Abstract
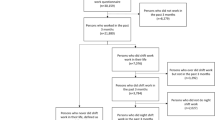
This study aimed to examine the association between rotating night shift work and carotid atherosclerosis in Chinese steelworkers. A total of 3582 subjects were included in this study. Different exposure metrics of night shifts, including current shift status, duration of night shifts (years), the cumulative number of night shifts (nights), cumulative length of night shifts (hours) and average frequency of night shifts (nights/month), were used to examine the relationship between night shift work and carotid atherosclerosis, including carotid plaque and carotid plaque scores. The prevalence of carotid plaque was 29.9% in the study population. Compared with day workers, significantly increased odds of carotid plaque were observed among shift workers in each quartile of the duration of night shifts after adjusting for potential confounders, especially in the third and fourth quartiles: odds ratio (OR) = 1.91, 95% confidence interval (CI): 1.46 to 2.49, in the third quartiles; OR = 1.69, 95% CI: 1.30 to 2.20, in the fourth quartiles. Positive associations of different exposure metrics of night shifts (continuous) with the odds of carotid plaque and the carotid plaque score were observed in the restricted cubic spline (RCS) models. No significant association was found in female workers between night shift work and carotid plaque. Rotating night shift work is associated with elevated odds of carotid atherosclerosis in male steelworkers.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Change history
14 November 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41440-022-01078-w
References
Puttonen S, Härmä M, Hublin C. Shift work and cardiovascular disease—pathways from circadian stress to morbidity. Scand J Work, Environ Health. 2010;36:96–108.
Humans IWGotEoCRt. Painting, firefighting, and shiftwork. IARC monographs on the evaluation of carcinogenic risks to humans 2010;98:9.
Puttonen S, Kivimäki M, Elovainio M, Pulkki-Råback L, Hintsanen M, Vahtera J, et al. Shift work in young adults and carotid artery intima-media thickness: the cardiovascular risk in young Finns study. Atherosclerosis. 2009;205:608–13.
group IMV. Carcinogenicity of night shift work. Lancet Oncol. 2019;20:1058–9.
Collaborators GCoD: Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1151–210.
Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16:203–12.
Knutsson A, Akerstedt T, Jonsson BG, Orth-Gomer K. Increased risk of ischaemic heart disease in shift workers. Lancet. 1986;2:89–92.
Bøggild H, Knutsson A. Shift work, risk factors and cardiovascular disease. Scand J Work, Environ Health. 1999;25:85–99.
Frost P, Kolstad HA, Bonde JP. Shift work and the risk of ischemic heart disease—a systematic review of the epidemiologic evidence. Scand J Work, Environ Health. 2009;35:163–79.
Vyas MV, Garg AX, Iansavichus AV, Costella J, Donner A, Laugsand LE, et al. Shift work and vascular events: systematic review and meta-analysis. BMJ. 2012;345:e4800.
Torquati L, Mielke GI, Brown WJ, Kolbe-Alexander T. Shift work and the risk of cardiovascular disease. A systematic review and meta-analysis including dose-response relationship. Scand J Work, Environ Health. 2018;44:229–38.
Scheer FAJL, Hilton MF, Mantzoros CS, Shea SA:. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci USA. 2009;106:4453–8.
Zhu Z, Hua B, Shang Z, Yuan G, Xu L, Li E, et al. Altered clock and lipid metabolism-related genes in atherosclerotic mice kept with abnormal lighting condition. BioMed Res Int. 2016;2016:5438589.
Figueiro MG, Goo Y-H, Hogan R, Plitnick B, Lee J-K, Jahangir K, et al. Light-dark patterns mirroring shift work accelerate atherosclerosis and promote vulnerable lesion phenotypes. J Am Heart Assoc. 2021;10:e018151.
Jankowiak S, Backé E, Liebers F, Schulz A, Hegewald J, Garthus-Niegel S, et al. Current and cumulative night shift work and subclinical atherosclerosis: results of the Gutenberg Health Study. Int Arch Occup Environ Health. 2016;89:1169–82.
Laclaustra M, Casasnovas JA, Fernández-Ortiz A, Fuster V, León-Latre M, Jiménez-Borreguero LJ, et al. Femoral and carotid subclinical atherosclerosis association with risk factors and coronary calcium: the AWHS study. J Am Coll Cardiol. 2016;67:1263–74.
