Abstract
Objective
To determine the prevalence of eating disorders and orthorexia in postpartum women and examine the relationship with postpartum depression.
Study design
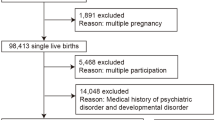
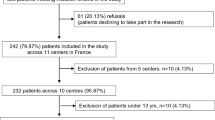
Included in this study were 227 postpartum women. The Eating Attitude Test-26 (EAT-26) was used to determine the risk of eating disorders in the women, followed by the Orthorexia 11 Scale (ORTO-11) to identify orthorexia, and the Edinburgh Postpartum Depression Scale (EPDS) to identify postpartum depression.
Results
63 of the women (27.8%) exhibited an orthorexic tendency, which was also related to eating disorders and postpartum depression. Each one-point increase in the EAT-26 score led to a decrease of 0.32 points in the ORTO-11 score. Similarly, each one-point increase in the EPDS score caused a reduction of 0.18 points in the ORTO-11 score. The ORTO-11 score increased by 0.26 points per each live birth.
Conclusion
An obsessive focus on healthful nutrition may result in the impairment of health and numerous adverse psychological and physiological outcomes in the future. Healthy eating habits should be maintained to improve the quality of life without causing an obsession with healthy eating.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
Bulik CM, Von Holle A, Siega-Riz AM, Torgersen L, Lie KK, Hamer RM, et al. Birth outcomes in women with eating disorders in the Norwegian Mother and Child cohort study (MoBa). Int J Eat Disord. 2009;42:9–18.
Franko DL, Blais MA, Becker AE, Delinsky SS, Greenwood DN, Flores AT, et al. Pregnancy complications and neonatal outcomes in women with eating disorders. Am J Psychiatry. 2001;158:1461–1466.
Hendrick VC. Psychiatric disorders in pregnancy and the postpartum: principles and treatment. New Jersey: Humana Press; 2006.
Koven NS, Abry AW. The clinical basis of orthorexia nervosa: emerging perspectives. Neuropsychiatr Dis Treat. 2015;11:385–394.
APA. Diagnostic and Statistical Manual of Mental Disorders-V. 5th ed. Arlington, VA: Amerikan Psychiatric Association; 2013.
Turner PG, Lefevre CE. Instagram use is linked to increased symptoms of orthorexia nervosa. Eat Weight Disord - Stud Anorex, Bulim Obes. 2017;22:277–284.
Ulfvebrand S, Birgegard A, Norring C, Högdahl L, von Hausswolff-Juhlin Y. Psychiatric comorbidity in women and men with eating disorders results from a large clinical database. Psychiatry Res. 2015;230:294–299.
Lee MF, Madsen J, Williams SL, Browne M, Burke KJ. Differential effects of intuitive and disordered eating on physical and psychological outcomes for women with young children. Matern Child Health J. 2022;26:1–8.
O’Hara MW, Swain AM. Rates and risk of postpartum depression - a meta-analysis. Int Rev Psychiatry. 1996;8:37–54.
Özcan NK, Boyacıoğlu NE, Dinç H. Postpartum depression prevalence and risk factors in Turkey: a systematic review and meta-analysis. Arch Psychiatr Nurs. 2017;31:420–428.
Kimmel MC, Ferguson EH, Zerwas S, Bulik CM, Meltzer-Brody S. Obstetric and gynecologic problems associated with eating disorders. Int J Eat Disord. 2016;49:260–275.
Mazzeo SE, Slof-Op’t Landt MCT, Jones I, Mitchell K, Kendler KS, Neale MC, et al. Associations among postpartum depression, eating disorders, and perfectionism in a population-based sample of adult women. Int J Eat Disord. 2006;39:202–211.
Micali N, Simonoff E, Treasure J. Pregnancy and post-partum depression and anxiety in a longitudinal general population cohort: The effect of eating disorders and past depression. J Affect Disord. 2011;131:150–157.
Lee MF, Williams SL, Burke KJ. Striving for the thin ideal post-pregnancy: a cross-sectional study of intuitive eating in postpartum women. J Reprod Infant Psychol. 2020;38:127–138.
