Abstract
Background
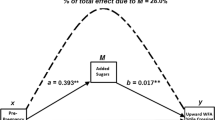
Higher maternal preconception body mass index (BMI) is associated with lower breastfeeding duration, which may contribute to the development of poor child eating behaviours and dietary intake patterns (components of nutritional risk). A higher maternal preconception BMI has been found to be associated with higher child nutritional risk. This study aimed to determine whether breastfeeding duration mediated the association between maternal preconception BMI and child nutritional risk.
Methods
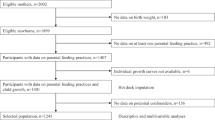
In this longitudinal cohort study, children ages 18 months to 5 years were recruited from The Applied Research Group for Kids (TARGet Kids!) in Canada. The primary outcome was child nutritional risk, using The NutriSTEP®, a validated, parent-reported questionnaire. Statistical mediation analysis was performed to assess whether total duration of any breastfeeding mediated the association between maternal preconception BMI and child nutritional risk.
Results
This study included 4733 children with 8611 NutriSTEP® observations. The mean (SD) maternal preconception BMI was 23.6 (4.4) and the mean (SD) breastfeeding duration was 12.4 (8.0) months. Each 1-unit higher maternal preconception BMI was associated with a 0.081 unit higher nutritional risk (95% CI (0.051, 0.112); p < 0.001) (total effect), where 0.011(95% CI (0.006, 0.016); p < 0.001) of that total effect or 13.18% (95% CI: 7.13, 21.25) was mediated through breastfeeding duration.
Conclusion
Total breastfeeding duration showed to mediate part of the association between maternal preconception BMI and child nutritional risk. Interventions to support breastfeeding in those with higher maternal preconception BMI should be evaluated for their potential effect in reducing nutritional risk in young children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data described in the manuscript, code book, and analytic code will be made available upon request pending application and approval.
References
Flores TR, Mielke GI, Wendt A, Nunes BP, Bertoldi AD. Prepregnancy weight excess and cessation of exclusive breastfeeding: a systematic review and meta-analysis. Eur J Clin Nutr. 2018;72:480–8.
Hashemi-Nazari SS, Hasani J, Izadi N, Najafi F, Rahmani J, Naseri P, et al. The effect of pre-pregnancy body mass index on breastfeeding initiation, intention and duration: a systematic review and dose-response meta-analysis. Heliyon. 2020;6:e05622.
Wojcicki JM. Maternal prepregnancy body mass index and initiation and duration of breastfeeding: a review of the literature. J Women’s Health. 2011;20:341–7.
Huang Y, Ouyang YQ, Redding SR. Maternal prepregnancy body mass index, gestational weight gain, and cessation of breastfeeding: a systematic review and meta-analysis. Breastfeed Med J Acad Breastfeed Med. 2019;14:366–74.
Kim TJ, von dem Knesebeck O. Income and obesity: what is the direction of the relationship? A systematic review and meta-analysis. BMJ Open. 2018;8:e019862.
Ryan AS, Zhou W. Lower breastfeeding rates persist among the special supplemental nutrition program for women, infants, and children participants, 1978–2003. Pediatrics. 2006;117:1136–46.
Temple Newhook J, Newhook LA, Midodzi WK, Murphy Goodridge J, Burrage L, Gill N, et al. Poverty and breastfeeding: comparing determinants of early breastfeeding cessation incidence in socioeconomically marginalized and privileged populations in the FiNaL study. Health Equity. 2017;1:96–102.
De Cosmi V, Scaglioni S, Agostoni C. Early taste experiences and later food choices. Nutrients. 2017;9:E107.
Scaglioni S, De Cosmi V, Ciappolino V, Parazzini F, Brambilla P, Agostoni C. Factors influencing children’s eating behaviours. Nutrients. 2018;10:E706.
Burnier D, Dubois L, Girard M. Exclusive breastfeeding duration and later intake of vegetables in preschool children. Eur J Clin Nutr. 2011;65:196–202.
Ventura AK. Does breastfeeding shape food preferences? links to obesity. Ann Nutr Metab. 2017;70:8–15.
Rogers SL, Blissett J. Breastfeeding duration and its relation to weight gain, eating behaviours and positive maternal feeding practices in infancy. Appetite. 2017;108:399–406.
Borkhoff CM, Dai DWH, Jairam JA, Wong PD, Cox KA, Maguire JL, et al. Breastfeeding to 12 mo and beyond: nutrition outcomes at 3 to 5 y of age. Am J Clin Nutr. 2018;108:354–62.