Spence JD. Carotid plaque measurement is superior to IMT Invited editorial comment on: carotid plaque, compared with carotid intima-media thickness, more accurately predicts coronary artery disease events: a meta-analysis-Yoichi Inaba, M.D., Jennifer A. Chen M.D., Steven R. Bergmann M.D., Ph.D. Atherosclerosis. 2012;220:34–35.
Gepner AD, Young R, Delaney JA, Budoff MJ, Polak JF, Blaha MJ et al. Comparison of carotid plaque score and coronary artery calcium score for predicting cardiovascular disease events: the multi-ethnic study of atherosclerosis. J Am Heart Assoc. 2017;6:e005179.
Hirata T, Arai Y, Takayama M, Abe Y, Ohkuma K, Takebayashi T. Carotid plaque score and risk of cardiovascular mortality in the oldest old: results from the TOOTH study. J Atherosclerosis Thrombosis. 2018;25:55–64.
Sillesen H, Sartori S, Sandholt B, Baber U, Mehran R, Fuster V. Carotid plaque thickness and carotid plaque burden predict future cardiovascular events in asymptomatic adult Americans. Eur Heart J Cardiovascular Imaging. 2018;19:1042–50.
Polak JF, Szklo M, Kronmal RA, Burke GL, Shea S, Zavodni AEH, et al. The value of carotid artery plaque and intima-media thickness for incident cardiovascular disease: the multi-ethnic study of atherosclerosis. J Am Heart Assoc. 2013;2:e000087.
McAlpine CS, Swirski FK. Circadian influence on metabolism and inflammation in atherosclerosis. Circulation Res. 2016;119:131–41.
Hall AL, Franche R-L, Koehoorn M. Examining exposure assessment in shift work research: a study on depression among nurses. Ann Work Exposures Health. 2018;62:182–94.
Touboul P-J, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, et al. Mannheim carotid intima-media thickness and plaque consensus (2004-2006-2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc Dis. 2012;34:290–6.
Crouse JR, Harpold GH, Kahl FR, Toole JF, McKinney WM. Evaluation of a scoring system for extracranial carotid atherosclerosis extent with B-mode ultrasound. Stroke. 1986;17:270–5.
Zhang S, Wang Y, Wang Z, Wang H, Xue C, Li Q, et al. Rotating night shift work and non-alcoholic fatty liver disease among steelworkers in China: a cross-sectional survey. Occup Environ Med. 2020;77:333–9.
Wang A, Arah OA, Kauhanen J, Krause N. Work schedules and 11-year progression of carotid atherosclerosis in middle-aged Finnish men. Am J Ind Med. 2015;58:1–13.
Silva-Costa A, Guimarães J, Chor D, Fonseca MDJMD, Bensenor I, Santos I, et al. Time of exposure to night work and carotid atherosclerosis: a structural equation modeling approach using baseline data from ELSA-Brasil. Int Arch Occup Environ Health. 2018;91:591–600.
Rizza S, Longo S, Piciucchi G, Romanello D, Mavilio M, Montagna M, et al. Carotid intimal medial thickness in rotating night shift is related to IL1β/IL6 axis. Nutr, Metab, Cardiovascular Dis: NMCD. 2020;30:1826–32.
Sugiura T, Dohi Y, Takagi Y, Yoshikane N, Ito M, Suzuki K, et al. Impacts of lifestyle behavior and shift work on visceral fat accumulation and the presence of atherosclerosis in middle-aged male workers. Hypertension Res: Off J Jpn Soc Hypertension. 2020;43:235–45.
Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115:459–67.
Inaba Y, Chen JA, Bergmann SR. Carotid plaque, compared with carotid intima-media thickness, more accurately predicts coronary artery disease events: a meta-analysis. Atherosclerosis. 2012;220:128–33.
Fernández-Friera L, Peñalvo JL, Fernández-Ortiz A, Ibañez B, López-Melgar B, Laclaustra M, et al. Prevalence, vascular distribution, and multiterritorial extent of subclinical atherosclerosis in a middle-aged cohort: the PESA (progression of early subclinical atherosclerosis) study. Circulation. 2015;131:2104–13.
