Abstract
Disruption of retinal vasculature is linked to various diseases, including diabetic retinopathy and macular degeneration, leading to vision loss. We present here a novel algorithmic approach that generates highly realistic digital models of human retinal blood vessels, based on established biophysical principles, including fully-connected arterial and venous trees with a single inlet and outlet. This approach, using physics-informed generative adversarial networks (PI-GAN), enables the segmentation and reconstruction of blood vessel networks with no human input and which out-performs human labelling. Segmentation of DRIVE and STARE retina photograph datasets provided near state-of-the-art vessel segmentation, with training on only a small (n = 100) simulated dataset. Our findings highlight the potential of PI-GAN for accurate retinal vasculature characterization, with implications for improving early disease detection, monitoring disease progression, and improving patient care.
Similar content being viewed by others
Introduction
Disruption of retinal vasculature is associated with a range of diseases which can result in loss of vision, including diabetic retinopathy (DR)1 and macular degeneration2. It is also increasingly recognized that retinal vasculature can indicate the presence of systemic pathology, such as vascular dementia3 and cardiovascular disease4. Automated methods to characterize and quantify changes in retinal vasculature from clinical imaging data therefore offer substantial promise for high-throughput, early detection of disease5, which is critically required to meet the increasing incidence of retinal disease, potentially alongside other vascular diseases, and their associated burden on healthcare systems6.
Much attention has been placed on supervised deep learning in this regard, where deep neural networks are trained to categorise images according to diagnosis or identify the location of features of interest7. Supervised learning, particularly with U-net architectures8, first rose to prominence in retinal image analysis for segmenting retinal layers in optical coherence tomography (OCT) data9, alongside blood vessel segmentation in retinal photographs10,11. A significant limitation to this type of approach is the lack of high-quality, manually-labelled image data in sufficient quantities to enable accurate and generalisable predictions to be made12. Novel deep learning architectures and hyperparameter selection are often employed to mitigate issues of smaller or lower quality datasets13,14, though there is consensus that the input data is of primary importance. The problem is particularly acute for the detection of blood vessels, in which manual labelling is highly time-consuming, generally limited to two-dimensional (2D) projections, confined to larger vessels only, and generally does not distinguish between arteries and veins15. Manual segmentation of a single 2D retinal image can take multiple hours16. Inter and intra grader variability can also be significant within the segmentation process17,18. Most segmentation studies have been conducted in 2D retinal fundus photographs using public datasets12,19,20. Previous studies have successfully used GAN based segmentation to segment retinal fundus21 and OCT-A22 images, without the need to create a generalisable model. Synthetic data approaches have also been deployed for blood vasculature on experimental imaging datasets (mesoscopic photoacoustic imaging)23. Approaches that utilise and extend these techniques for application on high resolution wide-field images are urgently needed to enable the robust translation of deep learning into the clinic.
To address these challenges, we describe here a novel set of algorithms that can generate highly realistic digital models of human retinal blood vessels, using established biophysical principles and unsupervised deep learning. Our biophysical models capture the complex structure of retinal vasculature, with interconnecting arterial and venous trees that are inherently three-dimensional, multi-scale and fully inter-connected via a capillary bed. They also feature dedicated macula and optic disc features. The central biophysical principles we draw on are (1) Murray’s Law, in which vessel diameters, branching distances and branching angles are optimised to form a balance between pumping power and blood volume and minimize resistance to flow24; and (2) fluid dynamics to model blood flow and vascular exchange. The latter is made possible by our synthetic networks containing fully-connected arterial and venous trees with a single inlet and outlet (the central retinal artery and vein), allowing blood flow and contrast agent delivery (e.g. fluorescein) data to be simulated with minimal assumptions in regard to network boundary conditions. The simulation of fluorescein angiography (FA) data, in which the time- and flow-dependent delivery of a contrast agent enables the characterisation of retinal vessels, is of particular interest as it facilitates the validation of temporal dynamics. The dye is also poorly tolerated by patients which reduces its usage clinically; simulated data could therefore be a valuable alternative25,26.
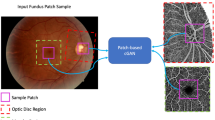
In this work, we investigate whether, through the use of generative deep learning, our biophysics-informed vascular network models can be used to infer information from real-world retinal images, such as the segmentation and reconstruction of blood vessel networks, without the need to perform any manual labelling, in an approach termed physics-informed generative adversarial learning (PI-GAN)27. An overview of our framework is provided in Fig. 1. Generative adversarial networks (GANs) incorporating cycle-consistency have previously been used for medical imaging domain machine learning tasks such as chest MRI to X-ray CT transformation28, PET image denoising29, and artefact reduction in fundus photography30. Likewise Menten et al used the space colonisation algorithm to generate macular blood vessel images, which they coupled with deep learning31.
Retinal blood vessel networks, featuring arterial and venous trees connected by a capillary bed, and special treatment of macula and optic disc features, were simulated using space filling growth algorithms based on Murray’s law. Blood flow and fluorescein delivery were simulated in synthetic vascular networks, using one-dimensional Poiseuille flow. By combining this with cycle-consistent, physics-informed deep generative learning, vessel simulations were converted into synthetic medical image data (fundus photography, Optical coherence tomography angiography (OCT-A) and FA), and the same trained networks used to detect blood vessels in clinical images. Image scale bar is given in millimeters (mm).
We demonstrate here the ability of our retinal simulation framework to accurately simulate real-world retinal vasculature, including blood flow, and model the presentation of two common vascular pathologies: DR and retinal vein occlusion (RVO). Moreover, we show that our PI-GAN workflow allows retinal vasculature to be segmented without any human manual labelling, and which outperforms state-of-the-art supervised learning approaches. This therefore offers numerous opportunities for improved detection and quantification of retinal disease in clinical ophthalmology.
Results
Procedural modelling of retinal vasculature
Retinal vascular networks were simulated in multiple, linked steps, using a combination of algorithms that draw on the known geometry and biophysics of retinal vasculature. In total, our procedural model of retinal vasculature contained 26 parameters (Supplementary Table 1), each of which were randomly sampled to simulate the broad range of retinal geometries occurring in the population (Fig. 2a–c)32,33.
a–c Examples of synthetic retinal vascular networks, featuring arterial (red) and venous (blue) trees, and with geometry optimised according to Murray’s law. Each simulation run used a different set of physiological parameter values, randomly sampled from the distributions defined in Supplemental Table 1. Scale bar is given in centimeters (cm). d–f A synthetic retina (d) with a 12 × 12 mm region surrounding the optic disc and macula (e) compared with a real OCT-A image (f). g A simulated vascular network projected onto three-dimensional surface (scale bar in millimeters (mm)).
Networks were seeded using a Lindenmayer-system (L-system)34, in which initial central retinal artery and vein segments were positioned at the location of an optic disc and iteratively branched within a plane. The first arterial and venous segment radii were 135 ± 15 µm and 151 ± 15 µm, respectively35. Branching was performed asymmetrically to create characteristically large vessels surrounding the macula, with smaller branches reaching towards the periphery, as observed in retinal images35.
