Abstract
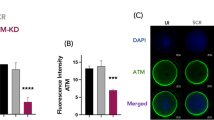
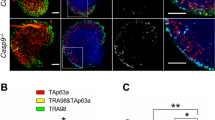
Aneuploidy, the presence of a chromosomal anomaly, is a major cause of spontaneous abortions and recurrent pregnancy loss in humans. However, the underlying molecular mechanisms still remain poorly understood. Here, we report that ARHGAP26, a putative tumor suppressor gene, is a newly identified regulator of oocyte quality to maintain mitochondrial integrity and chromosome euploidy, thus ensuring normal embryonic development and fertility. Taking advantage of knockout mouse model, we revealed that genetic ablation of Arhgap26 caused the oocyte death at GV stage due to the mitochondrial dysfunction-induced ROS accumulation. Lack of Arhgap26 also impaired both in vitro and in vivo maturation of survived oocytes which results in maturation arrest and aneuploidy, and consequently leading to early embryonic development defects and subfertility. These observations were further verified by transcriptome analysis. Mechanistically, we discovered that Arhgap26 interacted with Cofilin1 to maintain the mitochondrial integrity by regulating Drp1 dynamics, and restoration of Arhgap26 protein level recovered the quality of Arhgap26-null oocytes. Importantly, we found an ARHGAP26 mutation in a patient with history of recurrent miscarriage by chromosomal microarray analysis. Altogether, our findings uncover a novel function of ARHGAP26 in the oocyte quality control and prevention of aneuploidy and provide a potential treatment strategy for infertile women caused by ARHGAP26 mutation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
All study data are included in the article and Supplementary information. Data supporting the findings of this study are available on reasonable request from the corresponding authors.
References
Robinson GE. Pregnancy loss. Best Pract Res Clin Obstet Gynaecol. 2014;28:169–78.
Quenby S, Gallos ID, Dhillon-Smith RK, Podesek M, Stephenson MD, Fisher J, et al. Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss. Lancet. 2021;397:1658–67.
Garrido-Gimenez C, Alijotas-Reig J. Recurrent miscarriage: causes, evaluation and management. Postgrad Med J. 2015;91:151–62.
Magnus MC, Wilcox AJ, Morken NH, Weinberg CR, Haberg SE. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. BMJ. 2019;364:l869.
Korshunov MN, Korshunova ES, Kastrikin YV, E EA, Darenkov SP. [The role of male factor in pregnancy loss]. Urologiia 2021;4:152–7.
du Fosse NA, van der Hoorn MP, van Lith JMM, le Cessie S, Lashley E. Advanced paternal age is associated with an increased risk of spontaneous miscarriage: a systematic review and meta-analysis. Hum Reprod Update. 2020;26:650–69.
Du Y, Chen L, Lin J, Zhu J, Zhang N, Qiu X, et al. Chromosomal karyotype in chorionic villi of recurrent spontaneous abortion patients. Biosci Trends. 2018;12:32–39.
Soler A, Morales C, Mademont-Soler I, Margarit E, Borrell A, Borobio V, et al. Overview of chromosome abnormalities in first trimester miscarriages: a series of 1,011 consecutive chorionic villi sample karyotypes. Cytogenet Genome Res. 2017;152:81–89.
Sugiura-Ogasawara M, Ozaki Y, Katano K, Suzumori N, Kitaori T, Mizutani E. Abnormal embryonic karyotype is the most frequent cause of recurrent miscarriage. Hum Reprod. 2012;27:2297–303.
Werner M, Reh A, Grifo J, Perle MA. Characteristics of chromosomal abnormalities diagnosed after spontaneous abortions in an infertile population. J Assist Reprod Genet. 2012;29:817–20.
Bolor H, Mori T, Nishiyama S, Ito Y, Hosoba E, Inagaki H, et al. Mutations of the SYCP3 gene in women with recurrent pregnancy loss. Am J Hum Genet. 2009;84:14–20.
Singh P, Fragoza R, Blengini CS, Tran TN, Pannafino G, Al-Sweel N, et al. Human MLH1/3 variants causing aneuploidy, pregnancy loss, and premature reproductive aging. Nat Commun. 2021;12:5005.
