Abstract
In the 2022 fifth edition of the WHO Classification of Endocrine Tumours and of Central Nervous System Tumours, pituitary adenomas are reclassified as neuroendocrine tumours (NETs). This change confers an oncology label to neoplasms that are overwhelmingly benign. A comprehensive clinical classification schema is required to guide prognosis, therapy and outcomes for all patients with pituitary adenomas. Pituitary adenomas and NETs exhibit some morphological and ultrastructural similarities. However, unlike NETs, pituitary adenomas are highly prevalent, yet indolent and rarely become malignant. This Perspective presents the outcomes of an interdisciplinary international workshop that addressed the merit and clinical implications of the classification change of pituitary adenoma to NET. Many non-histological factors provide mechanistic insight and influence the prognosis and treatment of pituitary adenoma. We recommend the development of a comprehensive classification that integrates clinical, genetic, biochemical, radiological, pathological and molecular information for all anterior pituitary neoplasms.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Melmed, S. et al. Clinical biology of the pituitary adenoma. Endocr. Rev. 43, 1003–1037 (2022).
Asa, S. L., Mete, O., Perry, A. & Osamura, R. Y. Overview of the 2022 WHO classification of pituitary tumors. Endocr. Pathol. 33, 6–26 (2022).
Ho, K. K. Y. et al. A tale of pituitary adenomas: to NET or not to NET: pituitary society position statement. Pituitary 22, 569–573 (2019).
Jutel, A. Classification, disease, and diagnosis. Perspect. Biol. Med. 54, 189–205 (2011).
Doust, J. A., Bell, K. J. L. & Glasziou, P. P. Potential consequences of changing disease classifications. JAMA 323, 921–922 (2020).
Ho, K. et al. Pituitary neoplasm nomenclature workshop: does adenoma stand the test of time? J. Endocr. Soc. 5, bvaa205 (2021).
Ho, K. K. Y., Gadelha, M., Kaiser, U. B., Reincke, M. & Melmed, S. The NETting of pituitary adenoma: a gland illusion. Pituitary 25, 349–351 (2022).
Liu, X., Wang, R., Li, M. & Chen, G. Pituitary adenoma or pituitary neuroendocrine tumor: a narrative review of controversy and perspective. Transl. Cancer Res. 10, 1916–1920 (2021).
Doust, J. et al. Guidance for modifying the definition of diseases: a checklist. JAMA Intern. Med. 177, 1020–1025 (2017).
Asa, S. L. et al. From pituitary adenoma to pituitary neuroendocrine tumor (PitNET): an international pituitary pathology club proposal. Endocr. Relat. Cancer 24, C5–C8 (2017).
Fernandez, A., Karavitaki, N. & Wass, J. A. Prevalence of pituitary adenomas: a community-based, cross-sectional study in Banbury (Oxfordshire, UK). Clin. Endocrinol. 72, 377–382 (2010).
Daly, A. F. et al. High prevalence of pituitary adenomas: a cross-sectional study in the province of Liege, Belgium. J. Clin. Endocrinol. Metab. 91, 4769–4775 (2006).
Agustsson, T. T. et al. The epidemiology of pituitary adenomas in Iceland, 1955-2012: a nationwide population-based study. Eur. J. Endocrinol. 173, 655–664 (2015).
Graffeo, C. S. et al. Pituitary adenoma incidence, management trends, and long-term outcomes: a 30-year population-based analysis. Mayo Clin. Proc. 97, 1861–1871 (2022).
Dekkers, O. M., Karavitaki, N. & Pereira, A. M. The epidemiology of aggressive pituitary tumors (and its challenges). Rev. Endocr. Metab. Disord. 21, 209–212 (2020).
Han, A. J., Varlamov, E. V. & Fleseriu, M. Nonfunctioning pituitary microadenomas: should imaging interval be extended? A large single-center cohort study. J. Clin. Endocrinol. Metab. 107, e1231–e1241 (2022).
Karavitaki, N. et al. What is the natural history of nonoperated nonfunctioning pituitary adenomas? Clin. Endocrinol. 67, 938–943 (2007).
Lenders, N. et al. Longitudinal evaluation of the natural history of conservatively managed nonfunctioning pituitary adenomas. Clin. Endocrinol. 84, 222–228 (2016).
Raverot, G. et al. European society of endocrinology clinical practice guidelines for the management of aggressive pituitary tumours and carcinomas. Eur. J. Endocrinol. 178, G1–G24 (2018).