Peñalvo JL, Mertens E, Muñoz-Cabrejas A, León-Latre M, Jarauta E, Laclaustra M et al. Work shift, lifestyle factors, and subclinical atherosclerosis in Spanish male workers: a mediation analysis. Nutrients. 2021;13:1077.
Knutsson A, Bøggild H. Shiftwork and cardiovascular disease: review of disease mechanisms. Rev Environ Health. 2000;15:359–72.
Thomas C, Power C. Shift work and risk factors for cardiovascular disease: a study at age 45 years in the 1958 British birth cohort. Eur J Epidemiol. 2010;25:305–14.
Roskoden FC, Krüger J, Vogt LJ, Gärtner S, Hannich HJ, Steveling A, et al. Physical activity, energy expenditure, nutritional habits, quality of sleep and stress levels in shift-working health care personnel. PloS One. 2017;12:e0169983.
Lechner K, Schacky CV, McKenzie AL, Worm N, Nixdorff U, Lechner B, et al. Lifestyle factors and high-risk atherosclerosis: pathways and mechanisms beyond traditional risk factors. Eur J Preventive Cardiol. 2020;27:394–406.
Schwartz BG, French WJ, Mayeda GS, Burstein S, Economides C, Bhandari AK, et al. Emotional stressors trigger cardiovascular events. Int J Clin Pract. 2012;66:631–9.
Leng B, Jin Y, Li G, Chen L, Jin N. Socioeconomic status and hypertension: a meta-analysis. J Hypertension. 2015;33:221–9.
Cha SH, Park HS, Cho HJ. Socioeconomic disparities in prevalence, treatment, and control of hypertension in middle-aged Koreans. J Epidemiol. 2012;22:425–32.
Wolk R, Gami AS, Garcia-Touchard A, Somers VK. Sleep and cardiovascular disease. Curr Probl Cardiol. 2005;30:625–62.
Pagano ES, Spinedi E, Gagliardino JJ. White adipose tissue and circadian rhythm dysfunctions in obesity: pathogenesis and available therapies. Neuroendocrinology. 2017;104:347–63.
Archer E, Pavela G, Lavie CJ. The inadmissibility of what we eat in America and NHANES dietary data in nutrition and obesity research and the scientific formulation of national dietary guidelines. Mayo Clin Proc. 2015;90:911–26.
Wang C, Bangdiwala SI, Rangarajan S, Lear SA, AlHabib KF, Mohan V, et al. Association of estimated sleep duration and naps with mortality and cardiovascular events: a study of 116 632 people from 21 countries. Eur Heart J. 2019;40:1620–9.
Cain SW, Filtness AJ, Phillips CL, Anderson C. Enhanced preference for high-fat foods following a simulated night shift. Scand J Work, Environ Health. 2015;41:288–93.
Lowden A, Moreno C, Holmbäck U, Lennernäs M, Tucker P. Eating and shift work—effects on habits, metabolism and performance. Scand J Work, Environ Health. 2010;36:150–62.
Amani R, Gill T. Shiftworking, nutrition and obesity: implications for workforce health- a systematic review. Asia Pac J Clin Nutr. 2013;22:505–15.
Bonham MP, Bonnell EK, Huggins CE. Energy intake of shift workers compared to fixed day workers: a systematic review and meta-analysis. Chronobiol Int. 2016;33:1086–100.
Melkani GC, Panda S. Time-restricted feeding for prevention and treatment of cardiometabolic disorders. J Physiol. 2017;595:3691–700.
Crupi AN, Haase J, Brandhorst S, Longo VD. Periodic and intermittent fasting in diabetes and cardiovascular disease. Curr Diabetes Rep. 2020;20:83.
Acknowledgements
The authors would like to acknowledge all the participants and institutions involved in the collection of the baseline data.
Funding
This work was supported by the National Key R&D Program of China: Grant number 2016YFC0900605.
Author information
Authors and Affiliations
Contributions
LW created the study concept and drafted the manuscript; SZ conceived and designed this work; MY analyzed the data and performed revisions; and JY supervised the fieldwork of this project. All authors agreed to submit this article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, L., Zhang, S., Yu, M. et al. Association between rotating night shift work and carotid atherosclerosis among Chinese steelworkers: a cross-sectional survey. Hypertens Res 45, 686–697 (2022). https://doi.org/10.1038/s41440-021-00821-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-021-00821-z