Abstract
Penile prosthesis implantation continues to represent a reliable solution to address erectile dysfunction when oral medications fail, are not tolerated or are contraindicated, and most typically is associated with excellent satisfaction rates and durable results. Despite the dramatic improvements in the prostheses’ design, in the surgical instruments and techniques over the years, certain categories of patients still pose a significant surgical challenge. The aim of the current review is to provide a quick and useful practical guidance based on our expertise in the identification and management of the difficult penile prosthesis implantation cases. A narrative review design was here preferred to fulfil our purpose. The search strategy included a range of terms, e.g. penile prosthesis, corporal fibrosis, infection, ischaemic priapism, Peyronie’s disease, radical prostatectomy, pelvic surgery. Extensive corporal fibrosis after explantation of an infected device or after prolonged ischaemic priapism may represent the most difficult situations to deal with in penile prosthesis implantation surgery. Penile prosthesis implantation in patients with Peyronie’s disease and in those who previously underwent radical prostatectomy also presents with an increased risk of complications. Experienced surgeons need to be able to recognise promptly and manage urethral perforation, cylinder crossover, tunical perforation and erosion, as these complications are more common when dealing with difficult penile prosthesis implantation cases. Applying penile lengthening techniques and principles can be useful in selected cases to ensure better postoperative satisfaction rates, especially in those patients who have experienced a more significant degree of loss of length preoperatively. High-volume-implanting surgeons should always be involved in complex cases to minimise the risk of complications. A thorough preoperative counselling can set realistic patients’ expectations in this context, further contributing to postoperative satisfaction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Levine LA, Becher EF, Bella AJ, Brant WO, Kohler TS, Martinez-Salamanca JI, et al. Penile prosthesis surgery: current recommendations from the international consultation on sexual medicine. J Sex Med. 2016;13:489–518.
Chierigo F, Capogrosso P, Dehò F, Pozzi E, Schifano N, Belladelli F, et al. Long-Term Follow-Up After Penile Prosthesis Implantation-Survival and Quality of Life Outcomes. J Sex Med. 2019;16:1827–33.
Garaffa G, Ralph DJ. Penile prosthesis implantation in acute and chronic priapism. Sex Med Rev. 2013;1:76–82.
Montgomery BD, Lomas DJ, Ziegelmann MJ, Trost LW. Infection risk of undergoing multiple penile prostheses: an analysis of referred patient surgical histories. Int J Impot Res. 2018;30:147–52. https://doi.org/10.1038/s41443-018-0026-6.
Falcone M, Pucci L, Garaffa G, Cocci A, Gillo A, Capece M, et al. An outcomes analysis of penile prosthesis implantation following radical cystoprostatectomy and urinary diversion: a multicentric retrospective cohort study. Int J Impot Res. 2020;32:126–32.
Falcone M, Preto M, Cocci A, Garaffa G. Strategies and current practices for penile lengthening in severe Peyronie’s disease cases: a systematic review. Int J Impot Res. 2020;32:52–63. https://doi.org/10.1038/s41443-019-0189-9.
Sansalone S, Garaffa G, Djinovic R, Antonini G, Vespasiani G, Ieria FP, et al. Simultaneous total corporal reconstruction and implantation of a penile prosthesis in patients with erectile dysfunction and severe fibrosis of the corpora cavernosa. J Sex Med. 2012;9:1937–44.
Basilius JR, Hotaling JM, Pastuszak AW. Unwinding fibrosis in Peyronie’s disease. J Sex Med. 2020;17:835–7.
Golan R, Patel NA, Sun T, Barbieri CE, Sedrakyan A, Kashanian JA. Impact of pelvic radiation therapy on inflatable penile prosthesis reoperation rates. J Sex Med. 2018;15:1653–8.
Chew KK, Stuckey BGA, Earle CM, Dhaliwal SS, Keogh EJ, Porst H. Penile fibrosis in intracavernosal prostaglandin E1 injection therapy for erectile dysfunction. Int J Impot Res. 1997;9:225–9.
Wilson SK, Simhan J, Gross MS. Cylinder insertion into scarred corporal bodies: prosthetic urology’s most difficult challenge: some suggestions for making the surgery easier. Int J Impot Res. 2020;32:483–94.
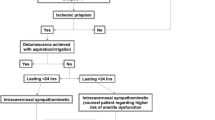
Zacharakis E, Garaffa G, Raheem AA, Christopher AN, Muneer A, Ralph DJ. Penile prosthesis insertion in patients with refractory ischaemic priapism: early vs delayed implantation. BJU Int. 2014;114:576–81.
