Abstract
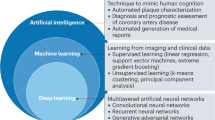
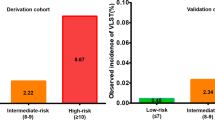
This Perspective article is a form of ‘pastiche’, inspired by the 1993 review by Lincoff and Topol entitled ‘Illusion of reperfusion’, and explores how their concept continues to apply to percutaneous revascularization in patients with coronary artery disease and ischaemia. Just as Lincoff and Topol argued that reperfusion of acute myocardial infarction was facing unresolved obstacles that hampered clinical success in 1993, we propose that challenging issues are similarly jeopardizing the potential benefits of stent-based angioplasty today. By analysing the appropriateness and efficacy of percutaneous coronary intervention (PCI), we emphasize the limitations of relying solely on visual angiographic guidance, which frequently leads to inappropriate stenting and overtreatment in up to one-third of patients and the associated increased risk of periprocedural myocardial infarction. The lack of optimal revascularization observed in half of patients undergoing PCI confers risks such as suboptimal physiology after PCI, residual angina and long-term stent-related events, leaving an estimated 76% of patients with an ‘illusion of revascularization’. These outcomes highlight the need to refine our diagnostic tools by integrating physiological assessments with targeted intracoronary imaging and emerging strategies, such as co-registration systems and angiography-based computational methods enhanced by artificial intelligence, to achieve optimal revascularization outcomes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Lincoff, A. M. & Topol, E. J. Illusion of reperfusion. Does anyone achieve optimal reperfusion during acute myocardial infarction? Circulation 88, 1361–1374 (1993).
Tonino, P. A. L. et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N. Engl. J. Med. 360, 213–224 (2009).
Layland, J. et al. Fractional flow reserve vs. angiography in guiding management to optimize outcomes in non-ST-segment elevation myocardial infarction: the British Heart Foundation FAMOUS-NSTEMI randomized trial. Eur. Heart J. 36, 100–111 (2015).
Stables, R. H. et al. Routine pressure wire assessment versus conventional angiography in the management of patients with coronary artery disease: the RIPCORD 2 trial. Circulation 146, 687–698 (2022).
Lee, J. M. et al. Fractional flow reserve versus angiography-guided strategy in acute myocardial infarction with multivessel disease: a randomized trial. Eur. Heart J. 44, 473–484 (2023).
Xu, B. et al. Angiographic quantitative flow ratio-guided coronary intervention (FAVOR III China): a multicentre, randomised, sham-controlled trial. Lancet 398, 2149–2159 (2021).
Koo, B. K. et al. Fractional flow reserve or intravascular ultrasonography to guide PCI. N. Engl. J. Med. 387, 779–789 (2022).
Di Serafino, L. et al. Long-term clinical outcome after fractional flow reserve- versus angio-guided percutaneous coronary intervention in patients with intermediate stenosis of coronary artery bypass grafts. Am. Heart J. 166, 110–118 (2013).
Wongpraparut, N. et al. Thirty-month outcome after fractional flow reserve-guided versus conventional multivessel percutaneous coronary intervention. Am. J. Cardiol. 96, 877–884 (2005).
Li, J. et al. Long-term outcomes of fractional flow reserve-guided vs. angiography-guided percutaneous coronary intervention in contemporary practice. Eur. Heart J. 34, 1375–1383 (2013).
Puymirat, E. et al. Long-term clinical outcome after fractional flow reserve-guided percutaneous coronary revascularization in patients with small-vessel disease. Circ. Cardiovasc. Interv. 5, 62–68 (2012).
Nam, C. W. et al. Outcomes of percutaneous coronary intervention in intermediate coronary artery disease: fractional flow reserve-guided versus intravascular ultrasound-guided. JACC Cardiovasc. Interv. 3, 812–817 (2010).
Burzotta, F. et al. Fractional flow reserve or optical coherence tomography to guide management of angiographically intermediate coronary stenosis: a single-center trial. JACC Cardiovasc. Interv. 13, 49–58 (2020).
Rioufol, G. et al. Fractional flow reserve to guide treatment of patients with multivessel coronary artery disease. J. Am. Coll. Cardiol. 78, 1875–1885 (2021).
Puymirat, E. et al. Multivessel PCI guided by FFR or angiography for myocardial infarction. N. Engl. J. Med. 385, 297–308 (2021).
de la Torre Hernandez, J. M. et al. Clinical outcomes after intravascular ultrasound and fractional flow reserve assessment of intermediate coronary lesions. Propensity score matching of large cohorts from two institutions with a differential approach. EuroIntervention 9, 824–830 (2013).
