Abstract
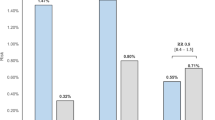
With the promising cardiovascular benefits in the STEP and SPRINT trials, the 2022 Taiwan’s hypertension guidelines redefined the hypertension threshold as 130/80 mmHg and a universal blood-pressure target of <130/80 mmHg. This study’s objective was to examine the cost-effectiveness of the intensive blood-pressure target for hypertensive patients using estimated lifetime medical costs and quality-adjusted life years (QALY) from the Taiwan national payer’s perspective. We developed a lifetime Markov model comparing the intensive and conservative blood-pressure targets. Incremental cost-effectiveness ratio (ICER) against the willing-to-pay thresholds at the one-time [US$34,000(NT$1,020,000)] and three-time [US$100,000(NT$3,000,000)] gross domestic product per capita were defined as very cost-effect and only cost-effective. The cost-effectiveness in different age stratifications and cardiovascular risks treated with a more intensive target (120 mmHg) were examined in the subgroup analyses. The new blood-pressure treatment target produced more lifetime medical costs [US$31,589(NT$947,670) versus US$26,788(NT$803,640)] and QALYs (12.54 versus 12.25), and the ICER was US$16,589(NT$497,670), which was 99.1% and 100% probability of a very cost-effective and cost-effective strategy. The ICERs in all age stratifications had more than a 90% probability of being very cost-effective, and ICERs decreased with age. More intensive control in patients with high cardiovascular risks produced a lower ICER [US$14,547(NT$436,410)]. In conclusion, Taiwan’s new blood-pressure treatment target can prevent more cardiovascular events with acceptable costs per QALY below the willing-to-pay thresholds. The cost-effectiveness of intensive control is consistent across different ages and more pronounced with the increase in age and cardiovascular risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;11:507–20.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American heart association task force on clinical practice guidelines. Circulation. 2018;138:e426–83.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67.
SPRINT Research Group, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N. Engl J Med. 2015;373:2103–16.
Douros A, Tölle M, Ebert N, Gaedeke J, Huscher D, Kreutz R, et al. Control of blood pressure and risk of mortality in a cohort of older adults: the Berlin Initiative Study. Eur Heart J. 2019;40:2021–8.
Zhang W, Zhang S, Deng Y, Wu S, Ren J, Sun G, et al. Trial of intensive blood-pressure control in older patients with hypertension. N. Engl J Med. 2021;385:1268–79.
Wang TD, Chiang CE, Chao TH, Cheng HM, Wu YW, Wu YJ, et al. 2022 Guidelines of the Taiwan society of cardiology and the Taiwan hypertension society for the management of hypertension. Acta Cardiol Sin. 2022;38:225–325.
Bress AP, Bellows BK, King JB, Hess R, Beddhu S, Zhang Z, et al. Cost-effectiveness of intensive versus standard blood-pressure control. N. Engl J Med. 2017;377:745–55.
Richman IB, Fairley M, Jørgensen ME, Schuler A, Owens DK, Goldhaber-Fiebert JD. Cost-effectiveness of intensive blood pressure management. JAMA Cardiol. 2016;1:872–9.
Health Technology Assessment of Center for Drug Evaluation, Taiwan. Taiwan guidelines of methodological standards for pharmacoeconomic evaluation. Accessed on May 3, 2022 from https://www.cde.org.tw/HTA/history.
SCORE2 working group and ESC Cardiovascular risk collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42:2439–54.
SCORE2-OP working group and ESC Cardiovascular risk collaboration, SCORE2-OP risk prediction algorithms: estimating incident cardiovascular event risk in older persons in four geographical risk regions. Eur Heart J. 2021;42:2455–67
Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S49–73.
Chien KL, Hsu HC, Su TC, Chang WT, Chen PC, Sung FC, et al. Constructing a point-based prediction model for the risk of coronary artery disease in a Chinese community: a report from a cohort study in Taiwan. Int J Cardiol. 2012;157:263–8.
Ministry of the Interior. Republic of China (Taiwan), Life Tables. Accessed on April 3, 2022. https://www.moi.gov.tw/english/cl.aspx?n=7779.
Burnier M, Egan BM. Adherence in hypertension. Circ Res. 2019;124:1124–40.
Iskedjian M, Einarson TR, MacKeigan LD, Shear N, Addis A, Mittmann N, et al. Relationship between daily dose frequency and adherence to antihypertensive pharmacotherapy: evidence from a meta-analysis. Clin Ther. 2002;24:302–16.
