Abstract
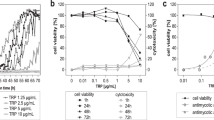
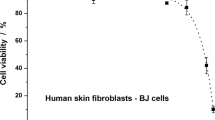
A new biological activity was discovered for marine fungal meroterpenoid meroantarctine A with unique 6/5/6/6 polycyclic system. It was found that meroantarctine A can significantly reduce biofilm formation by Staphylococcus aureus with an IC50 of 9.2 µM via inhibition of sortase A activity. Co-cultivation of HaCaT keratinocytes with a S. aureus suspension was used as an in vitro model of skin infection. Treatment of S. aureus-infected HaCaT cells with meroantarctine A at 10 µM caused a reduction in the production of TNF-α, IL-18, NO, and ROS, as well as LDH release and caspase 1 activation in these cells and, finally, recovered the proliferation and migration of HaCaT cells in an in vitro wound healing assay up to the control level. Thus, meroantarctine A is a new promising antibiofilm compound which can effective against S. aureus caused skin infection.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The original data presented in the study are included in the article; further inquiries can be directed to the corresponding author.
References
de Oliveira Santos JV, et al. Panorama of bacterial infections caused by epidemic resistant strains. Curr Microbiol. 2022;79:175.
Ikuta KS, et al. Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2022;400:2221–48.
Yang L, et al. Global epidemiology of asymptomatic colonisation of methicillin-resistant Staphylococcus aureus in the upper respiratory tract of young children: a systematic review and meta-analysis. Arch Dis Child. 2024;109:267.
Murray CJ, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399:629–55.
Liang Y, Li J, Hou L, Zhang X, Hou G, Zhang W. Changes of Staphylococcus aureus infection in children before and after the COVID-19 pandemic, Henan, China. J Infect. 2023;86:e70–e71.
Outterson K, Orubu ESF, Rex J, Årdal C, Zaman MH. Patient access in 14 high-income countries to new antibacterials approved by the US Food and Drug Administration, European Medicines Agency, Japanese Pharmaceuticals and Medical Devices Agency, or Health Canada, 2010–2020. Clin Infect Dis. 2022;74:1183–90.
Theuretzbacher U, Outterson K, Engel A, Karlén A. The global preclinical antibacterial pipeline. Nat Rev Microbiol. 2020;18:275–85.
Wang C, Tang S, Cao S. Antimicrobial compounds from marine fungi. Phytochem Rev. 2021;20:85–117.
El-Demerdash A, Kumla D, Kijjoa A. Chemical diversity and biological activities of meroterpenoids from marine derived-fungi: a comprehensive update. Mar Drugs 2020;18:317.
Gomes NM, et al. Antibacterial and antibiofilm activities of tryptoquivalines and meroditerpenes isolated from the marine-derived fungi Neosartorya paulistensis, N. laciniosa, N. tsunodae, and the soil fungi N. fischeri and N. siamensis. Mar Drugs. 2014;12:822–39.
Leshchenko EV, et al. Meroantarctines A–C, meroterpenoids with rearranged skeletons from the alga-derived fungus Penicillium antarcticum KMM 4685 with potent p-glycoprotein inhibitory activity. J Nat Prod. 2022;85:2746–52.
Zhuravleva OI, et al. Anthraquinone derivatives and other aromatic compounds from marine fungus Asteromyces cruciatus KMM 4696 and their effects against Staphylococcus aureus. Mar Drugs. 2023;21:431.
Yurchenko AN, et al. New cyclopiane diterpenes and polyketide derivatives from marine sediment-derived fungus Penicillium antarcticum KMM 4670 and their biological activities. Mar Drugs. 2023;21:584.
Campbell J. High‐throughput assessment of bacterial growth inhibition by optical density measurements. Curr Protoc Chem Biol. 2010;2:195–208.
Kifer D, Mužinić V, Klarić MŠ. Antimicrobial potency of single and combined mupirocin and monoterpenes, thymol, menthol and 1, 8-cineole against Staphylococcus aureus planktonic and biofilm growth. J Antibiot (Tokyo). 2016;69:689–96.
Grosdidier A, Zoete V, Michielin O. SwissDock, a protein-small molecule docking web service based on EADock DSS. Nucleic Acids Res. 2011;39:W270–277.