Seeding L-systems were then grown to the edge of the retina using a variant of constrained constructive optimisation (CCO)36,37,38,39,40. This step transformed L-system networks into realistic, space-filling networks with geometries defined by Murrays law24 (exponent of 2.4 ± 0.1141), whilst retaining the realistic macroscopic branching geometry imposed by the L-system seeding (Fig. 2d–f). A final growth step was incorporated to create the characteristic branching pattern of the macula, with radial alignment of arterioles and venules, greater relative vascular flow density (between 1.5 and 2.0 times the perfusion fraction) and a central avascular fovea.
Following growth, we augmented vessels with sinusoidal displacements to replicate the tortuous vasculature commonly observed in human retinas, with a greater displacement imposed on veins. A continuous capillary bed was generated using either (1) a 2D Voronoi algorithm that arterial and venous endpoints were connected to42 or (2) a 2D space colonization algorithm43. Following simulation within a 2D plane, vessels were projected onto a hemispherical mesh (diameter 23–25 mm) featuring macula and optic disc structures generated using a mixed Gaussian profile44 (Fig. 2, Supplementary Fig. 1, Supplementary Video 1).
Comparison of synthetic networks with real-world networks
Our set of retinal network growth algorithms is designed to provide an authentic replication of real retinal vasculature, by following established biophysical principles. To quantitatively evaluate the accuracy of these synthetic networks, we manually labelled all visible blood vessels in 19 optical coherence tomography angiography (OCT-A) image datasets, using in-house software. This included differentiating arteries and veins (A-V) in a subset of images (n = 5), using retinal photographs as a reference for determining A-V status. Vessel branching angle, inter-branch length, tortuosity, and radius were measured in three regions: the macula, the vessels surrounding the optic disc, and the periphery. The macula was defined as a 5.5 mm diameter circular area centred on the fovea, based on measurements referenced in Remington and Goodwin45. The vessels surrounding the optic disc were labelled as a 3.6 mm diameter centred at the optic disc, due to mean vertical and horizontal diameters of the optic disc reported as 1.88 and 1.77 mm respectively46. Vessels outside these regions were defined as ‘peripheral’. 100 synthetic retinal networks were initially created, with parameter values randomly drawn from the ranges shown in Supplementary Table 1.
According to ANOVA analysis, all geometric parameters associated with synthetic blood vessel networks did not reach the level of statistical significance compared to those measured in controls using manual segmentation of OCT-A images (branching angle, p = 0.824; vessel length, p = 0.177; vessel tortuosity, p = 0.095; vessel network volume, p = 0.061; vessel diameter, p = 0.593) (Fig. 3, Supplementary Table 2).
The box plot displays the following summary statistics: median, lower and upper hinges (which correspond to the first and third quartiles (the 25th and 75th percentiles)), and upper and lower whiskers (the upper whisker extends from the hinge to the largest value no further than 1.5 x interquartile range (IQR) from the hinge), and the lower whisker extends from the hinge to the smallest value at most 1.5 x IQR. No replicates were included. A Branching angle, (B) vessel length (micrometers, µm) (length of the segment connecting two branch points in a graph vessel network), (C) vessel tortuosity (distance between vessel branching points divided by the Euclidean distance between them), (D) vessel volume (square micrometers, µm2) and (E) vessel diameter (micrometers, µm), in three regions: macula (5.5 mm diameter circular area centred on the fovea45), optic disc (3.6 mm diameter area centred on the optic disc centre46), and periphery (all vessels outside those regions). A two-sided Analysis of variance (ANOVA) was used to assess differences in these metrics by retina region (optic disc, macula, and periphery) and by status (healthy control and simulated network) (Supplementary Table 2) with eye (right OD/ left OS), participant sex, and OCT-A imaging scan pattern used as covariates.
Simulating retinal blood flow and validation using FA
We have previously developed a mathematical framework for simulating blood flow in three dimensional vascular networks, which uses one-dimensional Poiseuille flow47. Our simulated retinal networks are ideally suited for this framework, having just one arterial input and one venous outlet meaning that pressure boundary conditions can be easily specified. Setting arterial pressure by sampling from a normal distribution parameterised by mean = 56.2 mmHg, s.d. = 14.0 mmHg48 and similarly for venous pressure with mean = 20.0 mmHg and s.d. = 10.0 mmHg48 gave an average total retinal flow prediction of 34.4 ± 1.8 µL/min, which is slightly lower, but still in good agreement with reports in the literature from healthy retinas (for example, 45.6 ± 3.8 µL/min48 44 ± 13 µL/min49 50.7 µL/min49 (Fig. 4a, b)).
a Blood flow (microlitre per minute, µL/min) and (b) vascular pressure (millimeter of mercury, mm Hg) were simulated using Poiseuille flow, with inlet arterial pressure and outlet venous pressure fixed at 56.2 ± 14.0 and 20.0 ± 10.0 mmHg, respectively. c–e Simulated delivery of fluorescein at 17 s (arterial phase), 30 s (venous phase) and 600 s (recirculation), with clinical fluorescein images (registered to the same coordinate space) shown in (f–h) for comparison.
To further evaluate these flow results, we next performed a simulation of retinal fluorescein delivery. FA is used in ophthalmology for diagnosis of macular oedema, macular degeneration, RVO, DR, and other diseases26,50. Fluorescein is injected as a bolus into the median cubital vein, and 10–15 s later appears in the choroidal vasculature at the rear of the eye25. Within 2 s of this, fluorescein appears in the anterior arteries and arterioles, and a further 2 s later by partial filling of venules and veins, followed by total filling and recirculation.
We simulated the systemic pharmacokinetics of fluorescein using literature data4,51, with the passage of fluorescein modelled as two displaced Gaussian functions to model the first and second passes, and an exponential washout term corresponding to systemic extraction (Supplementary Fig. 2). This time course was propagated through our synthetic retinal networks by partitioning by flow at branch points and delaying according to cumulative velocities. The delay between arterial and venous filling with fluorescein, across 1000 simulation runs was 7.3 ± 0.7 s, which is in keeping with timings described in clinical data25. Visual inspection of fluorescein delivery also revealed a good accordance with clinical delivery profiles (Fig. 4c–h).
Simulating retinal pathology
Given the physiologically-realistic results provided by our flow models, we next sought to perturb our simulated networks to examine the effect of pathological changes. As a first demonstration, we simulated the effect of RVO. A random location of artery-vein crossover on a large retinal vein was reduced in diameter by 80%. Blood flow within the network was recalculated, revealing a large region of hypoperfusion, as expected. This strongly reflected the presentation of RVO found in clinical FA data (Fig. 5) and induced a regional reduction in blood flow of 9.8 µL/min in the vessels immediately downstream of the occlusion.
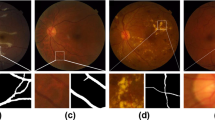
a An example of RVO simulation and loss of flow in downstream vessels. The yellow arrow shows the location of an imposed 80% decrease in vein diameter. The scale bar is in centimeters (cm) (b) An FA image of retinal occlusion, revealing a similar pattern of perfusion loss as simulated in (a). Colour bar unit is microliters per minute (c) The onset of DR, simulated by inhibiting flow in randomly-selected peripheral arterioles. d An OCT-A image of a retina exhibiting stage 4 DR, evidenced by extensive loss of perfusion in vessels and regions of ischaemia. The scale bar is shown in millimeters (mm).