Banning, A. P. et al. Five-year outcomes after state-of-the-art percutaneous coronary revascularization in patients with de novo three-vessel disease: final results of the SYNTAX II study. Eur. Heart J. 43, 1307–1316 (2022).
Jeremias, A. et al. Blinded physiological assessment of residual ischemia after successful angiographic percutaneous coronary intervention: the DEFINE PCI study. JACC Cardiovasc. Interv. 12, 1991–2001 (2019).
Ahn, J. M. et al. Fractional flow reserve and cardiac events in coronary artery disease: data from a prospective IRIS-FFR registry (Interventional Cardiology Research Incooperation Society Fractional Flow Reserve). Circulation 135, 2241–2251 (2017).
Zimmermann, F. M. et al. Fractional flow reserve-guided percutaneous coronary intervention vs. medical therapy for patients with stable coronary lesions: meta-analysis of individual patient data. Eur. Heart J. 40, 180–186 (2019).
De Bruyne, B. et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N. Engl. J. Med. 367, 991–1001 (2012).
Pijls, N. H. et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study. J. Am. Coll. Cardiol. 56, 177–184 (2010).
Fezzi, S. et al. Coronary physiology in the catheterisation laboratory: an A to Z practical guide. AsiaIntervention 8, 86–109 (2022).
Metz, L. D. et al. The prognostic value of normal exercise myocardial perfusion imaging and exercise echocardiography: a meta-analysis. J. Am. Coll. Cardiol. 49, 227–237 (2007).
Pijls, N. H. & Sels, J. W. Functional measurement of coronary stenosis. J. Am. Coll. Cardiol. 59, 1045–1057 (2012).
Zimmermann, F. M. et al. Deferral vs. performance of percutaneous coronary intervention of functionally non-significant coronary stenosis: 15-year follow-up of the DEFER trial. Eur. Heart J. 36, 3182–3188 (2015).
Toth, G. et al. Evolving concepts of angiogram: fractional flow reserve discordances in 4000 coronary stenoses. Eur. Heart J. 35, 2831–2838 (2014).
Zhang, R. et al. Outcomes of quantitative flow ratio-based percutaneous coronary intervention in an all-comers study. EuroIntervention 17, 1240–1251 (2022).
Toth, G. G. et al. Revascularization decisions in patients with stable angina and intermediate lesions: results of the international survey on interventional strategy. Circ. Cardiovasc. Interv. 7, 751–759 (2014).
Toth, G. G. et al. Revascularization decisions in patients with chronic coronary syndromes: results of the second International Survey on Interventional Strategy (ISIS-2). Int. J. Cardiol. 336, 38–44 (2021).
Park, S. J. et al. Trends in the outcomes of percutaneous coronary intervention with the routine incorporation of fractional flow reserve in real practice. Eur. Heart J. 34, 3353–3361 (2013).
Ueki, Y. & Räber, L. Frequency and outcomes of periprocedural myocardial infarction in patients with chronic coronary syndromes undergoing percutaneous coronary intervention. Curr. Opin. Cardiol. 37, 488–494 (2022).
Hara, H. et al. Impact of peri-procedural myocardial infarction on outcomes after revascularization. J. Am. Coll. Cardiol. 76, 1622–1639 (2020).
Gregson, J. et al. Implications of alternative definitions of peri-procedural myocardial infarction after coronary revascularization. J. Am. Coll. Cardiol. 76, 1609–1621 (2020).
De Bruyne, B. et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N. Engl. J. Med. 371, 1208–1217 (2014).
Xaplanteris, P. et al. Five-year outcomes with PCI guided by fractional flow reserve. N. Engl. J. Med. 379, 250–259 (2018).
Spertus, J. A. et al. Health-status outcomes with invasive or conservative care in coronary disease. N. Engl. J. Med. 382, 1408–1419 (2020).
Madhavan, M. V. et al. Stent-related adverse events >1 year after percutaneous coronary intervention. J. Am. Coll. Cardiol. 75, 590–604 (2020).
Pijls, N. H. et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER study. J. Am. Coll. Cardiol. 49, 2105–2111 (2007).
Escaned, J. et al. Safety of the deferral of coronary revascularization on the basis of instantaneous wave-free ratio and fractional flow reserve measurements in stable coronary artery disease and acute coronary syndromes. JACC Cardiovasc. Interv. 11, 1437–1449 (2018).