Wilson SK, Levine L, Wang R. “Make it as long as you can, Doc.” Concomitant surgical treatments with penile implant to enhance penile size. Int J Impot Res. 2021;33:587–95. https://doi.org/10.1038/s41443-020-0306-9.
Tsambarlis PN, Chaus F, Levine LA. Successful placement of penile prostheses in men with severe corporal fibrosis following vacuum therapy protocol. J Sex Med. 2017;14:44–6.
Sellers T, Dineen M, Wilson S. Vacuum protocol and cylinders that lengthen allow implantation of longer inflatable protheses reducing complaints of shortened penile length. J Urol. 2009;181:449.
Sellers T, Dineen M, Salem E, Wilson S. Vacuum Preparation, Optimization of Cylinder Length and Postoperative Daily Inflation Reduces Complaints of Shortened Penile Length Following Implantation of Inflatable Penile Prosthesis. Advances in Sexual Medicine. 2013;3:14–8.
Garber BB, Lim C. Inflatable penile prosthesis insertion in men with severe intracorporal fibrosis. Curr Urol. 2017;10:92–6.
Shaeer O, Shaeer A. Corporoscopic excavation of the fibrosed corpora cavernosa for penile prosethesis implantation: optical corporotomy and trans-corporeal resection, Shaeer’s technique. J Sex Med. 2007;4:218–25.
Andrianne R, Hubert C, Ben MA, Chehida M, Sempels LC, Waltregny D. Use of a wire loop monopolar electrode for open, visual excavation in severe corporeal penile fibrosis before penile prosthesis implantation. VJPU. 2017;2:101.
Wilson SK, Delk JR, Mulcahy JJ, Cleves M, Salem EA. Upsizing of inflatable penile implant cylinders in patients with corporal fibrosis. J Sex Med. 2006;3:736–42.
Ralph DJ. Words of wisdom. Re: upsizing of inflatable penile implant cylinders in patients with corporal fibrosis. Eur Urol. 2007;52:1259.
Lumen N, Monstrey S, Selvaggi G, Ceulemans P, De Cuypere G, Van, et al. Phalloplasty: a valuable treatment for males with penile insufficiency. Urology. 2008;71:272–7.
Lopes EJA, Kuwano AY, Guimaraes AN, Flores JP, Jacobino MAO. Corporoplasty using bovine pericardium grafts in complex penile prosthesis implantation surgery. Int Braz J Urol. 2009;35:45–9.
Palese MA, Burnett AL. Corporoplasty using pericardium allograft (tutoplast) with complex penile prosthesis surgery. Urology. 2001;58:1049–52.
Lentz AC, Carson CC 3rd. Peyronie’s surgery: graft choices and outcomes. Curr Urol Rep. 2009;10:460–7.
Garcia-Gomez B, Ralph D, Levine L, Moncada-Iribarren I, Djinovic R, Albersen M, et al. Grafts for Peyronie’s disease: a comprehensive review. Andrology. 2018;6:117–26.
Wilson SK, Zumbe J, Henry GD, Salem EA, Delk JR, Cleves MA. Infection reduction using antibiotic-coated inflatable penile prosthesis. Urology. 2007;70:337–40.
Katz BF, Gaunay GS, Barazani Y, Nelson CJ, Moreira DM, Dinlenc CZ, et al. Use of a preoperative checklist reduces risk of penile prosthesis infection. J Urol. 2014;192:130–5. https://www.sciencedirect.com/science/article/pii/S0022534713062113.
Köhler TS, Wen L, Wilson SK. Penile implant infection part 3: the changing spectrum of treatment. Int J Impot Res. 2021. https://doi.org/10.1038/s41443-020-00382-8.
Köhler TS, Wen L, Wilson SK. Penile implant infection prevention part 1: what is fact and what is fiction? Wilson’s Workshop #9. Int J Impot Res. 2020;33:785–92.
Habous M, Farag M, Williamson B, Laban O, Mahmoud S, Abdelwahab O, et al. Conservative therapy is an effective option in patients with localized infection after penile implant surgery. J Sex Med. 2016;13:972–6.
Mulcahy JJ. Long-term experience with salvage of infected penile implants. J Urol. 2000;163:481–2.
Caire AA, Boonjindasup A, Hellstrom WJG. Does a replacement or revision of an inflatable penile prosthesis lead to decreased patient satisfaction? Int J Impot Res. 2011;23:39–42.
Chandrapal J, Harper S, Davis LG, Lentz AC. Penile implant infection: experience with expanded salvage criteria and a shortened course of postoperative antibiotics. Sex Med. 2020;8:383–7.