Lv S, Liu M, Xu L, Zhang C. Downregulation of decidual SKP2 is associated with human recurrent miscarriage. Reprod Biol Endocrinol. 2021;19:88.
Hildebrand JD, Taylor JM, Parsons JT. An SH3 domain-containing GTPase-activating protein for Rho and Cdc42 associates with focal adhesion kinase. Mol Cell Biol. 1996;16:3169–78.
Taylor JM, Macklem MM, Parsons JT. Cytoskeletal changes induced by GRAF, the GTPase regulator associated with focal adhesion kinase, are mediated by Rho. J Cell Sci. 1999;112:231–42.
Francis MK, Holst MR, Vidal-Quadras M, Henriksson S, Santarella-Mellwig R, Sandblad L, et al. Endocytic membrane turnover at the leading edge is driven by a transient interaction between Cdc42 and GRAF1. J Cell Sci. 2015;128:4183–95.
Doherty GJ, Ahlund MK, Howes MT, Moren B, Parton RG, McMahon HT, et al. The endocytic protein GRAF1 is directed to cell-matrix adhesion sites and regulates cell spreading. Mol Biol Cell. 2011;22:4380–9.
Lundmark R, Doherty GJ, Howes MT, Cortese K, Vallis Y, Parton RG, et al. The GTPase-activating protein GRAF1 regulates the CLIC/GEEC endocytic pathway. Curr Biol. 2008;18:1802–8.
Nonnenmacher M, Weber T. Adeno-associated virus 2 infection requires endocytosis through the CLIC/GEEC pathway. Cell Host Microbe. 2011;10:563–76.
Simpson KJ, Selfors LM, Bui J, Reynolds A, Leake D, Khvorova A, et al. Identification of genes that regulate epithelial cell migration using an siRNA screening approach. Nat Cell Biol. 2008;10:1027–38.
Stergiou L, Bauer M, Mair W, Bausch-Fluck D, Drayman N, Wollscheid B, et al. Integrin-mediated signaling induced by simian virus 40 leads to transient uncoupling of cortical actin and the plasma membrane. PLoS ONE. 2013;8:e55799.
Bai X, Zhu Q, Combs M, Wabitsch M, Mack CP, Taylor JM. GRAF1 regulates brown and beige adipose differentiation and function. Res Sq. 2023:rs.3.rs-3740465. https://doi.org/10.21203/rs.3.rs-3740465/v1.
Lucken-Ardjomande Hasler S, Vallis Y, Jolin HE, McKenzie AN, McMahon HT. GRAF1a is a brain-specific protein that promotes lipid droplet clustering and growth, and is enriched at lipid droplet junctions. J Cell Sci. 2014;127:4602–19.
Lenhart KC, Becherer AL, Li J, Xiao X, McNally EM, Mack CP, et al. GRAF1 promotes ferlin-dependent myoblast fusion. Dev Biol. 2014;393:298–311.
Zhu Q, Combs ME, Liu J, Bai X, Wang WB, Herring LE, et al. GRAF1 integrates PINK1-Parkin signaling and actin dynamics to mediate cardiac mitochondrial homeostasis. Nat Commun. 2023;14:8187.
Zhu Q, Combs ME, Bowles DE, Gross RT, Mendiola Pla M, Mack CP, et al. GRAF1 acts as a downstream mediator of parkin to regulate mitophagy in cardiomyocytes. Cells. 2024;13:448.
Aly RM, Ghazy HF. High expression of GTPase regulator associated with the focal adhesion kinase (GRAF) is a favorable prognostic factor in acute myeloid leukemia. Blood Cells Mol Dis. 2014;53:185–8.
Borkhardt A, Bojesen S, Haas OA, Fuchs U, Bartelheimer D, Loncarevic IF, et al. The human GRAF gene is fused to MLL in a unique t(5;11)(q31;q23) and both alleles are disrupted in three cases of myelodysplastic syndrome/acute myeloid leukemia with a deletion 5q. Proc Natl Acad Sci USA. 2000;97:9168–73.