Next, we constructed a simple model of DR52,53,54, in which arterioles with a radius <35 µm were randomly selected and occluded, and the resultant change in network flow calculated. All vessels that become non-perfused, either up- or downstream of the occluded vessel, were removed from the network, creating regions of ischaemia, with occasional surviving vessels passing through (Fig. 5c, d, Supplementary Fig. 3). Occlusions were simulated in batches of 5, initially from the periphery (>1 cm from the macula centre), and then at decreasing minimum distances from the macula, as typically found in the clinical presentation of DR.
Both our retinal occlusion model and DR model produced images that were highly reminiscent of clinical images of both pathologies (Fig. 5), with loss of flow in downstream vessels in our RVO model and loss of perfusion and regions of ischaemia in the DR model.
Generating synthetic clinical ophthalmology data with deep learning
Our next challenge was to use deep learning to define a mapping between our biophysical vascular model and clinical ophthalmology data (and vice versa). For this we used cycle-consistent generative adversarial networks that enabled the translation of image texture and style between image domains55. We undertook this for three clinical imaging modalities: OCT-A, retinal photographs and FA.
We embedded our synthetic retinas in three-dimensional grids with axial and lateral resolutions of 6.3 µm and 21 µm, respectively, to match our clinical OCT-A data. We then trained three cycle-consistent GANs on these synthetic retinas, with each GAN mapping the conversion between the synthetic images and a different imaging modality (Supplementary Fig. 4). 590 retinal photographs, 43 OCT-A en-face images and 570 FA images were used in training for this purpose. PI-GAN enabled the geometry of source images (simulations- synthetic space) to be translated into a target style (retinal photographs- retinal photograph space, OCT-A- OCT-A space, and FA- FA- space). As can be seen in Fig. 6a, following 400 training epochs, the pattern of synthetic vasculature was realistically transferred into the style of each target image. The Frechet Inception Distance (FID)56 was 6.95 for retinal photographs, 5.17 for FA and 3.06 for OCT-A en-face images, indicating a small distance between feature vectors for real and synthetic images. FID calculated between two sets of real images from the same domain was used as a baseline (Supplementary Table 3).
a Direction 1 involves conversion of synthetic space (simulated network) into retinal photograph space, Optical coherence tomography angiography (OCT-A) space and fluorescein angiography (FA) space. b Direction 2 involves conversion of real retinal images (retinal photograph, OCT-A, and FA spaces) into fully connected networks/segmented data (synthetic space).
This process generated authentic-looking retinal image data with matched, fully specified ground truth blood vessels. However, cycle consistency also allows the reverse operation: to generate simulation data from clinical images (Fig. 6b). This enabled blood vessel networks to be segmented from OCT-A images and compared with manual segmentations of the same data (Fig. 7). For segmentation of OCT-A data we trained PI-GAN with a synthetic dataset instance featuring smaller ‘elusive’ vessels57 and capillary level vasculature. Visual inspection of PI-GAN segmentations revealed many more small ‘elusive’ vessels than represented within our manually-segmented images, arguably providing superior segmentation accuracy than the manual ‘gold standard’. Accordingly, the mean Dice score for OCT-A images was low (mean 0.35, s.d. 0.12 (2.s.f)), but the sensitivity (the percentage of pixels labelled as vessel in the manual segmentation that were also identified as vessel by PI-GAN) was high (87.1% (s.d. 1.20)), showing that PI-GAN is able to accurately label almost all of the vessels identified by human operators (Fig. 7g–j).
a–d OCT-A en-face images of retinal vasculature. b–e The same OCT-A images with vessel segmentations from PI-GAN. c–f Segmented vessels projected in three-dimensional space, colour-coded for vessel radius. g An OCT-A image with (h) manually-segmented and (i) PI-GAN-segmented blood vessels. j A composite image of manually- and PI-GAN-segmentations, with overlapping pixels rendered white, pixels with only PI-GAN-detected vessels in blue and pixels with only manual-detected vessels in red. k A retinal photograph taken from the DRIVE data set72 with (l) manually-segmented and (m) PI-GAN-segmented blood vessels. Scale bars are provided in millimeters (mm).
To further investigate the accuracy of the PI-GAN segmentation, we evaluated PI-GAN on two publicly available retinal photograph data sets with corresponding manual segmentations (STARE19 and DRIVE20). PI-GAN was trained here using a synthetic dataset filtered such that the smallest vessel diameter corresponded to the resolution of retinal photography (taken to be 100 µm). Contrasting the widefield (130° and 200°) retinal photograph images analyzed in this study, these public datasets were acquired with a smaller 45 degree FOV, and are widely used in benchmarking vessel segmentation. Dice scores indicated a high accordance between manual segmentations and PI-GAN segmentations (0.75 (0.11) for DRIVE and 0.82 (0.091) for STARE datasets (Supplementary Fig. 4)). These values compare favourably against previous methods using manually labelled data58 for which state-of-the-art was 0.8378 for STARE and 0.8275 for DRIVE, particularly given our absence of manual labelling and limited quantity of training data.
These results call into question how appropriate manual segmentation is as a gold standard in this setting; visual inspection suggests these additional small vessels labelled in the OCT-A data are indeed physiological and were simply missed by manual segmentation. PI-GAN achieved high accuracy comparable with state of the art, and demonstrated potential in accessing smaller vessels in higher resolution images.
They also demonstrate the key ability of physics-informed simulations with deep learning to autonomously segment blood vessels within a range of ophthalmology imaging modalities, without the need for any manually labelled training data.
Discussion
We have presented a physics-informed, generative approach that combines biophysical simulation with deep generative learning, to support quantitative assessment of retinal vasculature in clinical ophthalmology, alongside supporting research into the retinal presentation of systemic diseases such as cardiovascular disease and vascular dementia3,4. A useful outcome of this approach is the ability to automatically segment vascular data from clinical evaluation images, without any need for manual segmentation. Specifically, we created a linked set of algorithms that draw on established principles in biophysics to simulate fully-connected retinal vasculature, in a three-dimensional domain, with special treatment for optic disc and macula regions. The full connectivity of our models, with separate arterial and venous trees, enables realistic blood flow and delivery simulations (for example, as we show in FA). We demonstrated that our synthetic vascular networks are highly concordant with real retinal vasculature metrics, with network statistics matching those from manual segmentations, in three regions: the optic disc, macula and periphery.