Berntorp, K. et al. Clinical outcome of revascularization deferral with instantaneous wave-free ratio and fractional flow reserve: a 5-year follow-up substudy from the iFR-SWEDEHEART trial. J. Am. Heart Assoc. 12, e028423 (2023).
De Bruyne, B. et al. Abnormal epicardial coronary resistance in patients with diffuse atherosclerosis but “normal” coronary angiography. Circulation 104, 2401–2406 (2001).
Patel, M. R. et al. 1-Year outcomes of blinded physiological assessment of residual ischemia after successful PCI: DEFINE PCI trial. JACC Cardiovasc. Interv. 15, 52–61 (2022).
Masdjedi, K. et al. Prognostic value of post-percutaneous coronary intervention diastolic pressure ratio. Neth. Heart J. 30, 352–359 (2022).
Shin, D. et al. Prognostic implications of post-intervention resting Pd/Pa and fractional flow reserve in patients with stent implantation. JACC Cardiovasc. Interv. 13, 1920–1933 (2020).
Hakeem, A. et al. Incremental prognostic value of post-intervention Pd/Pa in patients undergoing ischemia-driven percutaneous coronary intervention. JACC Cardiovasc. Interv. 12, 2002–2014 (2019).
Ueno, H. et al. Prognostic implications of fractional flow reserve and coronary flow reserve after drug-eluting stent implantation. Circ. J. https://doi.org/10.1253/circj.CJ-23-0293 (2023).
Piroth, Z. et al. Prognostic value of measuring fractional flow reserve after percutaneous coronary intervention in patients with complex coronary artery disease: insights from the FAME 3 trial. Circ. Cardiovasc. Interv. 15, 884–891 (2022).
Hwang, D. et al. Prognostic implications of fractional flow reserve after coronary stenting: a systematic review and meta-analysis. JAMA Netw. Open 5, e2232842 (2022).
Diletti, R. et al. Impact of poststenting fractional flow reserve on long-term clinical outcomes. Circ. Cardiovasc. Interv. 14, e009681 (2021).
Hokama, Y. et al. Insufficient recovery of fractional flow reserve even after optimal implantation of drug-eluting stents: 3-year outcomes from the FUJI study. J. Cardiol. 77, 532–538 (2021).
Lee, J. M. et al. Prognostic impact of residual anatomic disease burden after functionally complete revascularization. Circ. Cardiovasc. Interv. 13, e009232 (2020).
Azzalini, L. et al. Impact of post-percutaneous coronary intervention fractional flow reserve measurement on procedural management and clinical outcomes: the REPEAT-FFR study. J. Invasive Cardiol. 31, 229–234 (2019).
Li, S. et al. Cutoff value and long-term prediction of clinical events by FFR measured immediately after implantation of a drug-eluting stent in patients with coronary artery disease: 1-to-3-year results from the DKCRUSH VII registry study. JACC Cardiovasc. Interv. 10, 986–995 (2017).
Piroth, Z. et al. Prognostic value of fractional flow reserve measured immediately after drug-eluting stent implantation. Circ. Cardiovasc. Interv. 10, e005233 (2017).
Kasula, S. et al. Clinical and prognostic value of poststenting fractional flow reserve in acute coronary syndromes. Heart 102, 1988–1994 (2016).
Agarwal, S. K. et al. Utilizing post-intervention fractional flow reserve to optimize acute results and the relationship to long-term outcomes. JACC Cardiovasc. Interv. 9, 1022–1031 (2016).
Reith, S., Battermann, S., Hellmich, M., Marx, N. & Burgmaier, M. Correlation between OCT-derived intrastent dimensions and fractional flow reserve measurements after coronary stent implantation and impact on clinical outcome. J. Invasive Cardiol. 27, 222–228 (2015).
Ito, T., Tani, T., Fujita, H. & Ohte, N. Relationship between fractional flow reserve and residual plaque volume and clinical outcomes after optimal drug-eluting stent implantation: insight from intravascular ultrasound volumetric analysis. Int. J. Cardiol. 176, 399–404 (2014).
Leesar, M. A. et al. The impact of fractional flow reserve measurement on clinical outcomes after transradial coronary stenting. EuroIntervention 7, 917–923 (2011).
Nam, C. W. et al. Relation of fractional flow reserve after drug-eluting stent implantation to one-year outcomes. Am. J. Cardiol. 107, 1763–1767 (2011).