Mulcahy JJ. Management of the infected penile implant–concepts on salvage techniques. Int J Impot Res. 1999;11(Suppl 1):S58–9.
Gross MS, Phillips EA, Balen A, Eid JF, Yang C, Simon R, et al. The malleable implant salvage technique: infection outcomes after mulcahy salvage procedure and replacement of infected inflatable penile prosthesis with malleable prosthesis. J Urol. 2016;195:694–7.
Lao M, Graydon RJ, Bieniek JM. Salvage penile prosthetic surgery utilizing temporary malleable implants. Transl Androl Urol. 2017;6(Suppl 5):S806–12.
Lopategui DM, Balise RR, Bouzoubaa LA, Wilson SK, Kava BR. The impact of immediate salvage surgery on corporeal length preservation in patients presenting with penile implant infections. J Urol. 2018;200:171–7.
Schifano N, Capogrosso P, Boeri L, Fallara G, Cakir OO, Castiglione F, et al. Medications mostly associated with priapism events: assessment of the 2015-2020 Food and Drug Administration (FDA) pharmacovigilance database entries. Int J Impot Res. 2022. https://doi.org/10.1038/s41443-022-00583-3.
Zacharakis E, Raheem AA, Freeman A, Skolarikos A, Garaffa G, Christopher AN, et al. The efficacy of the T-shunt procedure and intracavernous tunneling (snake maneuver) for refractory ischemic priapism. J Urol. 2014;191:164–8.
Ralph DJ, Garaffa G, Muneer A, Freeman A, Rees R, Christopher AN, et al. The immediate insertion of a penile prosthesis for acute ischaemic priapism. Eur Urol. 2009;56:1033–8.
La Croce G, Schifano N, Pescatori E, Caraceni E, Colombo F, Bettocchi C, et al. Which patient may benefit the most from penile prosthesis implantation? Andrology. 2022. https://doi.org/10.1111/andr.13294. Epub ahead of print.
Capogrosso P, Bettocchi C, Colombo F, Liguori G, Fiordelise S, Vitarelli A, et al. PS-7-5 risk of unfavorable outcomes after penile prosthesis implantation—results from a National Registry (INSIST-ED). J Sex Med. 2020;17(Suppl 2):S140. https://www.sciencedirect.com/science/article/pii/S1743609520302824.
El-Khatib FM, Huynh LM, Yafi FA. Intraoperative methods for residual curvature correction during penile prosthesis implantation in patients with Peyronie’s disease and refractory erectile dysfunction. Int J Impot Res. 2020;32:43–51.
Wilson SK, Delk JR 2nd. A new treatment for Peyronie’s disease: modeling the penis over an inflatable penile prosthesis. J Urol. 1994;152:1121–3.
Shabbir M, Muneer A, Minhas S. Surgery for erectile dysfunction. In: Muneer A, editor. Atlas of male genitourethral surgery. John Wiley & Sons, Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK; 2014. p. 71–91.
Bokarica P, Parazajder J, Mazuran B, Gilja I. Surgical treatment of Peyronie’s disease based on penile length and degree of curvature. Int J Impot Res. 2005;17:170–4.
Schifano N, Cakir O, Castiglione F, Montorsi F, Garaffa G. Multidisciplinary approach and management of patients who seek medical advice for penile size concerns: a narrative review. Int J Impot Res. 2021. https://pubmed.ncbi.nlm.nih.gov/34045688/.
Rolle L, Ceruti C, Timpano M, Sedigh O, Destefanis P, Galletto E, et al. A new, innovative, lengthening surgical procedure for Peyronie’s disease by penile prosthesis implantation with double dorsal-ventral patch graft: the “Sliding Technique.” J Sex Med. 2012.
Egydio PH, Kuehhas FE. Penile lengthening and widening without grafting according to a modified “sliding” technique. BJU Int. 2015;116:965–72.
Rolle L, Ceruti C, Timpano M, Sedigh O, Destefanis P, Galletto E, et al. A new, innovative, lengthening surgical procedure for Peyronie’s disease by penile prosthesis implantation with double dorsal-ventral patch graft: the “sliding technique”. J Sex Med. 2012;9:2389–95.
Garaffa G, Capece M, Chiriaco G, Ralph DJ. Peyronie’s disease: tunical string-vest incisions for girth and length restoration after penile prosthesis implantation. VJPU. 2018;2:140. https://www.vjpu-issm.info/videos/peer-reviewed/1-penile-prosthesis-malleable-inflatable-penile-prosthesis-ipp/1-a-first-time-implant/1-a-e-lengthening-procedures/item/141-peyronie-s-disease-tunical-string-vest-incisions-for-girth-and-length-restoration-a.