Perrine CG, Galuska DA, Thompson FE, Scanlon KS. Breastfeeding duration is associated with child diet at 6 years. Pediatrics. 2014;134:S50–55.
Soldateli B, Vigo A, Giugliani ERJ. Effect of pattern and duration of breastfeeding on the consumption of fruits and vegetables among preschool children. PLOS ONE. 2016;11:e0148357.
Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC. Tracking of obesity-related behaviours from childhood to adulthood: a systematic review. Maturitas. 2011;70:266–84.
Kim J, Lim H. Nutritional management in childhood obesity. J Obes Metab Syndr. 2019;28:225–35.
Birch L, Savage JS, Ventura A. Influences on the development of children’s eating behaviours: from infancy to adolescence. Can J Diet Pr Res. 2007;68:s1–56.
Haycraft E, Karasouli E, Meyer C. Maternal feeding practices and children’s eating behaviours: a comparison of mothers with healthy weight versus overweight/obesity. Appetite. 2017;116:395–400.
Andersen LBB, Pipper CB, Trolle E, Bro R, Larnkjær A, Carlsen EM, et al. Maternal obesity and offspring dietary patterns at 9 months of age. Eur J Clin Nutr. 2015;69:668–75.
Fisk CM, Crozier SR, Inskip HM, Godfrey KM, Cooper C, Robinson SM, et al. Influences on the quality of young children’s diets: the importance of maternal food choices. Br J Nutr. 2011;105:287–96.
Kiefte-de Jong JC, de Vries JH, Bleeker SE, Jaddoe VW, Hofman A, Raat H, et al. Socio-demographic and lifestyle determinants of ‘Western-like’ and ‘Health conscious’ dietary patterns in toddlers. Br J Nutr. 2013;109:137–47.
Braddon KE, Keown-Stoneman CD, Dennis CL, Li X, Maguire JL, O’Connor DL, et al. Maternal Preconception body mass index and early childhood nutritional risk. J Nutr. 2023;153:2421–31.
Carsley S, Borkhoff CM, Maguire JL, Birken CS, Khovratovich M, McCrindle B, et al. Cohort profile: the applied research group for kids (TARGet Kids!). Int J Epidemiol. 2015;44:776–88.
World Health Organization. WHO child growth standards: training course on child growth assessment [Internet]. World Health Organization; 2008. Available from: https://apps.who.int/iris/handle/10665/43601
Randall Simpson JA, Keller HH, Rysdale LA, Beyers JE. Nutrition screening tool for every preschooler (NutriSTEPTM): validation and test–retest reliability of a parent-administered questionnaire assessing nutrition risk of preschoolers. Eur J Clin Nutr. 2008;62:770–80.
Randall Simpson J, Gumbley J, Whyte K, Lac J, Morra C, Rysdale L, et al. Development, reliability, and validity testing of Toddler NutriSTEP: a nutrition risk screening questionnaire for children 18-35 months of age. Appl Physiol Nutr Metab Physiol Appl Nutr Metab. 2015;40:877–86.
Omand J, Janus M, Maguire J, Parkin P, Aglipay M, Simpson J, et al. Nutritional risk in early childhood and school readiness. J Nutr. 2021;151:3811–9.
VanderWeele TJ. Mediation analysis: a practitioner’s guide. Annu Rev Public Health. 2016;37:17–32.
VanderWeele T. Explanation in causal inference: methods for mediation and interaction. New York: Oxford University Press; 2015. p. 729.
French SA, Tangney CC, Crane MM, Wang Y, Appelhans BM. Nutrition quality of food purchases varies by household income: the SHoPPER study. BMC Public Health. 2019;19:231.
Roustaei Z, Räisänen S, Gissler M, Heinonen S. Socioeconomic differences in the association between maternal age and maternal obesity: a register-based study of 707,728 women in Finland. Scand J Public Health. 2022;51:963–71.
Wemakor A, Garti H, Azongo T, Garti H, Atosona A. Young maternal age is a risk factor for child undernutrition in Tamale Metropolis, Ghana. BMC Res Notes. 2018;11:877.