This close accordance between simulation and real-world geometries is key to its ability to segment blood vessels from ophthalmology images. Cycle-consistent deep generative learning allowed us to create realistic fundus photograph, OCT-A and FA images that inherently maintained feature geometry through the translation from simulation to clinical image domains. The resultant data are inherently paired, and so could provide data to augment conventional supervised learning approaches. However, cycle-consistency also facilitates the reverse translation, from clinical image domains back into the simulation domain, allowing the automated segmentation of blood vessels without human-labelled data. Comparing segmentation performance against manual segmentations revealed a much greater ability to label small vessels in high resolution images, and with excellent overlap with larger manually-segmented vessels. Overall performance assessed via Dice score for OCT-A showed a relatively low accordance, due in part to the greater ability of the PI-GAN approach to detect small blood vessels omitted from manual segmentations, but also false-positives in human-labels, alongside a small number (0.67%) of false-positive PI-GAN-labelled vessels (‘hallucinations’59). Benchmarking PI-GAN segmentations against publicly-available retinal photograph datasets returned Dice scores aligned with state of the art, which is remarkable for a technique that requires no human oversight.
To date, supervised deep learning approaches have yielded impressive results in 2D vessel segmentation relative to manual segmentation, although tend to favour precision over recall5, resulting in an under-segmentation of faint vessels, underestimation of the width of thicker vessels and some ‘elusive’ vessels being missed57. This is problematic for diagnostic interpretation, because many biomarkers (such as artery-vein (AV) ratio, branching angles, number of bifurcations, fractal dimension and tortuosity) need precise measurements of individual vessels. GANs incorporating cycle-consistency have previously been used for medical imaging domain machine learning tasks such as chest MRI to X-ray CT transformation28, PET image denoising29, and artefact reduction in fundus photography30. Likewise Menten et al used the space colonisation algorithm to generate macular blood vessel images, which they coupled with deep learning31.
Our approach builds on this by incorporating biophysically-informed models of flow within fully-connected artery and venous networks that extend across the entire retina, and our use of it to inform cycle-consistent deep generative learning. These developments allow application in larger field of view images (e.g. wide-field fundus photography), and also enable a large range of future applications, including flow modelling and oxygen delivery60. Moreover, given our ability to model arterial and venous trees, there is potential for independent segmentation of both vascular supplies.
These biophysical simulations also aimed to capture the wide range of variation found in real retinal networks, by varying the 26 simulation parameters across their reported physiological range. A further advantage of developing flow models into our biophysical framework was the ability to simulate pathology, such as the progression of DR and RVO. Many other pathologies could be simulated in follow-on studies, including changes in retinal vessel diameters associated with factors such as aging or hypertension. For example, Wong and colleagues reported retinal arteriolar diameters to decrease by ~2.1 µm for each decade increase in age, and by 4.4 µm for each 10 mmHg increase in arterial blood pressure61. Performing disease-specific deep generative learning runs will enable us to further refine our segmentation approaches and begin to characterise pathology.
Accordingly, there is also potential to use clinical data to further improve our biophysical simulations, enabling more accurate modelling of retinal physiology (and disease) and the ability to develop interpretable AI systems. The results of several recent studies using deep learning suggest that that retinal vasculature can provide a window into many systemic diseases (including dementia3, kidney disease62 and cardiovascular disease4), but cannot easily explain the structural basis of these associations. A PI-GAN framework is inherently coupled to biophysical laws, and so could help determine their origins or underpinning mechanistic processes. Additional challenges for segmentation are artery-vein classification63 and establishing connectivity of the vessels64, which, having a well-defined ground truth data set from simulations, could be realised through PI-GAN.
Overall our results demonstrate the potential of biophysical models of the retina, which can be interrogated to understand how physiological perturbations (such as disease) effect vascular function. Further work could explore regional variability in blood flow, with the temporal side exhibiting greater flow than the nasal side in both retinal venules and arteries, which may be related to retinal ganglion cell numbers65. Additionally, the model could be used in predicting inhibitors of angiogenesis, such as VEGF inhibitor Bevacizumab. Incorporating this model into a larger-scale retinal model (including the choroidal supply) would enable complete simulation of the retinal supply. The ability to then apply these simulation results for the interpretation of clinical images, via physics-informed generative learning, is a significant step forward.
Methods
Procedural generation of synthetic retinal vasculature
Algorithms for generating synthetic retinas followed multiple, length scale dependent steps66. Firstly, the values of geometrical parameters were set by sampling from a normal or uniform distribution according to parameter values shown in Supplementary Table 1. Retinal vasculature took the form of spatial graphs (i.e. branching nodes connected via vessel segments) which were initially seeded using a Lindenmayer system (L-system), and then extended using constrained constructive optimisation (CCO) and Lattice Sequence Vascularisation (LSV). For the L-system (see Github directory: retinasim/lsystemlib/) retinal artery and retinal vein segments were initially directed from a central optic disc point and branched by five generation to form seeding retinal arcades. These were passed into the CCO algorithm, followed by LSV, to further branch the vessels in progressively finer resolutions. Once complete, the macula region was cleared and regrown into a radially-spaced lattice (https://github.com/AndrewAGuy/vascular-networks). Finally, spatial undulations were imposed onto the vessels by overlaying sinusoidal curves with randomised frequencies and amplitudes (retinasim/sine_interpolate.py). These implementation of these linked algorithms is described further in the sections below.
Lindenmeyer system seeding
Firstly, seeding networks following approximate retinal vascular branching geometry were constructed, starting with a putative central retinal artery and retinal vein positioned at the centre of the optic disc. The diameters of the retinal artery and vein were 135 ± 15 μm and 151 ± 15 μm, respectively35, oriented parallel to the optic nerve (defined as the z-direction). Two branches were added to the end of each of these segments, oriented in the x-y plane, and one directed above and the other below the retinal midline. Subsequent branching of these vessels was performed stochastically, with segment lengths between bifurcations set as a fixed fraction of vessel diameter (18 ± 3) and bifurcation vessel diameters set according to:
Normally-distributed noise was added to branching angle values, with a standard deviation of 5°. Vessel bifurcation angles were assigned such that the larger vessel oriented towards the macula to create putative major vessels oriented around the macula. Fifth-order bifurcations were added to the network, or until vessels breached the edge of the retina domain. Supplementary Fig. 1a shows an example of an L-system seeding network.
Major vessel growth
Seed vessel networks were used as input into a multi-scale growth algorithm for the creation of hierarchical vasculature. First, seed networks were amended to provide a uniform distribution of leaf nodes (terminating arteriole and venuole nodes created prior to construction of capillary networks at a later stage) throughout the circular domain, using Accelerated Constrained Constructive Optimisation40, using a leaf node spacing of 3 mm. Multiscale, two-dimensional lattices were defined (stride lengths ranging from 3000 to 150 µm, with five iterations linearly spaced within that range) and used to grow vessel networks by progressively adding vessels into unoccupied lattice sites from neighbouring occupied sites, choosing the candidate vessel which minimised the expected change in network cost (see below), and progressively reducing the length scale when no more progress could be made. After the initial growth stage, all existing leaf nodes were removed67. At all stages of the major vessel growth the macula region was kept free of vessels by removing vessels which intersected it, forcing flow to divert around it.