Zohrabian VM, Nandu H, Gulati N, Khitrov G, Zhao C, Mohan A, et al. Gene expression profiling of metastatic brain cancer. Oncol Rep. 2007;18:321–8.
Li J, Zheng X, Jia J, Xie B, Zhang C, Wang H, et al. CLDN18-ARHGAP26 function in gastric cancer and be a new therapeutic target by ABCG2 and ABCB1 pathway. Food Sci Tech. 2022;42:e54821.
Xu G, Zhao L, Hua Q, Wang L, Liu H, Lin Z, et al. CEMIP, acting as a scaffold protein for bridging GRAF1 and MIB1, promotes colorectal cancer metastasis via activating CDC42/MAPK pathway. Cell Death Dis. 2023;14:167.
Chen X, Chen S, Li Y, Gao Y, Huang S, Li H, et al. SMURF1-mediated ubiquitination of ARHGAP26 promotes ovarian cancer cell invasion and migration. Exp Mol Med. 2019;51:1–12.
Xiong B, Li S, Ai JS, Yin S, Ouyang YC, Sun SC, et al. BRCA1 is required for meiotic spindle assembly and spindle assembly checkpoint activation in mouse oocytes. Biol Reprod. 2008;79:718–26.
Winship AL, Alesi LR, Stringer JM, Cao Y, Lewis YM, Tu L, et al. Conditional loss of Brca1 in oocytes causes reduced litter size, ovarian reserve depletion and impaired oocyte in vitro maturation with advanced reproductive age in mice. EBioMedicine. 2024;106:105262.
Bai L, Li P, Xiang Y, Jiao X, Chen J, Song L, et al. BRCA1 safeguards genome integrity by activating chromosome asynapsis checkpoint to eliminate recombination-defective oocytes. Proc Natl Acad Sci USA. 2024;121:e2401386121.
Miao Y, Wang P, Xie B, Yang M, Li S, Cui Z, et al. BRCA2 deficiency is a potential driver for human primary ovarian insufficiency. Cell Death Dis. 2019;10:474.
Weinberg-Shukron A, Rachmiel M, Renbaum P, Gulsuner S, Walsh T, Lobel O, et al. Essential role of BRCA2 in ovarian development and function. N Engl J Med. 2018;379:1042–9.
Bolcun-Filas E, Rinaldi VD, White ME, Schimenti JC. Reversal of female infertility by Chk2 ablation reveals the oocyte DNA damage checkpoint pathway. Science. 2014;343:533–6.
Tuppi M, Kehrloesser S, Coutandin DW, Rossi V, Luh LM, Strubel A, et al. Oocyte DNA damage quality control requires consecutive interplay of CHK2 and CK1 to activate p63. Nat Struct Mol Biol. 2018;25:261–9.
Dai XX, Duan X, Liu HL, Cui XS, Kim NH, Sun SC. Chk2 regulates cell cycle progression during mouse oocyte maturation and early embryo development. Mol Cells. 2014;37:126–32.
Luan Y, Yu SY, Abazarikia A, Dong R, Kim SY. TAp63 determines the fate of oocytes against DNA damage. Sci Adv. 2022;8:eade1846.
Huang C, Zhao S, Yang Y, Guo T, Ke H, Mi X, et al. TP63 gain-of-function mutations cause premature ovarian insufficiency by inducing oocyte apoptosis. J Clin Invest. 2023;133:e162315.
Suh EK, Yang A, Kettenbach A, Bamberger C, Michaelis AH, Zhu Z, et al. p63 protects the female germ line during meiotic arrest. Nature. 2006;444:624–8.
Dumollard R, Duchen M, Carroll J. The role of mitochondrial function in the oocyte and embryo. Curr Top Dev Biol. 2007;77:21–49.
Wang LY, Wang DH, Zou XY, Xu CM. Mitochondrial functions on oocytes and preimplantation embryos. J Zhejiang Univ Sci B. 2009;10:483–92.
Miao Y, Cui Z, Gao Q, Rui R, Xiong B. Nicotinamide mononucleotide supplementation reverses the declining quality of maternally aged oocytes. Cell Rep. 2020;32:107987.