Shai I, Jiang R, Manson JE, Stampfer MJ, Willett WC, Colditz GA, et al. Ethnicity, obesity, and risk of type 2 diabetes in women: a 20-year follow-up study. Diabetes Care. 2006;29:1585–90.
de Hoog MLA, Kleinman KP, Gillman MW, Vrijkotte TGM, van Eijsden M, Taveras EM. Racial/ethnic and immigrant differences in early childhood diet quality. Public Health Nutr. 2014;17:1308–17.
Ugwuja EI, Nnabu RC, Ezeonu PO, Uro-Chukwu H. The effect of parity on maternal body mass index, plasma mineral element status and new-born anthropometrics. Afr Health Sci. 2015;15:986–92.
Potter C, Gibson EL, Ferriday D, Griggs RL, Coxon C, Crossman M, et al. Associations between number of siblings, birth order, eating rate and adiposity in children and adults. Clin Obes. 2021;11:e12438.
Government of Canada SC. Statistics Canada. 2022 [cited 2023 Feb 15]. 2021 Census of Population - Toronto, City (C) [Census subdivision], Ontario. Available from: https://www12.statcan.gc.ca/census-recensement/2021/dp-pd/prof/index.cfm?Lang=E
Eny KM, Chen S, Anderson LN, Chen Y, Lebovic G, Pullenayegum E, et al. Breastfeeding duration, maternal body mass index, and birth weight are associated with differences in body mass index growth trajectories in early childhood. Am J Clin Nutr. 2018;107:584–92.
Buuren Svan, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45:1–67.
van Buuren S. Flexible imputation of missing data. Second edition. (International and comparative criminal justice series). Boca Raton, FL: Chapman and Hall/CRC, an imprint of Taylor and Francis; 2018.
Steen J, Loeys T, Moerkerke B, Vansteelandt S. Medflex: an R package for flexible mediation analysis using natural effect models. J Stat Softw. 2017;76:1–46.
Zeileis A, Köll S, Graham N. Various versatile variances: an object-oriented implementation of clustered covariances in R. J Stat Softw. 2020;95:36.
R Core Team. R: A language and environment for statistical computing [Internet]. Vienna, Austria: R Foundation for Statistical Computing; 2021. Available from: https://www.R-project.org/
Weir CB, Jan A. BMI classification percentile and cut off points. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 [cited 2022 Jun 3]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK541070/
Perez MR, de Castro LS, Chang YS, Sañudo A, Marcacine KO, Amir LH, et al. Breastfeeding Practices and problems among obese women compared with nonobese women in a Brazilian hospital. Women’s Health Rep. 2021;2:219–26.
Preusting I, Brumley J, Odibo L, Spatz DL, Louis JM. Obesity as a predictor of delayed lactogenesis II. J Hum Lact. 2017;33:684–91.
Nommsen-Rivers LA, Wagner EA, Roznowski DM, Riddle SW, Ward LP, Thompson A. Measures of maternal metabolic health as predictors of severely low milk production. Breastfeed Med J Acad Breastfeed Med. 2022;17:566–76.
Dennis CL. Theoretical underpinnings of breastfeeding confidence: a self-efficacy framework. J Hum Lact J Int Lact Consult Assoc. 1999;15:195–201.
Dias CC, Figueiredo B. Breastfeeding and depression: a systematic review of the literature. J Affect Disord. 2015;171:142–54.
Kair LR, Colaizy TT. Obese mothers have lower odds of experiencing pro-breastfeeding hospital practices than mothers of normal weight: CDC Pregnancy Risk Assessment Monitoring System (PRAMS), 2004-2008. Matern Child Health J. 2016;20:593–601.
DiSantis KI, Collins BN, Fisher JO, Davey A. Do infants fed directly from the breast have improved appetite regulation and slower growth during early childhood compared with infants fed from a bottle? Int J Behav Nutr Phys Act. 2011;8:89.
Larsen JK, Bode L. Obesogenic programming effects during lactation: a narrative review and conceptual model focusing on underlying mechanisms and promising future research avenues. Nutrients. 2021;13:299.
Yelverton CA, Geraghty AA, O’Brien EC, Killeen SL, Horan MK, Donnelly JM, et al. Breastfeeding and maternal eating behaviours are associated with child eating behaviours: findings from the ROLO Kids Study. Eur J Clin Nutr. 2021;75:670–9.
Taveras EM, Scanlon KS, Birch L, Rifas-Shiman SL, Rich-Edwards JW, Gillman MW. Association of breastfeeding with maternal control of infant feeding at age 1 year. Pediatrics. 2004;114:e577–583.