Brooks BR, et al. CHARMM: The biomolecular simulation program. J Comput Chem. 2009;30:1545–614.
Haberthür U, Caflisch A. FACTS: Fast analytical continuum treatment of solvation. J Comput Chem. 2008;29:701–15.
Grosdidier A, Zoete V, Michielin O. Fast docking using the CHARMM force field with EADock DSS. J Comput Chem. 2011;32:2149–59.
Yurchenko EA, Khmel OO, Nesterenko LE, Aminin DL. The Kelch/Nrf2 antioxidant system as a target for some marine fungal metabolites. Oxygen. 2023;3:374–85.
Kozlovskiy SA, et al. Anti-inflammatory activity of 1,4-naphthoquinones blocking P2X7 purinergic receptors in RAW 264.7 macrophage cells. Toxins. 2023;15:47.
Girich EV, et al. Absolute stereochemistry and cytotoxic effects of vismione E from marine sponge-derived fungus Aspergillus sp. 1901NT-1.2.2. Int J Mol Sci. 2023;24:8150.
Zong Y, Bice TW, Ton-That H, Schneewind O, Narayana SVL. Crystal structures of Staphylococcus aureus sortase A and its substrate complex. J Biol Chem. 2004;279:31383–9.
Tsuchiya K. Inflammasome-associated cell death: pyroptosis, apoptosis, and physiological implications. Microbiol Immunol. 2020;64:252–69.
Jang KO, Lee YW, Kim H, Chung DK. Complement inactivation strategy of Staphylococcus aureus using decay-accelerating factor and the response of infected HaCaT cells. Int J Mol Sci. 2021;22:4015.
Paharik AE, Horswill AR. The Staphylococcal biofilm: adhesins, regulation, and host response. Microbiol Spectrum. 2016;4:VMBF-0022-2015
Malone M, et al. The prevalence of biofilms in chronic wounds: a systematic review and meta-analysis of published data. J Wound Care. 2017;26:20–25.
Simonetti O, et al. New perspectives on old and new therapies of staphylococcal skin infections: the role of biofilm targeting in wound healing. Antibiotics. 2021;10:1377.
Guo N, Bai X, Shen Y, Zhang T. Target-based screening for natural products against Staphylococcus aureus biofilms. Crit Rev Food Sci Nutr. 2023;63:2216–30.
Wang X, et al. The protection effect of rhodionin against methicillin-resistant Staphylococcus aureus-induced pneumonia through sortase A inhibition. World J Microbiol Biotechnol. 2022;39:18.
Kudryavtsev KV, Fedotcheva TA, Shimanovsky NL. Inhibitors of sortases of gram-positive bacteria and their role in the treatment of infectious diseases (review). Pharm Chem J 2021;55:751–6.
Jiang T, et al. Echinacoside, a promising sortase A inhibitor, combined with vancomycin against murine models of MRSA-induced pneumonia. Med Microbiol Immunol. 2023;212:421–35.
Marraffini LA, Ton-That H, Zong Y, Narayana SVL, Schneewind O. Anchoring of surface proteins to the cell wall of Staphylococcus aureus: a conserved arginine residue is required for efficient catalysis of sortase A. J Biol Chem. 2004;279:37763–70.
Thappeta KR, et al. In-Silico identified new natural sortase A inhibitors disrupt S. aureus biofilm formation. Int J Mol Sci. 2020;21:8601.
Missiakas D, Winstel V. Selective host cell death by Staphylococcus aureus: A strategy for bacterial persistence. Front Immunol. 2021;11:621733.
Cheng Y-L, et al. Staphylococcus aureus induces microglial inflammation via a glycogen synthase kinase 3β-regulated pathway. Infect Immun. 2009;77:4002–8.
Gómez MI, et al. Staphylococcus aureus protein A induces airway epithelial inflammatory responses by activating TNFR1. Nat Med. 2004;10:842–8.
Alexander EH, Rivera FA, Marriott I, Anguita J, Bost KL, Hudson MC. Staphylococcus aureus - induced tumor necrosis factor - related apoptosis - inducing ligand expression mediates apoptosis and caspase-8 activation in infected osteoblasts. BMC Microbiol. 2003;3:5.