Bank of Taiwan. Accessed on June 1, 2022. https://rate.bot.com.tw/xrt?Lang=zh-TW.
International Monetary Fund. World Economic Outlook Database, April 2022. Accessed on 19 May 2022. https://www.imf.org/en/Home.
Bertram MY, Lauer JA, De Joncheere K, Edejer T, Hutubessy R, Kieny MP, et al. Cost–effectiveness thresholds: pros and cons. Bull World Health Organ. 2016;94:925.
Briggs AH. Handling uncertainty in cost-effectiveness models. Pharmacoeconomics. 2000;17:479–500.
Taiwan Ministry of Health and Welfare. Cause of Death Statistics. https://www.mohw.gov.tw/np-128-2.html. Accessed 30 May 2019.
Chia YC, Buranakitjaroen P, Chen CH, Divinagracia R, Hoshide S, Park S, et al. Current status of home blood pressure monitoring in Asia: Statement from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2017;19:1192–201.
Cheng HM, Lin HJ, Wang TD, Chen CH. Asian management of hypertension: Current status, home blood pressure, and specific concerns in Taiwan. J Clin Hypertens (Greenwich). 2020;22:511–4.
Taiwan Health Promotion Administration MoHaW. National Health Interview Survey. https://www.hpa.gov.tw/. Accessed on June, 2022.
Liao CT, Yang CT, Kuo FH, Lee MC, Chang WT, Tang HJ, et al. Cost-effectiveness evaluation of add-on empagliflozin in patients with heart failure and a reduced ejection fraction from the healthcare system’s perspective in the Asia-Pacific region. Front Cardiovasc Med. 2021;8:750381.
Liao CT, Yang CT, Toh HS, Chang WT, Chang HY, Kuo FH, et al. Cost-effectiveness evaluation of add-on dapagliflozin for heart failure with reduced ejection fraction from perspective of healthcare systems in Asia-Pacific region. Cardiovasc Diabetol. 2021;20:204.
Lee MC, Liao CT, Toh HS, Chou CC, Chang WT, Chen ZC, et al. Cost-effectiveness analysis of rivaroxaban plus aspirin versus aspirin alone in secondary prevention among patients with chronic cardiovascular diseases. Cardiovasc Drugs Ther. 2021;35:539–47.
Liao CT, Lee MC, Chen ZC, Ku LE, Wang JD, Toh HS. Cost-effectiveness analysis of oral anticoagulants in stroke prevention among patients with atrial fibrillation in Taiwan. Acta Cardiol Sin. 2020;36:50–61.
Li C, Chen K, Cornelius V, Tomeny E, Wang Y, Yang X, et al. Applicability and cost-effectiveness of the Systolic Blood Pressure Intervention Trial (SPRINT) in the Chinese population: A cost-effectiveness modeling study. PLoS Med. 2021;18:e1003515.
Lin SF, Kuo TT, Pan WH, Bai CH. Effects of socioeconomic status on the control of hypertension in patients <65 and ≥65 years of age in Taiwan: a nationwide cross-sectional study. BMJ Open. 2022;12:e050041.
Acknowledgements
CTL drafted the manuscript. CTL, HST, CTY and CYH contributed to this study, including the conception and design of the research. CTL, WTC and HYC contributed to this study’s data extraction, analyses, and interpretation of data. This manuscript was revised by HST, WTC, ZCC, and CS. All authors gave final approval and agree to all aspects of the work, ensuring integrity and accuracy. We appreciated the supports of Professor Zhen-Yu Zhang, Dongmei Wei and Jesus Melgarejo from KU Leuven.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: this project was supported by a grant to Chia-Te Liao from the Ministry of Science and Technology in Taiwan (MOST 111–2917-I-006–007 and MOST 111–2314-B-384-003), and Chi Mei Medical Center (CMHCR11003).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liao, CT., Toh, H.S., Yang, CT. et al. Economic evaluation of new blood pressure target for hypertensive patients in Taiwan according to the 2022 hypertension clinical practice guidelines of the Taiwan society of cardiology: a simulation modeling study. Hypertens Res 46, 187–199 (2023). https://doi.org/10.1038/s41440-022-01037-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-01037-5
Keyword
This article is cited by
-
Economic evaluation of a new blood pressure target for hypertensive patients in Taiwan
Hypertension Research (2023)