Molitch, M. E. Diagnosis and treatment of pituitary adenomas: a review. JAMA 317, 516–524 (2017).
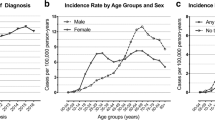
White, B. E. et al. Incidence and survival of neuroendocrine neoplasia in England 1995-2018: a retrospective, population-based study. Lancet Reg. Health Eur. 23, 100510 (2022).
Hallet, J. et al. Exploring the rising incidence of neuroendocrine tumors: a population-based analysis of epidemiology, metastatic presentation, and outcomes. Cancer 121, 589–597 (2015).
Eriksson, J. et al. Primary small intestinal neuroendocrine tumors are highly prevalent and often multiple before metastatic disease develops. Scand. J. Surg. 110, 44–50 (2021).
Chen, C. et al. Incidence, demographics, and survival of patients with primary pituitary tumors: a SEER database study in 2004-2016. Sci. Rep. 11, 15155 (2021).
Raphael, M. J., Chan, D. L., Law, C. & Singh, S. Principles of diagnosis and management of neuroendocrine tumours. CMAJ 189, E398–E404 (2017).
Pape, U. F. et al. ENETS consensus guidelines for neuroendocrine neoplasms of the appendix (excluding goblet cell carcinomas). Neuroendocrinology 103, 144–152 (2016).
Dasari, A. et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 3, 1335–1342 (2017).
Schonhoff, S. E., Giel-Moloney, M. & Leiter, A. B. Neurogenin 3-expressing progenitor cells in the gastrointestinal tract differentiate into both endocrine and non-endocrine cell types. Dev. Biol. 270, 443–454 (2004).
Jenny, M. et al. Neurogenin3 is differentially required for endocrine cell fate specification in the intestinal and gastric epithelium. EMBO J. 21, 6338–6347 (2002).
Gradwohl, G., Dierich, A., LeMeur, M. & Guillemot, F. neurogenin3 is required for the development of the four endocrine cell lineages of the pancreas. Proc. Natl Acad. Sci. USA 97, 1607–1611 (2000).
Ando, M. et al. The proneural bHLH genes Mash1, Math3 and NeuroD are required for pituitary development. J. Mol. Endocrinol. 61, 127–138 (2018).
Davis, S. W. et al. Molecular mechanisms of pituitary organogenesis: in search of novel regulatory genes. Mol. Cell Endocrinol. 323, 4–19 (2010).
Fang, Q. et al. Genetics of combined pituitary hormone deficiency: roadmap into the genome era. Endocr. Rev. 37, 636–675 (2016).
Rindi, G. et al. A common classification framework for neuroendocrine neoplasms: an International Agency for Research on Cancer (IARC) and World Health Organization (WHO) expert consensus proposal. Mod. Pathol. 31, 1770–1786 (2018).
Brown, M. B. & Limaiem, F. Histology, parathyroid gland. StatPearls https://www.ncbi.nlm.nih.gov/books/NBK546596/ (2022).
Rindi, G. et al. Overview of the 2022 WHO classification of neuroendocrine neoplasms. Endocr. Pathol. 33, 115–154 (2022).
Satoh, F., Umemura, S., Yasuda, M. & Osamura, R. Y. Neuroendocrine marker expression in thyroid epithelial tumors. Endocr. Pathol. 12, 291–299 (2001).
Haak, H. R. & Fleuren, G. J. Neuroendocrine differentiation of adrenocortical tumors. Cancer 75, 860–864 (1995).
Uhlig, R. et al. Synaptophysin and chromogranin A expression analysis in human tumors. Mol. Cell Endocrinol. 555, 111726 (2022).
Trouillas, J. et al. A new prognostic clinicopathological classification of pituitary adenomas: a multicentric case-control study of 410 patients with 8 years post-operative follow-up. Acta Neuropathol. 126, 123–135 (2013).
Knosp, E., Steiner, E., Kitz, K. & Matula, C. Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33, 610–617 (1993).
Raverot, G. et al. Risk of recurrence in pituitary neuroendocrine tumors: a prospective study using a five-tiered classification. J. Clin. Endocrinol. Metab. 102, 3368–3374 (2017).
Sahakian, N. et al. Real-life clinical impact of a five-tiered classification of pituitary tumors. Eur. J. Endocrinol. 187, 893–904 (2022).