Kappa HM, Litteral JL, Keim SA, Jackson JL, Schofield KA, Crerand CE. Body image dissatisfaction, breastfeeding experiences, and self-efficacy in postpartum women with and without eating disorder symptoms. J Hum Lact. 2022;38:633–643.
Rodgers RF, O’Flynn JL, Bourdeau A, Zimmerman E. A biopsychosocial model of body image, disordered eating, and breastfeeding among postpartum women. Appetite. 2018;126:163–168.
Lacey JH, Smith G. Bulimia Nervosa. Br J Psychiatry. 1987;150:777–781.
Morgan JF, Lacey JH, Sedgwick PM. Impact of pregnancy on bulimia nervosa. Br J Psychiatry. 1999;174:135–140.
Vanderkruik R, Ellison K, Kanamori M, Freeman MP, Cohen LS, Stice E. Body dissatisfaction and disordered eating in the perinatal period: an underrecognized high-risk timeframe and the opportunity to intervene. Arch Women’s Ment Health. 2022;25:739–751.
Makino M, Yasushi M, Tsutsui S. The risk of eating disorder relapse during pregnancy and after delivery and postpartum depression among women recovered from eating disorders. BMC Pregnancy Childbirth. 2020;20:323.
Martini MG, Bramante A, Micali N. Eating Disorders in pregnancy and postpartum period. In: Percudani M, Brenna V, Pariante C (ed). Key Topics in Perinatal Mental Health. New Jersey: Cham: Springer International Publishing; 2022, 127–137.
Pettersson CB, Zandian M, Clinton D. Eating disorder symptoms pre- and postpartum. Arch Women’s Ment Health. 2016;19:675–680.
Nathina C. A guide for occupational therapist working with women with postpartum depression and eating disorders. North Dokato: University of North Dakota; 2021.
WHO. Global Database on Body Mass Index (BMI). 2020. Available from: https://www.who.int/nutrition/databases/bmi/en/
Garner DM, Garfinkel PE. The eating attitudes test: an index of the symptoms of anorexia nervosa. Psychol Med. 1979;9:273–279.
Erol N, Savaşır I. Eating attitude test: an index of anorexia nervosa symptoms. Turkish J Psychol. 1989;23:132–136.
Rivas T, Bersabé R, Jiménez M, Berrocal C. The eating attitudes test (EAT-26): reliability and validity in spanish female samples. Span J Psychol. 2010;13:1044–1056.
Donini LM, Marsili D, Graziani MP, Imbriale M, Cannella C. Orthorexia nervosa: a preliminary study with a proposal for diagnosis and an attempt to measure the dimension of the phenomenon. Eat Weight Disord. 2004;9:151–157.
Arusoğlu G, Kabakcı E, Köksal G. Ortoreksiya Nervoza ve ORTO-11’in Türkçeye Uyarlama Çalışması. Türk Psikiyatr Derg. 2008;19:283–291.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–786.
Karaçam Z, Kiriş Y. The Postpartum Depression Screening Scale: its reliability and validity for the Turkish population. Turk Psikiyatr Derg. 2008;19:187–196.
Easter A, Solmi F, Bye A, Taborelli E, Corfield F, Schmidt U, et al. Antenatal and postnatal psychopathology among women with current and past eating disorders: longitudinal patterns. Eur Eat Disord Rev. 2015;23:19–27.
Angélica Nunes M, Poyastro Pinheiro A, Feliciati Hoffmann J, Inês Schmidt M. Eating disorders symptoms in pregnancy and postpartum: a prospective study in a disadvantaged population in Brazil. Int J Eat Disord. 2014;47:426–430.
Cici Saraç N, Bülbül S. Doğum sonrası kadınlarda beslenme bozukluklarının varlığının saptaması. Kırıkkale University; 2018. Master Thesis, Kırıkkale, Turkey.
Tayhan Kartal F, Yabancı Ayhan N. Relationship between eating disorders and internet and smartphone addiction in college students. Eat Weight Disord. 2020;26:1853–1862.
Kadioglu M, Ergun A. The eating attitudes of the university students, self-efficacy and affecting factors. J Marmara Univ Inst Heal Sci. 2015;5:96–104.