As retinal vasculature is positioned in front of the retina itself, we optimised networks to minimise the area of the retina occluded by vessels, according to a cost function based on Murray’s law:
with ρ = 1 and λ = 1, and where B is the set of vessel segments in the network, with length l and radius r. After each growth step the network geometry was optimised by moving vessel nodes, and highly asymmetric bifurcations were trimmed for regrowth40 using the thresholds from ref. 39 to account for the high asymmetry of optimal networks39. After growth at each length scale was terminated, the networks were optimised topologically by allowing asymmetric bifurcations to move their low-flow side downstream and branches which were short compared to their expected length under the West, Brown and Enquist model68 to be treated as a single higher-order split for regrouping using a method similar to69. Due to the two-dimensional nature of the networks, network self-intersections were tested for using the approach of40 however, rather than resolving the intersections by making excursions around the contact site we rewire the vessels to prevent future iterations from recreating the same intersection.
Unlike the implementation of ref. 40, leaf nodes were allowed to move from their nominal location up to a specified “pinning distance”, given as a fraction of the leaf spacing. Existing vessels could be specified as frozen, in which case the optimiser did not touch them. This approach was used to perturb the optimal root vessel structure with artificial tortuosity, strip away the downstream branches and regrow the downstream vessels, repeating this down the tree structure.
Macula growth
Vessels supplying the macula have a characteristic radial structure, motivating the development of a particular approach to enforce this structure. This uses the same lattice site invasion approach between the macula outer radius and the fovea (which is kept vessel-free), but with the stride set low enough that the majority of the growth arises from spreading over many iterations at the same length scale rather than hierarchical refinement. The macula has a configurable flow rate density compared to the rest of the retina, ranging from 1.5 – 2.0 and leaf nodes are offset by uniformly sampling an offset in a disc around the nominal position to ensure that vessels did not align along the lattice sites. The macular vessels were prevented from doubling back on themselves by setting a hard limit on the vessel angle, preventing obviously non-physiological structures from arising whilst still allowing the radial pattern to develop. After all leaf nodes are created, a sparsity factor is specified and each leaf node removed with this probability, then the remaining vessels are geometrically optimised.
Network overpass and interleaving
In the final stage, the arterial and venous networks have their collisions resolved using the method of ref. 40, creating out-of-plane excursions around contact sites between the networks. To enable further micro-scale network growth techniques to create an interdigitated structure, we remove the low-flow side of all arterio-venous intersections with a radius below a critical value (5 um), leaving surviving vessel geometry untouched. Interdigitations were then created using a Space Colonisation implementation70, interspersed with geometric optimisation.
Vessel tortuosity
The multi-scale growth algorithm creates relatively straight paths between branching points, and to simulate tortuous retinal vessels, particularly in veins, sinusoidal displacements were overlaid. Two oscillations were superimposed according to:
where d(x,r) is the path taken by a vessel with radius r, and d’(x,r) is the modulated path. The amplitude of displacements, a0 + a1 ranged from r –3.5r for arteries and r –7.5r for veins, with a low frequency period (τ0, ranging from 15r – 25r) and a high frequency period (τ1, ranging from 30r – 50r). The phase of the modulations, φ0 and φ1, enabled modulations to be matched between vessel bifurcations.
Simulating vascular flow and fluorescein delivery
Blood flow in retinal networks were simulated using our REANIMATE platform47, which uses a connectivity-based formalism to optimise Poiseuille flow in tree-like spatial graphs. As anterior retinal vasculature features a single arterial inlet and venous outlet, the system requires only one pressure boundary condition (the difference between arterial and venous inlet pressures), which was fixed at 56.2 ± 14.0 and 20.0 ± 10.0 mmHg, respectively.
Time-dependent delivery of contrast agent (e.g. fluorescein) was simulated as described in d’Esposito et al.47. Briefly, a bolus of fluorescein was simulated according to
where C(t) is the concentration of fluorescein as a function of time t. The first two terms, Gaussian functions, represent the first and second pass of the bolus and the third term, an exponential decay, represents the washout phase51 The width of the first and second pass were σ1 = 10 s and σ2 = 25 s, respectively, and the decay rate of the washout phase, β, was 0.043 /minute. T1, t2 and τ are the time to peak for the first pass, second pass and washout phases, and were set at 0.171, 0.364 and 0.482 min, respectively51. S1, s2 and α were fixed at 0.833, 0.336 and 1.064 (dimensionless units). Peak concentration was normalised to unity at the inlet to the retinal artery and the time course in each connected vessel segment was time-shifted according to the velocity of blood in each vessel and scaled according to the ratio of flow in the parent and child vessels at bifurcation points.
Image datasets
This study was carried out in accordance with the Declaration of Helsinki71. Ethical approval of retrospective audit data was obtained through Moorfields Eye Hospital Research and Development and Audit number 1078. Informed consent was not obtained for retrospective data. Participants were not compensated as retrospective data was utilized. Only de-identified retrospective data was used for research, without the active involvement of patients. Sex was self-reported by study participants. Clinical ophthalmological retinal images were obtained from equipment at Moorfields Eye Hospital NHS Trust, London, UK: OCT-A images were obtained from a PLEX Elite 9000 (Carl Zeiss Meditec LLC, Dublin, CA, USA), ultra-wide true colour retinal photographs were obtained from Zeiss Clarus 500 Fundus machine (Carl Zeiss Meditec LLC, Dublin, CA, USA), fluorescein angiograms were obtained from Optos widefield camera (Optos, Inc. Marlborough, MA, USA). 19 manually segmented OCT-A images were obtained from healthy controls not ascertained for disease status (10 male, 9 female, mean age 39.89 (s.d. 11.25)). These manual segmentations were used in comparison of network structure with simulated networks. Datasets of 570 FA images, 590 colour retinal photographs, 43 OCT-A en-face images, and 130 simulated networks were used in training and testing the PI-GAN algorithm.
Manual labelling of clinical data
Manually labelled data was generated using a custom-built Python package enabling tracing of vasculature in 3D. The process involved placing user defining control points on the 2D image indicating where in a slab the vessel is located via maximum intensity projection. The z-height of the vessel was then fixed by identifying the height of the highest signal intensity voxel, which was manually constrained to exclude the choroid or RPE. The radius of each vessel was automatically calculated by setting a user-defined signal intensity threshold. Review of segmented structures was performed in 3D panel to assess and ensure labelling quality. In images with pathological blood vessels such as DR the abnormal vasculature or areas of neoangiogenesis were traced in the same manner. Vessel information (vessel coordinates, edge connectivity, number of edge points, edge point coordinates, radii, and vessel type) was exported and stored in Amira spatial graph format (ThermoFisher Scientific, Waltham, Massachussetts USA). Retinal regions were labelled. The macula was defined as a 5.5 mm diameter circular area centred on the fovea. The vessels surrounding the optic disc were labelled as a 3.6 mm diameter centred at the optic disc. Vessels outside these regions were defined as ‘peripheral’.