Neleman, T. et al. The prognostic value of angiography-based vessel fractional flow reserve after percutaneous coronary intervention: the FAST outcome study. Int. J. Cardiol. 359, 14–19 (2022).
You, W. et al. Post-PCI quantitative flow ratio predicts 3-year outcome after rotational atherectomy in patients with heavily calcified lesions. Clin. Cardiol. 45, 558–566 (2022).
Dai, N. et al. Prognostic implications of prestent pullback pressure gradient and poststent quantitative flow ratio in patients undergoing percutaneous coronary intervention. J. Am. Heart Assoc. 11, e024903 (2022).
Erbay, A. et al. Prognostic impact of pancoronary quantitative flow ratio assessment in patients undergoing percutaneous coronary intervention for acute coronary syndromes. Circ. Cardiovasc. Interv. 14, e010698 (2021).
Tang, J. et al. Clinical implication of quantitative flow ratio to predict clinical events after drug-coated balloon angioplasty in patients with in-stent restenosis. Clin. Cardiol. 44, 978–986 (2021).
Liu, L. et al. Prognostic value of post-procedural μQFR for drug-coated balloons in the treatment of in-stent restenosis. Cardiol. J. 30, 167–117 (2021).
Saito, Y. et al. Long-term serial functional evaluation after implantation of the Fantom sirolimus-eluting bioresorbable coronary scaffold. Catheter. Cardiovasc. Interv. 97, 431–436 (2021).
Tang, J. et al. Clinical implication of QFR in patients with ST-segment elevation myocardial infarction after drug-eluting stent implantation. Int. J. Cardiovasc. Imaging 37, 755–766 (2021).
Kogame, N. et al. Clinical implication of quantitative flow ratio after percutaneous coronary intervention for 3-vessel disease. JACC Cardiovasc. Interv. 12, 2064–2075 (2019).
Biscaglia, S. et al. Prognostic value of QFR measured immediately after successful stent implantation: the international multicenter prospective HAWKEYE study. JACC Cardiovasc. Interv. 12, 2079–2088 (2019).
Agarwal, S. K. et al. Clinical and angiographic predictors of persistently ischemic fractional flow reserve after percutaneous revascularization. Am. Heart J. 184, 10–16 (2017).
Baranauskas, A. et al. FFR result post PCI is suboptimal in long diffuse coronary artery disease. EuroIntervention 12, 1473–1480 (2016).
Wolfrum, M., Maria, G. L. D., Benenati, S., Langrish, J. & Banning, A. P. What are the causes of a suboptimal FFR after coronary stent deployment? Insights from a consecutive series using OCT imaging. EuroIntervention 14, e1324–e1331 (2018).
van Zandvoort, L. J. C. et al. Explanation of postprocedural fractional flow reserve below 0.85: a comprehensive ultrasound analysis of the FFR SEARCH registry. Circ. Cardiovasc. Interv. 12, e007030 (2019).
Ding, D. et al. Optical flow ratio for assessing stenting result and physiological significance of residual disease. EuroIntervention 17, e989–e998 (2021).
Collison, D. et al. Post-stenting fractional flow reserve vs coronary angiography for optimization of percutaneous coronary intervention (TARGET-FFR). Eur. Heart J. 42, 4656–4668 (2021).
Collet, C. et al. Differential improvement in angina and health-related quality of life after PCI in focal and diffuse coronary artery disease. JACC Cardiovasc. Interv. 15, 2506–2518 (2022).
Stone, G. W. et al. Blinded outcomes and angina assessment of coronary bioresorbable scaffolds: 30-day and 1-year results from the ABSORB IV randomised trial. Lancet 392, 1530–1540 (2019).
Boden, W. E. et al. The evolving pattern of symptomatic coronary artery disease in the United States and Canada: baseline characteristics of the clinical outcomes utilizing revascularization and aggressive DruG evaluation (COURAGE) trial. Am. J. Cardiol. 99, 208–212 (2007).
Head, S. J. et al. Incidence, predictors and outcomes of incomplete revascularization after percutaneous coronary intervention and coronary artery bypass grafting: a subgroup analysis of 3-year SYNTAX data. Eur. J. Cardiothorac. Surg. 41, 535–541 (2012).
Arnold, S. V. et al. Prediction of residual angina after percutaneous coronary intervention. Eur. Heart J. Qual. Care Clin. Outcomes 1, 23–30 (2015).
Baron, S. J. et al. Quality-of-life after everolimus-eluting stents or bypass surgery for left-main disease: results from the EXCEL trial. J. Am. Coll. Cardiol. 70, 3113–3122 (2017).