CDC. Increase the proportion of women delivering a live birth who had a healthy weight prior to pregnancy (Maternal Infant and Child Health). 2011. Available from: https://www.cdc.gov/nchs/data/hpdata2020/hp2020_FP_MICH_Progress_Review_Appendix.pdf
Linardon J, Braithwaite R, Cousins R, Brennan L. Appearance-based rejection sensitivity as a mediator of the relationship between symptoms of social anxiety and disordered eating cognitions and behaviors. Eat Behav. 2017;27:27–32.
Siega-Riz AM, Von Holle A, Haugen M, Meltzer HM, Hamer R, Torgersen L, et al. Gestational weight gain of women with eating disorders in the Norwegian pregnancy cohort. Int J Eat Disord. 2011;44:428–434.
Zerwas SC, Von Holle A, Perrin EM, Cockrell Skinner A, Reba-Harrelson L, Hamer RM, et al. Gestational and postpartum weight change patterns in mothers with eating disorders. Eur Eat Disord Rev. 2014;22:397–404.
Bergmeier H, Hill B, Haycraft E, Blewitt C, Lim S, Meyer C, et al. Maternal body dissatisfaction in pregnancy, postpartum and early parenting: An overlooked factor implicated in maternal and childhood obesity risk. Appetite. 2020;147:104525.
Koven N, Abry A. The clinical basis of orthorexia nervosa: emerging perspectives. Neuropsychiatr Dis Treat. 2015;18:385–394.
Altıner R, Okumuş F. Gebelerde Ortoreksiya Nervoza Eğiliminin Belirlenmesi. İstanbul Medipol University; 2019. Master Thesis, İstanbul, Turkey.
Ayhan Baser D, Cankurtaran M. The assessment of the orthorexia nervosa tendencies among postpartum women. Konuralp Med J 2021;13:218–225.
Arslantaş H. Eating behaviour and orthorexia nervosa (healthy eating obsession) in nursing students: cross-sectional analytic study. J Psychiatr Nurs. 2017;8:137–143.
Gezer C, Kabaran S. Orthorexia nervosa: is it a risk for female students studying nutrition and dietetics? Süleyman Demirel Üniversitesi Sağlık Bilim Derg. 2013;4:14–22.
Arusoğlu G. Healthy eating obsession (orthorexia): examination of the symptoms, the adaptation of ORTO-15. [In Turkish.] Ankara, Turkey: Hacettepe University; 2006.
Franko DL, Walton BE. Pregnancy and eating disorders: a review and clinical implications. Int J Eat Disord. 1993;13:41–47.
Lovering ME, Rodgers RF, George JE, Franko DL. Exploring the tripartite influence model of body dissatisfaction in postpartum women. Body Image. 2018;24:44–54.
Shorey S, Chee CYI, Ng ED, Chan YH, Tam WWS, Chong YS. Prevalence and incidence of postpartum depression among healthy mothers: a systematic review and meta-analysis. J Psychiatr Res. 2018;104:235–248.
Moroze RM, Dunn TM, Craig Holland J, Yager J, Weintraub P. Microthinking about micronutrients: a case of transition from obsessions about healthy eating to near-fatal “orthorexia nervosa” and proposed diagnostic criteria. Psychosomatics. 2015;56:397–403.
Lopes R, Melo R, Dias Pereira B. Orthorexia nervosa and comorbid depression successfully treated with mirtazapine: a case report. Eat Weight Disord. 2020;25:163–167.
Luck-Sikorski C, Jung F, Schlosser K, Riedel-Heller SG. Is orthorexic behavior common in the general public? A large representative study in Germany. Eat Weight Disord. 2019;24:267–273.
Author information
Authors and Affiliations
Contributions
FT was responsible for conceptualizing the research protocol, writing the protocol and report, conducting the research, analyzing data, interpreting results, adjusting the manuscript according to the comments of co-authors, updating reference lists and forming ‘Summary of findings’ tables. GD and NYA were responsible for designing the research protocol and screening potentially appropriate studies. They provided a review and critical evaluation of the manuscript. CS contributed to collecting the data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tayhan, F., Doğan, G., Yabancı Ayhan, N. et al. Assessment of eating disorders and depression in postpartum women. Eur J Clin Nutr 78, 314–319 (2024). https://doi.org/10.1038/s41430-023-01384-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-023-01384-7