Jelachich Mary L, Lipton Howard L. Theiler’s murine encephalomyelitis virus induces apoptosis in gamma interferon-activated M1 differentiated myelomonocytic cells through a mechanism involving tumor necrosis factor alpha (TNF-α) and TNF-α-related apoptosis-inducing ligand. J Virol. 2001;75:5930–8.
Lima Leite E, et al. Involvement of caspase‐1 in inflammasomes activation and bacterial clearance in S. aureus‐infected osteoblast‐like MG‐63 cells. Cell Microbiol. 2020;22:e13204.
Hu XM, et al. Guidelines for regulated cell death assays: a systematic summary, a categorical comparison, a prospective. Front Cell Developmental Biol. 2021;9:634690.
Syed AK, Reed TJ, Clark KL, Boles BR, Kahlenberg JM. Staphlyococcus aureus phenol-soluble modulins stimulate the release of proinflammatory cytokines from keratinocytes and are required for induction of skin inflammation. Infect Immun. 2015;83:3428–37.
Soe YM, Bedoui S, Stinear TP, Hachani A. Intracellular Staphylococcus aureus and host cell death pathways. Cell Microbiol. 2021;23:e13317.
Wiegand C, Abel M, Ruth P, Hipler UC. HaCaT keratinocytes in co-culture with Staphylococcus aureus can be protected from bacterial damage by polihexanide. Wound Repair Regeneration. 2009;17:730–8.
Kirker KR, Secor PR, James GA, Fleckman P, Olerud JE, Stewart PS. Loss of viability and induction of apoptosis in human keratinocytes exposed to Staphylococcus aureus biofilms in vitro. Wound Repair Regeneration. 2009;17:690–9.
Chingizova EA, et al. Marine fungal cerebroside flavuside B protects HaCaT keratinocytes against Staphylococcus aureus induced damage. Mar Drugs 2021;19:553.
Yurchenko EA, et al. Cytoprotective activity of p-terphenyl polyketides and flavuside B from marine-derived fungi against oxidative stress in Neuro-2a cells. Molecules. 2021;26:3618.
Seo S-H, Jeong G-S. Fisetin inhibits TNF-α-induced inflammatory action and hydrogen peroxide-induced oxidative damage in human keratinocyte HaCaT cells through PI3K/AKT/Nrf-2-mediated heme oxygenase-1 expression. Int Immunopharmacol 2015;29:246–53.
Moormeier DE, Bose JL, Horswill AR, Bayles KW. Temporal and stochastic control of Staphylococcus aureus biofilm development. mBio. 2014;5:e01341–14. https://doi.org/10.1128/mbio.01341-01314
Díaz-Navarro M, et al. Understanding the diagnosis of catheter-related bloodstream infection: real-time monitoring of biofilm growth dynamics using time-lapse optical microscopy. Front Cell Infect Microbiol. 2023;13:1286527.
Caudal F, et al. Anti-biofilm extracts and molecules from the marine environment. Mar Drugs. 2024;22:313.
Acknowledgements
This study was carried out using the equipment of the Collective Facilities Center “The Far Eastern Center for Structural Molecular Research (NMR/MS) PIBOC FEB RAS” and using the Collective Facilities Center “Collection of Marine Microorganisms PIBOC FEB RAS”.
Funding
This research was funded by the Russian Science Foundation (grant number 23-24-00471).
Author information
Authors and Affiliations
Contributions
Conceptualization, EAY and EAC; methodology, EAY, EAC and ESM; software, EAY, ASK and ANY; validation, DLA, and IVG; formal analysis, ESM, ASK and EAC; investigation, EAC, ARC, ESM, EAP, EVL, GVB, and EAY; resources, IVG and EAC; data curation, DLA and EAY; writing—original draft prep-aration, EAC, and EAY; writing—review and editing, DLA and IVG; visualization, ESM, EAP, and EAC supervision, EAY and DLA; project administration, EAC and EAY; funding acquisition, EAC. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chingizova, E.A., Chingizov, A.R., Menchinskaya, E.S. et al. The influence of marine fungal meroterpenoid meroantarctine A toward HaCaT keratinocytes infected with Staphylococcus aureus. J Antibiot (2024). https://doi.org/10.1038/s41429-024-00771-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41429-024-00771-x