Abdallah, M. S. et al. Quality of life after PCI vs CABG among patients with diabetes and multivessel coronary artery disease: a randomized clinical trial. JAMA 310, 1581–1590 (2013).
Collison, D. et al. Angina after percutaneous coronary intervention: patient and procedural predictors. Circ. Cardiovasc. Interv. 16, e012511 (2023).
Ono, M. et al. Impact of residual angina on long-term clinical outcomes after percutaneous coronary intervention or coronary artery bypass graft for complex coronary artery disease. Eur. Heart J. Qual. Care Clin. Outcomes 9, 490–501 (2022).
Johnson, N. P. et al. Prognostic value of fractional flow reserve: linking physiologic severity to clinical outcomes. J. Am. Coll. Cardiol. 64, 1641–1654 (2014).
Andersen, B. K. et al. Predictive value of post-percutaneous coronary intervention fractional flow reserve: a systematic review and meta-analysis. Eur. Heart J. Qual. Care Clin. Outcomes 9, 99–108 (2023).
Rajkumar, C. A. et al. A placebo-controlled trial of percutaneous coronary intervention for stable angina. N. Engl. J. Med. 389, 2319–2330 (2023).
Escaned, J. et al. Applied coronary physiology for planning and guidance of percutaneous coronary interventions. A clinical consensus statement from the European Association of Percutaneous Cardiovascular Interventions (EAPCI) of the European Society of Cardiology. EuroIntervention 19, 464–481 (2023).
Ding, D. et al. Quantitative flow ratio modulated by intracoronary optical coherence tomography for predicting physiological efficacy of percutaneous coronary intervention. Catheter. Cardiovasc. Interv. 102, 36–45 (2023).
Ding, D. et al. Immediate post-procedural functional assessment of percutaneous coronary intervention: current evidence and future directions. Eur. Heart J. 42, 2695–2707 (2021).
Tu, S. et al. Diagnostic accuracy of fast computational approaches to derive fractional flow reserve from diagnostic coronary angiography: the international multicenter FAVOR Pilot study. JACC Cardiovasc. Interv. 9, 2024–2035 (2016).
Tu, S. et al. Fractional flow reserve in clinical practice: from wire-based invasive measurement to image-based computation. Eur. Heart J. 41, 3271–3279 (2020).
Nijjer, S. S. et al. Pre-angioplasty instantaneous wave-free ratio pullback provides virtual intervention and predicts hemodynamic outcome for serial lesions and diffuse coronary artery disease. JACC Cardiovasc. Interv. 7, 1386–1396 (2014).
Kikuta, Y. et al. Pre-angioplasty instantaneous wave-free ratio pullback predicts hemodynamic outcome in humans with coronary artery disease: primary results of the international multicenter iFR GRADIENT registry. JACC Cardiovasc. Interv. 11, 757–767 (2018).
Zhang, R. et al. Post-PCI outcomes predicted by pre-intervention simulation of residual quantitative flow ratio using augmented reality. Int. J. Cardiol. 352, 33–39 (2022).
Yu, W. et al. Diagnostic accuracy of intracoronary optical coherence tomography-derived fractional flow reserve for assessment of coronary stenosis severity. EuroIntervention 15, 189–197 (2019).
Scarsini, R. et al. Functional patterns of coronary disease: diffuse, focal, and serial lesions. JACC Cardiovasc. Interv. 15, 2174–2191 (2022).
Scarsini, R. et al. Impact of physiologically diffuse versus focal pattern of coronary disease on quantitative flow reserve diagnostic accuracy. Catheter. Cardiovasc. Interv. 99, 736–745 (2022).
Dourado, L. O. C. et al. Coronary artery bypass surgery in diffuse advanced coronary artery disease: 1-year clinical and angiographic results. Thorac. Cardiovasc. Surg. 66, 477–482 (2018).
Ann, S. H., Balbir Singh, G., Lim, K. H., Koo, B.-K. & Shin, E.-S. Anatomical and physiological changes after paclitaxel-coated balloon for atherosclerotic de novo coronary lesions: serial IVUS-VH and FFR study. PLoS ONE 11, e0147057 (2016).
Ahmad, W. A. W. et al. Treatment of coronary de novo lesions by a sirolimus- or paclitaxel-coated balloon. JACC Cardiovasc. Interv. 15, 770–779 (2022).
Schaar, J. A. et al. Intravascular palpography for high-risk vulnerable plaque assessment. Herz 28, 488–495 (2003).
