with obesity: application of the Andersen’s behavioral model to the CONSTANCES survey. Cancer Causes Control. 31 (1), 51–62 (2020).
Leone, L. A. et al. Race moderates the relationship between obesity and colorectal cancer screening in women. Cancer Causes Control. 21 (3), 373–385 (2010).
Messina, C. R., Lane, D. S. & Anderson, J. C. Body mass index and screening for colorectal cancer: gender and attitudinal factors. Cancer Epidemiol. 36 (4), 400–408 (2012).
Tekkel, M., Veideman, T. & Rahu, M. Use of mammography, Pap test and prostate examination by body mass index during the developmental period of cancer screening in Estonia. Public Health 125 (10), 697–703 (2011).
Hashemi, S. M. et al. Prevalence of anxiety among breast cancer patients: a systematic review and meta-analysis. Breast Cancer 27 (2), 166–178 (2020).
Faller, H. et al. Symptoms of depression and anxiety as predictors of physical functioning in breast cancer patients. A prospective study using path analysis. Acta Oncol. 56 (12), 1677–1681 (2017).
Seibert, R. G. et al. National disparities in colorectal cancer screening among obese adults. Am. J. Prev. Med. 53 (2), e41–e49 (2017). This study revealed that men with obesity are less likely to adhere to colorectal cancer screening guidelines than men with normal BMI, while significantly more women with obesity, compared with those without obesity, indicate pain and embarrassment as reasons for non-adherence.
Phelan, S. M. et al. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes. Rev. 16 (4), 319–326 (2015).
Nutter, S. et al. Changing the global obesity narrative to recognize and reduce weight stigma: a position statement from the World Obesity Federation. Obes. Rev. 25, e13642 (2023).
Dyck, L. et al. Suppressive effects of the obese tumor microenvironment on CD8 T cell infiltration and effector function. J. Exp. Med. 219, e20210042 (2022).
O’Neill, L. M. et al. The RESTORE randomized controlled trial: impact of a multidisciplinary rehabilitative program on cardiorespiratory fitness in esophagogastric cancer survivorship. Ann. Surg. 268 (5), 747–755 (2018).
Dickinson, H. et al. The effect of weight in the outcomes of meningioma patients. Surg. Neurol. Int. 4, 45 (2013).
Cao, J. et al. Potential impact of body mass index on the clinical outcome of papillary thyroid cancer after high-dose radioactive iodine therapy. Front. Endocrinol. 13, 870530 (2022).
Dieringer et al. Associations between body mass and papillary thyroid cancer stage and tumor size: a population-based study. J. Cancer Res. Clin. Oncol. 141 (1), 93–98 (2015).
Kim, H. J. et al. Associations between body mass index and clinico-pathological characteristics of papillary thyroid cancer. Clin. Endocrinol. 78 (1), 134–140 (2013).
Incio, J. et al. Obesity-induced inflammation and desmoplasia promote pancreatic cancer progression and resistance to chemotherapy. Cancer Discov. 6 (8), 852–869 (2016).
Liu, X. & Xu, J. Body mass index and waistline are predictors of survival for hepatocellular carcinoma after hepatectomy. Med. Sci. Monit. 21, 2203–2209 (2015).
Mathur, A. et al. Obesity portends increased morbidity and earlier recurrence following liver transplantation for hepatocellular carcinoma. HPB 15 (7), 504–510 (2013).
Ochiai, M. et al. Unlocking drug resistance in multiple myeloma: adipocytes as modulators of treatment response. Cancers 15, 4347 (2023).
Ren, L. et al. The obesity paradox in multiple myeloma: a report from Multiple Myeloma Research Foundation (MMRF) dataset. Cancer Med. 12 (23), 21400–21407 (2023).
Bracht, J. R. et al. The role of estrogens in the adipose tissue milieu. Ann. N. Y. Acad. Sci. 1461 (1), 127–143 (2020).
He, Y. et al. Cancer-specific survival after diagnosis in men versus women: a pan-cancer analysis. MedComm 3 (3), e145 (2022).
Lopez et al. Associations of fat and muscle mass with overall survival in men with prostate cancer: a systematic review with meta-analysis. Prostate Cancer Prostatic Dis. 25 (4), 615–626 (2022).
Ferrante, J. M. et al. Family physicians’ barriers to cancer screening in extremely obese patients. Obesity 18 (6), 1153–1159 (2010).
Franck, J. E. et al. Patterns of gynaecological check-up and their association with body mass index within the CONSTANCES cohort. J. Med. Screen 28 (1), 10–17 (2021).
Hellmann, S. S. et al. Body mass index and participation in organized mammographic screening: a prospective cohort study. BMC Cancer 15, 294 (2015). This Danish study revealed that postmenopausal women with underweight or class II or III obesity are significantly less likely to participate in mammographic screening than postmenopausal women with normal weight.
Clarke, M. A. et al. Epidemiologic evidence that excess body weight increases risk of cervical cancer by decreased detection of precancer. J. Clin. Oncol. 36 (12), 1184–1191 (2018).
Vazquez, C. E. & Cubbin, C. Socioeconomic status and childhood obesity: a review of literature from the past decade to inform intervention research. Curr. Obes. Rep. 9 (4), 562–570 (2020).
Hastert, T. A. et al. Contribution of health behaviors to the association between area-level socioeconomic status and cancer mortality. Soc. Sci. Med. 148, 52–58 (2016).
Cheng, I. et al. Contribution of the neighborhood environment and obesity to breast cancer survival: the California Breast Cancer Survivorship Consortium. Cancer Epidemiol. Biomark. Prev. 24 (8), 1282–1290 (2015).
Drewnowski, A., & Specter, S. E. Poverty and obesity: the role of energy density and energy costs. Am. J. Clin. Nutr. 79 (1), 6–16 (2004).
Akinyemiju, T. et al. Life-course socioeconomic status and breast and cervical cancer screening: analysis of the WHO’s Study on Global Ageing and Adult Health (SAGE). BMJ Open 6 (11), e012753 (2016).
Bozhar, H. et al. Socio-economic inequality of utilization of cancer testing in Europe: a cross-sectional study. Prev. Med. Rep. 26, 101733 (2022).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Endocrinology thanks the anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
American Cancer Society: www.cancer.org
Physical activity: www.who.int/news-room/fact-sheets/detail/physical-activity
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lysaght, J., Conroy, M.J. The multifactorial effect of obesity on the effectiveness and outcomes of cancer therapies. Nat Rev Endocrinol (2024). https://doi.org/10.1038/s41574-024-01032-5
Accepted:
Published:
DOI: https://doi.org/10.1038/s41574-024-01032-5