Deep generative learning
Image-to-image translation was performed using cycle-consistent generative adversarial networks30. This algorithm enables automated unsupervised training with unpaired samples, learning a bi-directional mapping function between two different domains with deep generative adversarial networks. It utilises cycle consistency, where the reconstructed image obtained by a cycle adaptation is expected to be identical to the original image for both generative networks. Cycle-consistent GANs are composed of two main deep neural network blocks which are trained simultaneously: an image generator (generator) and an adversarial network (discriminator). There is a loss (G loss) to make a synthesised image from domain A closer to a real image from domain B, and a loss (D loss) to distinguish the synthesised image from domain A from a real image from A. There are also losses facilitating the conversion in the opposite direction (G loss making synthesised image from domain B closer to domain A, and D loss to distinguish synthesised and real domain B images). Additionally, cycle loss is the difference between the input image and the double-synthesised image and identity loss is the difference between output and input images. A train/validation/test split of 75%/5%/20% was used. All PI-GANtraining and evaluation was performed using a single NVIDIA Titan RTX GPU.
We iteratively trained a switchable PI-GAN algorithm with 500 epochs (Supplemental Fig. 5). All networks were trained using the optimizer ADAM solver35 with β1 = 0.5, β2 = 0.999. The learning rate for the first 100 epochs was 2 * 10−4, and then linearly decayed to 2 * 10−6. Images were pre-processed with crop size 256 pixels. The minibatch size was 1. The loss weights λ were set as 10. The model was trained on NVIDIA TITAN RTX in Pytorch v1.9.1.
Loss functions
Adversarial losses
For mapping function G : X → Y and its discriminator DY, the objective is expressed as:
Where G attempts image generation G(x) to look similar to images from domain Y and DY tries to distinguish between translated samples G(x) and real samples y55.
Cycle consistency loss
Cycle consistency loss is utilised to reduce the space of possible mapping functions to the target domain; the image translation cycle aims to bring an image back from its translation to the original. The images should satisfy both forward and backward cycle consistency. The mapping from one image, to translated domain, back to original is incentivised using the cycle consistency loss:
Identity loss
An additional loss is utilised to regularise the generator to be near an identity mapping when real samples from the target domain are used as the input of the generator:
Statistical evaluation of synthetic vessel networks
Vessel metrics of vessel branching angle, length, tortuosity, network volume and diameter were calculated. Two-sided Analysis of variance (ANOVA) was used to assess differences in these metrics by retina region (optic disc, macula, and periphery) and by status (healthy control and simulated network) (Supplementary Table 2) with eye (right OD/ left OS), participant sex, and OCT-A imaging scan pattern used as covariates.
Expert evaluation of PI-GAN vessels
A clinical expert (consultant ophthalmologist at Moorfields Eye Hospital with fellowship-level subspecialty training in medical retinal disease and extensive clinical experience (14 years of experience)) reviewed the original segmentations from DRIVE and STARE datasets along with the corresponding images. Using evaluation in regions ‘disc’, ‘centre’ and ‘mid-periphery’, they evaluated all reviewed images as containing ‘possible’ small vessels. Their evaluation was that for 90% of DRIVE and 80.95% of STARE images, PI-GAN segmented additional vessels that were not seen in the original segmentation, that they considered ‘possibly’ present in the retinas. The remaining images were ranked ‘unclear’. They noted that image quality for DRIVE/STARE datasets was a limiting factor in conclusively determining the presence of smaller vessels.
Evaluation metrics
Frechet inception distance
GAN output was evaluated using the Fréchet Inception Distance (FID), which evaluates model quality by calculating the distance between feature vectors for real and generated images. FID compares the distribution of generated images with distribution of real images that were used to train the generator. Lower FID scores indicate more similarity between two groups. The FID score is calculated by first loading a pre-trained Inception v3 model. The output layer of the model is removed and the output is taken as the activations from the last pooling layer, a global spatial pooling layer.
Three FID scores were calculated: real simulation images (synthetic space) versus manually segmented vasculature clinical images; real retinal photographs (retinal photograph space) versus PI-GAN generated retinal photographs; real OCT-A images (OCT-A space) versus PI-GAN generated OCT-A images; real FA (FA space) versus PI-GAN generated FA images.
Dice score
Dice scores were additionally calculated. This is a commonly used performance statistic for evaluating the similarity of two samples. For a ground truth segmentation label L and associated prediction P, we measure the binary Dice score D:
We carried out benchmarking of the PI-GAN algorithm against other models trained for manual segmentations from segmentation of retinal vessels using STARE, and DRIVE datasets public datasets, which are regularly used for benchmarking of algorithm results19,72. Dice score were evaluated from the output of PI-GAN trained to carry out the mapping between simulated data segmentations and retinal photographs and compared to GAN performance without synthetic data.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data supporting the findings are available in the article, the Supplementary Information, and from the corresponding author upon request, aside from data that is subject to the restrictions detailed below. Source retinal simulation data have been deposited on FigShare (https://figshare.com/articles/dataset/sim00000000_zip/26364181, https://doi.org/10.6084/m9.figshare.26364181) and Dropbox (https://www.dropbox.com/scl/fo/whwru5rmz8g7cr0h8ytg1/h?rlkey=ynbh2kdhe0pcvpfo6cypm9oc6&dl=0). The Moorfields Eye Hospital data is protected and subject to restrictions of data sharing due to its sensitive nature and privacy concerns, as it is patient or research participant data and is not available for access to the wider research community without data share agreements. Access to the data is managed by the audit department and Moorfields Research and Development, along with timeframes to responses to requests, and details of restrictions on data use via data use agreements (https://www.moorfields.nhs.uk/research/). DRIVE and STARE datasets are available online. Use of data from these online sources complies with database terms and conditions.
Code availability
All code is available in https://github.com/simonwalkersamuel/retinasim/tree/main66. RetinaSim, and relies on several libraries: (1) The code in this repository (RetinaSim) is written in python (3.8), and both provides functionality and glues together the other libraries; (2) Reanimate for 1D flow simulation (provided here as a submodule); (3) RetinaGen for procedural modelling of blood vessel networks (provided here as a submodule); (4) Pymira for creating and editing spatial graph structures in python (provided here as a submodule). Installation instruction is provided on the GitHub repository. Deep generative learning was performed using an adaptation of https://github.com/junyanz/pytorch-CycleGAN-and-pix2pix provided in the RetinaSim codebase.
References
Shin, E. S., Sorenson, C. M. & Sheibani, N. Diabetes and retinal vascular dysfunction. J. Ophthalmic. Vis. Res. 9, 362–373 (2014).
Trinh, M., Kalloniatis, M. & Nivison-Smith, L. Vascular changes in intermediate age-related macular degeneration quantified using optical coherence tomography angiography. Transl. Vis. Sci. Technol. 8, 20 (2019).
Czako, C. et al. Retinal biomarkers for Alzheimer’s disease and vascular cognitive impairment and dementia (VCID): implication for early diagnosis and prognosis. Geroscience 42, 1499–1525 (2020).
McClintic, B. R. et al. The relationship between retinal microvascular abnormalities and coronary heart disease: a review. Am. J. Med. 123, 374.e1–374.e7 (2010).
Khanal, A., Estrada, R. Dynamic deep networks for retinal vessel segmentation. Front. Comput. Sci. https://doi.org/10.3389/fcomp.2020.00035 (2020).
Ting, D. S., Cheung, G. C. & Wong, T. Y. Diabetic retinopathy: global prevalence, major risk factors, screening practices and public health challenges: a review. Clin. Exp. Ophthalmol. 44, 260–277 (2016).