Orr SK, Dachner N, Frank L, Tarasuk V. Relation between household food insecurity and breastfeeding in Canada. CMAJ. 2018;190:E312–9.
Thulier D, Mercer J. Variables associated with breastfeeding duration. J Obstet Gynecol Neonatal Nurs. 2009;38:259–68.
Cohen AK, Rai M, Rehkopf DH, Abrams B. Educational attainment and obesity: a systematic review. Obes Rev. 2013;14:989–1005.
Headen I, Cohen AK, Mujahid M, Abrams B. The accuracy of self-reported pregnancy-related weight: a systematic review. Obes Rev. 2017;18:350–69.
Brownell EA, Hagadorn JI, Lussier MM, Goh G, Thevenet-Morrison KN, Lerer TJ, et al. Optimal periods of exclusive breastfeeding associated with any breastfeeding duration through one year. J Pediatr. 2015;166:566–.e1.
Acknowledgements
We thank the following sources of support; Clinician Scientist Training Program Scholarship (CSTP), Canadian Institute of Health Research (CIHR) and the Edwin S.H. Leong Centre for Healthy Children. We thank all of the participating families for their time and involvement in TARGet Kids! and are grateful to all practitioners who are currently involved in the TARGet Kids! practice-based research network.
Members of the TARGet Kids! Collaboration:
Co-Leads: Catherine S. Birken, MD, and Jonathon L. Maguire, MD.
Executive Committee: Christopher Allen, BSc; Laura N. Anderson, PhD; Danielle D’Annunzio, BA, LLM, PMP; Mateenah Jaleel, BSc; Charles Keown-Stoneman, PhD; Natricha Levy McFarlane, MPhil; Jessica A. Omand RD, PhD; and Sharon Thadani, MLA/T.
Investigators and Trainees: Mary Aglipay, MSc; Imaan Bayoumi, MD MSc; Cornelia M. Borkhoff, PhD; Sarah Carsley, PhD; Alice Charach, MD; Katherine Cost, PhD; Curtis D’Hollander RD MSc; Anne Fuller, MD; Laura Kinlin, MD MPH; Michaela Kucab RD, MSc; Patricia Li, MD MSc; Pat Parkin, MD; Nav Persaud, MD MSc; Sarah Rae, BHSc, MSc; Izabela Socynska, RD MSc; Shelley Vanderhout, RD PhD; Leigh Vanderloo, PhD; and Peter Wong, MD PhD.
Research Staff: Piyumi Konara Mudiyanselage, MSc; Xuedi Li, MSc; Jenny Liu, BHSc; Michelle Mitchell, BA; Yulika Yoshida-Montezuma, MPH; and Nusrat Zaffar, MBBS.
Clinical Site Research Staff: Trudy-Ann Buckley, BSc; Pamela Ruth Flores, MD; Kardelen Kurt, BSc; Sangeetha Loganathan, BPT; Tarandeep Mali, BSc; and Laurie Thompson, MLT.
Parent Partners: Jennifer Batten; Jennifer Chan; John Clark; Amy Craig; Kim De Castris-Garcia; Sharon Dharman; Sarah Kelleher; Salimah Nasser; Tammara Pabon; Michelle Rhodes; Rafael Salsa; Julie Skelding; Daniel Stern; Kerry Stewart; Erika Sendra Tavares; Shannon Weir; and Maria Zaccaria Cho.
Offord Centre for Child Studies Collaboration: Principal Investigator: Magdalena Janus, PhD; Co-investigator: Eric Duku, PhD; Research Team: Caroline Reid-Westoby, PhD; Patricia Raso, MSc; and Amanda Offord, MSc.