Wang W, Liu H, Liu S, Hao T, Wei Y, Wei H, et al. Oocyte-specific deletion of eukaryotic translation initiation factor 5 causes apoptosis of mouse oocytes within the early-growing follicles by mitochondrial fission defect-reactive oxygen species-DNA damage. Clin Transl Med. 2024;14:e1791.
Zhang H, Pan Z, Ju J, Xing C, Li X, Shan M, et al. DRP1 deficiency induces mitochondrial dysfunction and oxidative stress-mediated apoptosis during porcine oocyte maturation. J Anim Sci Biotechnol. 2020;11:77.
Rehklau K, Hoffmann L, Gurniak CB, Ott M, Witke W, Scorrano L, et al. Cofilin1-dependent actin dynamics control DRP1-mediated mitochondrial fission. Cell Death Dis. 2017;8:e3063.
Papas RS, Kutteh WH. Genetic testing for aneuploidy in patients who have had multiple miscarriages: a review of current literature. Appl Clin Genet. 2021;14:321–9.
Wang K, Lu Y, Morrow DF, Xiao D, Xu C. Alzheimer’s disease neuroimaging I. Associations of ARHGAP26 polymorphisms with Alzheimer’s disease and cardiovascular disease. J Mol Neurosci. 2022;72:1085–97.
Wang Q, Stringer JM, Liu J, Hutt KJ. Evaluation of mitochondria in oocytes following gamma-irradiation. Sci Rep. 2019;9:19941.
Zhang D, Keilty D, Zhang ZF, Chian RC. Mitochondria in oocyte aging: current understanding. Facts Views Vis Obgyn. 2017;9:29–38.
Colley E, Hamilton S, Smith P, Morgan NV, Coomarasamy A, Allen S. Potential genetic causes of miscarriage in euploid pregnancies: a systematic review. Hum Reprod Update. 2019;25:452–72.
Fenton AR, Jongens TA, Holzbaur ELF. Mitochondrial dynamics: shaping and remodeling an organelle network. Curr Opin Cell Biol. 2021;68:28–36.
Chan DC. Mitochondrial dynamics and its involvement in disease. Annu Rev Pathol. 2020;15:235–59.
Wakai T, Harada Y, Miyado K, Kono T. Mitochondrial dynamics controlled by mitofusins define organelle positioning and movement during mouse oocyte maturation. Mol Hum Reprod. 2014;20:1090–1100.
Hoffmann L, Rust MB, Culmsee C. Actin(g) on mitochondria - a role for cofilin1 in neuronal cell death pathways. Biol Chem. 2019;400:1089–97.
Hoffmann L, Waclawczyk MS, Tang S, Hanschmann EM, Gellert M, Rust MB, et al. Cofilin1 oxidation links oxidative distress to mitochondrial demise and neuronal cell death. Cell Death Dis. 2021;12:953.
Zhang Y, Bai J, Cui Z, Li Y, Gao Q, Miao Y, et al. Polyamine metabolite spermidine rejuvenates oocyte quality by enhancing mitophagy during female reproductive aging. Nat Aging. 2023;3:1372–86.
Funding
This work was supported by the National Key Research and Development Program of China (2021YFC2700100) and the National Natural Science Foundation of China (32070836).
Author information
Authors and Affiliations
Contributions
BX and XO conceived and designed the research; SL, YZ, RY, SZ, JB and YM performed the experiments; SL, YZ, XO, QW and BX analyzed the data; SL, XO, QW and BX wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the Institutional Review Board (IRB) of Guangdong Second Provincial General Hospital (2018-SZYX-013), China. The peripheral blood sample was donated by the patient after signing the informed consent at the Center for Reproductive Medicine in Guangdong Second Provincial General Hospital. The patient was informed that her peripheral blood would be used for chromosomal microarray. All mouse experiments were performed in accordance with the Animal Research Institute Committee guidelines of Nanjing Agricultural University, China.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, S., Zhang, Y., Yuan, R. et al. ARHGAP26 deficiency drives the oocyte aneuploidy and early embryonic development failure. Cell Death Differ (2024). https://doi.org/10.1038/s41418-024-01384-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41418-024-01384-5