Aljuaid, A. & Anwar, M. Survey of supervised learning for medical image processing. SN Comput. Sci. 3, 292 (2022).
Ronneberger, O., Fischer, P., & Brox, T. U-net: convolutional networks for biomedical image segmentation. In, Medical Image Computing and Computer-Assisted Intervention—MICCAI 2015. MICCAI 2015 (Navab, N., Hornegger, J., Wells, W., Frangi, A.) 9351 (Springer, Cham, 2015).
De Fauw, J. et al. Clinically applicable deep learning for diagnosis and referral in retinal disease. Nat. Med. 24, 1342–1350 (2018).
Hussain, S. et al. DilUnet: A U-net based architecture for blood vessels segmentation. Comput. Methods Prog. Biomed. 218, 106732 (2022).
Ren, K. et al. An improved U-net based retinal vessel image segmentation method. Heliyon 8, e11187 (2022).
Jin, K. et al. FIVES: A fundus image dataset for artificial intelligence based vessel segmentation. Sci Data 9, 475 (2022).
Li, C. et al. Attention unet++: A nested attention-aware u-net for liver ct image segmentation. In 2020 IEEE int. conference on image processing (ICIP). 345–349 (IEEE, 2020).
Kipf, T. N., Welling, M. Semi-supervised classification with graph convolutional networks. arXiv https://doi.org/10.48550/arXiv.1609.02907 (2016).
de Moura, J., Novo, J., Ortega, M., & Charlón, P. 3D retinal vessel tree segmentation and reconstruction with OCT images. In Image Analysis and Recognition. (eds. Campilho, A., Karray, F.) 9730 (Springer, Cham, 2016).
Meng, X. et al. A framework for retinal vasculature segmentation based on matched filters. Biomed. Eng. Online 14, 94 (2015).
Covert, E. C. et al. Intra- and inter-operator variability in MRI-based manual segmentation of HCC lesions and its impact on dosimetry. EJNMMI Phys. 9, 90 (2022).
Veiga-Canuto, D. et al. Comparative multicentric evaluation of inter-observer variability in manual and automatic segmentation of neuroblastic tumors in magnetic resonance images. Cancers (Basel). 14, 3648 (2022).
Hoover, A., Kouznetsova, V. & Goldbaum, M. Locating blood vessels in retinal images by piecewise threshold probing of a matched filter response. IEEE Trans. Med. Imaging. 19, 203–210 (2000).
Staal, J. et al. Ridge-based vessel segmentation in color images of the retina. IEEE Trans. Med. Imaging. 23, 501–509 (2004).
Andreini, P. et al. A two-stage gan for high-resolution retinal image generation and segmentation. Electronics 11, 60 (2021).
Kreitner, L. et al. Synthetic optical coherence tomography angiographs for detailed retinal vessel segmentation without human annotations. IEEE Transactions on Medical Imaging. (2024).
Sweeney, P. W. et al. Segmentation of 3D blood vessel networks using unsupervised deep learning. bioRxiv https://doi.org/10.1101/2023.04.30.538453 (2023).
Sherman, T. F. On connecting large vessels to small. The meaning of Murray’s law. J. Gen. Physiol. 78, 431–453 (1981).
Ruia, S. & Tripathy, K. Fluorescein Angiography (StatPearls Publishing, 2023).
Marmor, M. F. & Ravin, J. G. Fluorescein angiography: insight and serendipity a half century ago. Arch Ophthalmol 129, 943–948 (2011).
Liu, Y., Zhang, D. & Karniadakis, G. M. Physics-informed generative adversarial networks for stochastic differential equations. SIAM J. Sci. Comput. 42, A292–A317 (2020).
Matsuo, H. et al. Unsupervised-learning-based method for chest MRI-CT transformation using structure constrained unsupervised generative attention networks. Sci. Rep. 12, 11090 (2022).
Zhou, L. et al. Supervised learning with Cyclegan for low-dose FDG PET image denoising. Med. Image Anal. 65, 101770 (2020).
Yoo, T. K., Choi, J. Y. & Kim, H. K. CycleGAN-based deep learning technique for artifact reduction in fundus photography. Graefes Arch. Clin. Exp. Ophthalmol. 258, 1631–1637 (2020).
Menten, M. J. et al. Physiology-based simulation of the retinal vasculature enables annotation-free segmentation of OCT angiographs. In Medical Image Computing and Computer Assisted Intervention–MICCAI 2022. (eds. Wang, L., Dou, Q., Fletcher, P.T., Speidel, S., Li, S.) 13438 (Springer, Cham, 2022).
Miller, D. Optics and Refraction: a User-Friendly Guide 0th edn (Gower Medical Pub, 1991).
Mukherjee, P. K. Manual of Optics and Refraction (Jaypee Brothers Medical Publishers, 2015).
Lindenmayer, A. Mathematical models for cellular interactions in development. II. Simple and branching filaments with two-sided inputs. J. Theor. Biol. 18, 300–315 (1968).
Goldenberg, D. et al. Diameters of retinal blood vessels in a healthy cohort as measured by spectral domain optical coherence tomography. Retina 33, 1888–1894 (2013).
Liu, X., Liu, H, Hao, A & Zhao, Q. Simulation of blood vessels for surgery simulators. In Int. Conf. Machine Vision and Human-machine Interface. 377–380 (2010).
Galarreta-Valverde, M. A., Macedo, M., Mekkaoui, C. & Jackowski, M. Three-dimensional synthetic blood vessel generation using stochastic L-systems. In Medical Imaging 2013: Image Processing, International Society for Optics and Photonics. 8669 (SPIE, 2013).
Buxbaum, P. F., Schreiner, W. Computer-optimization of vascular trees. in IEEE Trans. Biomed. Eng. 40, 482–91 (1993).
Schreiner, W. et al. The influence of optimization target selection on the structure of arterial tree models generated by constrained constructive optimization. J. Gen. Physiol. 106, 583–599 (1995).
Guy, A. A. et al. 3D printable vascular networks generated by accelerated constrained constructive optimization for tissue engineering. IEEE Trans. Biomed. Eng. 67, 1650–1663 (2020).
Luo, T. et al. Retinal vascular branching in healthy and diabetic subjects. Invest. Ophthalmol. Vis. Sci. 58, 2685–2694 (2017).
Smith, A. F. et al. Brain capillary networks across species: a few simple organizational requirements are sufficient to reproduce both structure and function. Front. Physiol. 10, 233 (2019).
Runions, A., Lane, B., Prusinkiewicz, P. Modelling Trees with a Space Colonization Algorithm in Eurographics Workshop on Natural Phenomena. http://algorithmicbotany.org/papers/colonization.egwnp2007.large.pdf (algorithmicbotany.org)(2007).
Tariq, A., Shaukat, A & Khan, S. A. A gaussian mixture model based system for detection of macula in fundus images. In Neural Information Processing: 19th International Conference, ICONIP. (eds. Huang, T., Zeng, Z., Li, C., Leung, C.S.) 7664 (Springer, Berlin, Heidelberg, 2012).