Site Investigators: Emy Abraham, MD; Sara Ali, MD; Kelly Anderson, MD; Gordon Arbess, MD; Jillian Baker, MD; Tony Barozzino, MD; Sylvie Bergeron, MD; Gary Bloch, MD; Joey Bonifacio, MD; Ashna Bowry, MD; Caroline Calpin, MD; Douglas Campbell, MD; Sohail Cheema, MD; Elaine Cheng, MD; Brian Chisamore, MD; Evelyn Constantin, MD; Karoon Danayan, MD; Paul Das, MD; Viveka De Guerra, MD; Mary Beth Derocher, MD; Anh Do, MD; Kathleen Doukas, MD; Anne Egger, BScN; Allison Farber, MD; Amy Freedman, MD; Sloane Freeman, MD; Sharon Gazeley, MD; Karen Grewal, MD; Charlie Guiang, MD; Dan Ha, MD; Curtis Handford, MD; Laura Hanson, BScN, RN; Leah Harrington, MD; Sheila Jacobson, MD; Lukasz Jagiello, MD; Gwen Jansz, MD; Paul Kadar, MD; Lukas Keiswetter, MD; Tara Kiran, MD; Holly Knowles, MD; Bruce Kwok, MD; Piya Lahiry, MD; Sheila Lakhoo, MD; Margarita Lam-Antoniades, MD; Eddy Lau, MD; Denis Leduc, MD; Fok-Han Leung, MD; Alan Li, MD; Patricia Li, MD; Roy Male, MD; Aleks Meret, MD; Elise Mok, MD; Rosemary Moodie, MD; Katherine Nash, BScN, RN; James Owen, MD; Michael Peer, MD; Marty Perlmutar, MD; Navindra Persaud, MD; Andrew Pinto, MD; Michelle Porepa, MD; Vikky Qi, MD; Noor Ramji, MD; Danyaal Raza, MD; Katherine Rouleau, MD; Caroline Ruderman, MD; Janet Saunderson, MD; Vanna Schiralli, MD; Michael Sgro, MD; Hafiz Shuja, MD; Farah Siam, MD; Susan Shepherd, MD; Cinntha Srikanthan, MD; Carolyn Taylor, MD; Stephen Treherne, MD; Suzanne Turner, MD; Fatima Uddin, MD; Meta van den Heuvel, MD; Thea Weisdorf, MD; Peter Wong, MD; John Yaremko, MD; Ethel Ying, MD; Elizabeth Young, MD; and Michael Zajdman, MD.
Applied Health Research Centre: Esmot Ara Begum, PhD; Peter Juni, MD, University of Toronto, Gurpreet Lakhanpal, MSc, CCRP, PMP; Gerald Lebovic, PhD, University of Toronto, Ifeayinchukwu (Shawn) Nnorom, BSc; Marc Denzel Nunez, HBSc; Audra Stitt, MSc; and Kevin Thorpe, MMath.
Mount Sinai Services Laboratory: Raya Assan, MSc, MLT; Homa Bondar, BSc; George S. Charames, PhD, FACMG; Andrea Djolovic, MSc, CCGC; Chelsea Gorscak-Dunn; Mary Hassan, MLT; Rita Kandel, MD; and Michelle Rodrigues, BSc, MLT.
Author information
Authors and Affiliations
Contributions
KEB, CDGK-S, CSB, DLOC, JLM: Designed research (project conception, development of overall research plan, and study oversight); KEB: Conducted research; CKS, JRS: Provided essential materials (research database, questionnaires); KEB, CDGK-S, XL: Preformed statistical analyses; KEB: Wrote paper; KEB, CSB: Had primary responsibility for final content; CLD, JAO, JRS, XL, CDGK-S, CSB, DLOC, JLM: provided expertise review and feedback on manuscript content; All authors read and approved manuscript.
Corresponding author
Ethics declarations
Competing interests
CSB reported receiving research funding from the Canadian Institute for Health Research Heart and Stroke Foundation of Canada, Physician Services Inc, The Edwin S.H. Leong Centre for Healthy Children, University of Toronto and Hospital for Sick Children, Centre for Addictions and Mental Health, Ontario Child Health Support Unit (OCHSU) Impact Child Health Award, and a Walmart Community Grant through the SickKids Foundation for a study on food insecurity in the inpatient hospital setting. JLM received an unrestricted research grant for a completed investigator-initiated study from the Dairy Farmers of Canada (2011–2012) and D drops provided non-financial support (vitamin D supplements) for an investigator-initiated study on vitamin D and respiratory tract infections (2011–2015). CLD reported receiving research funding from the Canadian Institute for Health Research. JRS reported receiving grant support from the Canadians Institutes of Health Research, the Danone Institute of Canada, the Canadian Foundation for Dietetic Research, and the Canadian Home Economics Foundation. The other authors had no conflicts of interest relevant to this article to disclose. The funding agencies had no role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, or the preparation, review, and approval of the manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Braddon, K.E., Keown-Stoneman, C.D.G., Dennis, CL. et al. The mediation effect of breastfeeding duration on the relationship between maternal preconception BMI and childhood nutritional risk. Eur J Clin Nutr 78, 427–435 (2024). https://doi.org/10.1038/s41430-024-01420-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-024-01420-0