Bourantas, C. V. et al. Shear stress estimated by quantitative coronary angiography predicts plaques prone to progress and cause events. JACC Cardiovasc. Imaging 13, 2206–2219 (2020).
Wu, X. et al. A novel four-dimensional angiographic approach to assess dynamic superficial wall stress of coronary arteries in vivo: initial experience in evaluating vessel sites with subsequent plaque rupture. EuroIntervention 13, e1099–e1103 (2017).
Tu, S. et al. Short-term risk stratification of non-flow-limiting coronary stenosis by angiographically derived radial wall strain. J. Am. Coll. Cardiol. 81, 756–767 (2023).
Huang, J. et al. Optical coherence tomography-derived changes in plaque structural stress over the cardiac cycle: a new method for plaque biomechanical assessment. Front. Cardiovasc. Med. 8, 715995 (2021).
Wang, Z. Q. et al. Angiography-derived radial wall strain predicts coronary lesion progression in non-culprit intermediate stenosis. J. Geriatr. Cardiol. 19, 937–948 (2022).
Hong, H. et al. Radial wall strain: a novel angiographic measure of plaque composition and vulnerability. EuroIntervention 18, 1001–1010 (2022).
Pijls, N. H. J. et al. Coronary pressure measurement after stenting predicts adverse events at follow-up: a multicenter registry. Circulation 105, 2950–2954 (2002).
Matsuo, A. et al. Clinical implications of coronary pressure measurement after stent implantation. Cardiovasc. Interv. Ther. 28, 170–177 (2013).
Lee, J. M. et al. Prognostic implications of relative increase and final fractional flow reserve in patients with stent implantation. JACC Cardiovasc. Interv. 11, 2099–2109 (2018).
Hwang, D. et al. Influence of target vessel on prognostic relevance of fractional flow reserve after coronary stenting. EuroIntervention 15, 457–464 (2019).
van Bommel, R. J. et al. Routine fractional flow reserve measurement after percutaneous coronary intervention — the FFR-SEARCH study. Circ. Cardiovas. Interv. 12, e007428 (2019).
Stone, G. W. et al. 5-Year outcomes after bioresorbable coronary scaffolds implanted with improved technique. J. Am. Coll. Cardiol. 82, 183–195 (2023).
Boden, W. E. et al. Optimal medical therapy with or without PCI for stable coronary disease. N. Engl. J. Med. 356, 1503–1516 (2007).
Serruys, P. W. et al. Percutaneous coronary intervention versus coronary artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 360, 961–972 (2009).
Stone, G. W. et al. Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N. Engl. J. Med. 375, 2223–2235 (2016).
Farkouh, M. E. et al. Strategies for multivessel revascularization in patients with diabetes. N. Engl. J. Med. 367, 2375–2384 (2012).
Acknowledgements
The authors are supported in part by a Science Foundation Ireland Research Professorship Award (15/RP/2765) to W.W., which supports S.F., D.D. and J.H., and by grants from the Natural Science Foundation of China (no. 82020108015 and 81871460) to S.T. F.M. is supported by Deutsche Gesellschaft für Kardiologie, Deutsche Forschungsgemeinschaft (SFB TRR219, project ID 322900939) and Deutsche Herzstiftung.
Author information
Authors and Affiliations
Contributions
S.F., D.D. and W.W. researched data for the article. S.F., D.D., S.T. and W.W. discussed its content and wrote the manuscript. All the authors reviewed/edited the article before submission.
Corresponding authors
Ethics declarations
Competing interests
F.M. has received scientific support from Ablative Solutions, Medtronic and ReCor Medical and speaker honoraria/consulting fees from Ablative Solutions, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Inari, Medtronic, Merck, ReCor Medical, Servier and Terumo. A.J.L. has received consulting fees from MedAlliance and MicroPort. S.T. is the co-founder of Pulse Medical, and reports research grants and consultancy from Pulse Medical. W.W. reports grants and consulting fees from MicroPort, is a medical adviser for Corrib Core Laboratory and Rede Optimus, and is a co-founder of Argonauts, which is an innovation facilitator. All other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks William Boden, Antonio Colombo and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fezzi, S., Ding, D., Mahfoud, F. et al. Illusion of revascularization: does anyone achieve optimal revascularization during percutaneous coronary intervention?. Nat Rev Cardiol (2024). https://doi.org/10.1038/s41569-024-01014-0
Accepted:
Published:
DOI: https://doi.org/10.1038/s41569-024-01014-0