Remington, L. A., & Goodwin, D. Clinical Anatomy and Physiology of the Visual System E-Book 4th edn, Vol. 350 (Elsevier Health Sciences, 2021).
Quigley, H. A. et al. The size and shape of the optic disc in normal human eyes. Arch. Ophthalmol. 108, 51–57 (1990).
d’Esposito, A. et al. Computational fluid dynamics with imaging of cleared tissue and of in vivo perfusion predicts drug uptake and treatment responses in tumours. Nat. Biomed. Eng. 2, 773–787 (2018).
Sun, R. et al. Central retinal artery pressure and carotid artery stenosis. Exp. Ther. Med. 11, 873–877 (2016).
Baumann, B. et al. Total retinal blood flow measurement with ultrahigh speed swept source/fourier domain OCT. Biomed. Opt. Express 2, 1539–1552 (2011).
Savastano, M. C. et al. Fluorescein angiography versus optical coherence tomography angiography: FA vs OCTA Italian study. Eur. J. Ophthalmol. 31, 514–520 (2021).
Parker, G. J. et al. Experimentally-derived functional form for a population-averaged high-temporal-resolution arterial input function for dynamic contrast-enhanced MRI. Magn. Reson. Med. 56, 993–1000 (2006).
Bek, T. Diameter changes of retinal vessels in diabetic retinopathy. Curr. Diab. Rep. 17, 82 (2017).
Wang, W. & Lo, A. C. Y. Diabetic retinopathy: pathophysiology and treatments. Int. J. Mol. Sci. 19, 1816 (2018).
Tan, T. E. et al. Global assessment of retinal arteriolar, venular and capillary microcirculations using fundus photographs and optical coherence tomography angiography in diabetic retinopathy. Sci. Rep. 9, 11751 (2019).
Zhu, J. Y., Park, T., Isola, P., Efros A. A. Unpaired image-to-image translation using cycle-consistent adversarial network. arXiv https://doi.org/10.48550/arXiv.1703.10593 (2017).
Obukhov, A., Krasnyanskiy, M. Quality assessment method for GAN based on modified metrics inception score and Fréchet inception distance. In Computational Methods in Systems and Software 2020 (eds. Silhavy, R., Silhavy, P., Prokopova, Z.) 1294 (Springer, Cham, 2020).
Zhou, Y. et al. A refined equilibrium generative adversarial network for retinal vessel segmentation. Neurocomputing 437, 118–130 (2021).
Son, J., Park, S. J. & Jung, K. H. Towards accurate segmentation of retinal vessels and the optic disc in fundoscopic images with generative adversarial networks. J. Digit. Imaging 32, 499–512 (2019).
Cohen, J. P., Luck, M., Honari, S. Distribution matching losses can hallucinate features in medical image translation. In Medical Image Computing and Computer Assisted Intervention—MICCAI 2018 (eds. Frangi, A., Schnabel, J., Davatzikos, C., Alberola-López, C., Fichtinger, G.) 11070 (Springer, Cham, 2018).
Sweeney, P. W., Walker-Samuel, S. & Shipley, R. J. Insights into cerebral haemodynamics and oxygenation utilising in vivo mural cell imaging and mathematical modelling. Sci. Rep. 8, 1373 (2018).
Wong, T. Y. et al. Retinal vessel diameters and their associations with age and blood pressure. Invest. Ophthalmol. Vis. Sci. 44, 4644–4650 (2003).
Yeung, L. et al. Early retinal microvascular abnormalities in patients with chronic kidney disease. Microcirculation 26, e12555 (2019).
Galdran, A. et al. State-of-the-art retinal vessel segmentation with minimalistic models. Sci. Rep. 12, 6174 (2022).
Shin, S. Y. et al. Deep vessel segmentation by learning graphical connectivity. Med. Image. Anal. 58, 101556 (2019).
Garhofer, G. et al. Retinal blood flow in healthy young subjects. Invest. Ophthalmol. Vis. Sci. 53, 698–703 (2012).
Simonwalkersamuel, E. B. & Guy A. Simonwalkersamuel/retinasim: RetinaSim v1.0.0 (v1.0.0). https://github.com/simonwalkersamuel/retinasim (2024).
Schwen, L. O. & Preusser, T. Analysis and algorithmic generation of hepatic vascular systems. Int. J. Hepatol. 2012, 357687 (2012).
Brown, J. H., G. B. West & B. J. Enquist, yes, west, brown and enquist’s model of allometric scaling is both mathematically correct and biologically relevant. Funct. Ecol. 19, 735–738 (2005).
Georg, M., Preusser, T. & Hahn, H. K. Global constructive optimization of vascular systems’, all computer science and engineering research. Compt. Sci. Eng. Res. WUCSE-2010-11, 16 (2010).
Runions, A., Lane, B. & Prusinkiewicz, P. Modeling Trees with a Space Colonization Algorithm. http://algorithmicbotany.org/papers/colonization.egwnp2007.large.pdf (2007).
General Assembly of the World Medical. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. J. Am. Coll. Dent. 81, 14–18 (2014).
Accademic Torents. DRIVE: Digital Retinal Images for Vessel Extraction. https://academictorrents.com/details/062dc18f55b086c76c718ac88f98972789b3c04c (2020).
Acknowledgements
This research was funded by Cancer Research UK (C44767/A29458 and C23017/A27935) and EPSRC (EP/W007096/1). Audit number 1078 was used in accessing ophthalmological image data from Moorfields Eye Hospital NHS Foundation Trust. The audit was authorised by Moorfields Clinical Audit team. EB is a part of EPSRC-funded UCL Centre for Doctoral Training in Intelligent, Integrated Imaging in Healthcare (i4health). CW was supported by the Chan Zuckerberg Initiative DAF an advised fund of Silicon Valley Community Foundation (2020-225394). The authors would like to thank Drs Gabriela Grimaldi and Rajna Rasheed for assigning artery-vein status to a subset of retinal photographs (n=5), and Henry Cole, Andrew. Kume, Jinyu Li, Kendra Hilliard, Yiyun Zhang, Jiahao Xu, Shuo Wu who assisted with data pre-processing, labelling and segmentation. We also thank all participants and patients who contributed ophthalmological imaging data.
Author information
Authors and Affiliations
Contributions
E.E.B. contributed conception and design, analysis and interpretation of data, creation of software, and drafting the work. A.A.G. contributed creation of new software used. N.A.H. contributed analysis and interpretation of data. P.S. contributed creation of new software used. L.G. contributed analysis and interpretation of data. H.C. contributed analysis and interpretation of data. C.W. contributed analysis and interpretation of data. AM contributed creation of new software used. R.S. contributed conception and design, acquisition, and substantial revision to draft. R.R. contributed conception and design of work, acquisition of data, interpretation of data, and substantially revising draft. S.W.S. contributed conception and design of work, acquisition, interpretation of data, creation of new software, and substantial revision of draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brown, E.E., Guy, A.A., Holroyd, N.A. et al. Physics-informed deep generative learning for quantitative assessment of the retina. Nat Commun 15, 6859 (2024). https://doi.org/10.1038/s41467-024-50911-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-50911-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.