Hatzichristodoulou G. The PICS technique: a novel approach for residual curvature correction during penile prosthesis implantation in patients with severe Peyronie’s disease using the Collagen Fleece TachoSil. J Sex Med. 2018;15:416–21.
Miranda A. Auxetic expansion of the Tunica Albuginea for penile length and girth restoration without a graft: a translational study. Sex Med. 2021;9:100456.
Megas G, Papadopoulos G, Stathouros G, Moschonas D, Gkialas I, Ntoumas K. Comparison of efficacy and satisfaction profile, between penile prosthesis implantation and oral PDE5 inhibitor tadalafil therapy, in men with nerve-sparing radical prostatectomy erectile dysfunction. BJU Int. 2013;112:E169–76.
Schifano N, Capogrosso P, Tutolo M, Dehò F, Montorsi F, Salonia A. How to Prevent and Manage Post-Prostatectomy Incontinence: A Review. World J Mens Health. 2021;39:581–97.
Hakky TS, Baumgarten AS, Parker J, Zheng Y, Kongnyuy M, Martinez D, et al. Penile rehabilitation: the evolutionary concept in the management of erectile dysfunction. Curr Urol Rep. 2014;15:393.
Tal R, Heck M, Teloken P, Siegrist T, Nelson CJ, Mulhall JP. Peyronie’s disease following radical prostatectomy: incidence and predictors. J Sex Med. 2010;7:1254–61.
Wilson SK, Simhan J, Osmonov D. Should occasional implanters learn ectopic placement of IPP reservoirs? Int J Impot Res. 2020;32:371–8.
Garaffa G, Ralph DJ. Ectopic reservoir during inflatable penile implant surgery: is it now standard of care? J Sex Med. 2017;14:316–7.
Minhas S. Urethral perforation during penile implant surgery: what to do? J Sex Med. 2017;14:867–9.
Wilson SK, Simhan J, Carrion R. Inflatable penile prosthesis cylinders out of place during implantation. Int J Impot Res. 2020;32:598–605. https://doi.org/10.1038/s41443-020-0293-x.
Bettocchi C, Ditonno P, Palumbo F, Lucarelli G, Garaffa G, Giammusso B, et al. Penile prosthesis: what should we do about complications? Adv Urol. 2008;2008:573560.
Karpman E. Management of distal & proximal penile prosthesis crossover. J Sex Med. 2016;13:1008–12.
Levine LA, Rybak J. Traction therapy for men with shortened penis prior to penile prosthesis implantation: a pilot study. J Sex Med. 2011;8:2112–7.
Moskovic DJ, Pastuszak AW, Lipshultz LI, Khera M. Revision of penile prosthesis surgery after use of penile traction therapy to increase erect penile length: case report and review of the literature. J Sex Med. 2011;8:607–11.
Schifano N, Castiglione F, Cakir OO, Montorsi F, Garaffa G. Reconstructive surgery of the scrotum: a systematic review. Int J Impot Res. 2022;34:359–68.
Garaffa G, Sansalone S, Ralph DJ. Augmentation procedures for the penis. In: Muneer A, editor. Atlas of male genitourethral surgery. John Wiley & Sons, Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK; 2014. p. 71–91.
Miranda-Sousa A, Keating M, Moreira S, Baker M, Carrion R. Concomitant ventral phalloplasty during penile implant surgery: a novel procedure that optimizes patient satisfaction and their perception of phallic length after penile implant surgery. J Sex Med. 2007;4:1494–9.
Gupta NK, Sulaver R, Welliver C, Kottwitz M, Frederick L, Dynda D, et al. Scrotoplasty at time of penile implant is at high risk for dehiscence in diabetics. J Sex Med. 2019;16:602–8.
Montague DK, Angermeier KW. Corporeal excavation: new technique for penile prosthesis implantation in men with severe corporeal fibrosis. Urology. 2006;67:1072–5.
Caso J, Keating M, Miranda-Sousa A, Carrion R. Ventral phalloplasty. Asian J Androl. 2008;10:155–7.
Author information
Authors and Affiliations
Contributions
Conception of the work: NS and GG; Data collection: NS, PC and OOC; Data analysis and interpretation: NS, PC and OOC; Drafting the article: NS and OOC; Critical revision of the article: PC, FD and GG; Final approval of the version to be published: NS, PC, OOC, FD and GG.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schifano, N., Capogrosso, P., Cakir, O.O. et al. Surgical tips in difficult penile prosthetic surgery: a narrative review. Int J Impot Res 35, 690–698 (2023). https://doi.org/10.1038/s41443-022-00629-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-022-00629-6