Asioli, S. et al. Validation of a clinicopathological score for the prediction of post-surgical evolution of pituitary adenoma: retrospective analysis on 566 patients from a tertiary care centre. Eur. J. Endocrinol. 180, 127–134 (2019).
Spada, A. et al. Pituitary tumors: genetic and molecular factors underlying pathogenesis and clinical behavior. Neuroendocrinology 112, 15–33 (2022).
Wildemberg, L. E. et al. gsp mutation is not a molecular biomarker of long-term response to first-generation somatostatin receptor ligands in acromegaly. Cancers 13, 4857 (2021).
Reincke, M. et al. Mutations in the deubiquitinase gene USP8 cause Cushing’s disease. Nat. Genet. 47, 31–38 (2015).
Casar-Borota, O. et al. Corticotroph aggressive pituitary tumors and carcinomas frequently harbor ATRX mutations. J. Clin. Endocrinol. Metab. 106, 1183–1194 (2021).
Rindi, G. et al. TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Arch. 449, 395–401 (2006).
Chanson, P. & Maiter, D. The epidemiology, diagnosis and treatment of Prolactinomas: The old and the new. Best Pract. Res. Clin. Endocrinol. Metab. 33, 101290 (2019).
Fleseriu, M. et al. Consensus on diagnosis and management of Cushing’s disease: a guideline update. Lancet Diabetes Endocrinol. 9, 847–875 (2021).
Yavropoulou, M. P., Tsoli, M., Barkas, K., Kaltsas, G. & Grossman, A. The natural history and treatment of non-functioning pituitary adenomas (non-functioning PitNETs). Endocr. Relat. Cancer 27, R375–R390 (2020).
Dixon, P. R. et al. The role of disease label in patient perceptions and treatment decisions in the setting of low-risk malignant neoplasms. JAMA Oncol. 5, 817–823 (2019).
Chadha, N. K. & Repanos, C. Patients’ understanding of words used to describe lumps: a cross-sectional study. J. Laryngol. Otol. 120, 125–128 (2006).
Van den Bruel, A. The triumph of medicine: how overdiagnosis is turning healthy people into patients. Fam. Pract. 32, 127–128 (2015).
Glasziou, P. P., Jones, M. A., Pathirana, T., Barratt, A. L. & Bell, K. J. Estimating the magnitude of cancer overdiagnosis in Australia. Med. J. Aust. 212, 163–168 (2020).
Esserman, L. J. et al. Addressing overdiagnosis and overtreatment in cancer: a prescription for change. Lancet Oncol. 15, e234–e242 (2014).
Esserman, L. J. & Varma, M. Should we rename low risk cancers? BMJ 364, k4699 (2019).
Epstein, J. I. Is grade group 1 (Gleason score 3 + 3 = 6) adenocarcinoma of the prostate really cancer? Curr. Opin. Urol. 32, 91–95 (2022).
Epstein, J. I. et al. The 2019 genitourinary pathology society (GUPS) white paper on contemporary grading of prostate cancer. Arch. Pathol. Lab. Med. 145, 461–493 (2021).
Melmed, S. Pituitary-tumor endocrinopathies. N. Engl. J. Med. 382, 937–950 (2020).
Neou, M. et al. Pangenomic classification of pituitary neuroendocrine tumors. Cancer Cell 37, 123–134 e125 (2020).
Acknowledgements
The PANOMEN 2 workshop was sponsored by The Pituitary Society with no commercial support. We thank M. Beatriz S. Lopes, University of Virginia, Charlottesville, VA, USA, and Olivera Casar-Borota, Uppsala University Hospital, Uppsala, Sweden, for participating in the discussions.
Author information
Authors and Affiliations
Contributions
A.D.B., P.C., L.E., L.N., G.R., L.R., M.R., J.S. and J.W. researched data for the article. All authors contributed substantially to discussion of the content. K.H. and S.M. wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Endocrinology thanks Nienke Biermasz and Gherardo Mazziotti for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Acromegaly Community: https://acromegalycommunity.org
NETs: http://www.mayoclinic.org/syc-20354132
WHO Family of International Classifications: https://www.who.int/standards/classifications
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ho, K.K.Y., Kaiser, U.B., Chanson, P. et al. Pituitary adenoma or neuroendocrine tumour: the need for an integrated prognostic classification. Nat Rev Endocrinol 19, 671–678 (2023). https://doi.org/10.1038/s41574-023-00883-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-023-00883-8