Abstract
Aims This study aims to understand the experiences of general dental practitioners (GDPs) performing dental extractions for patients at risk of developing medication-related osteonecrosis of the jaw (MRONJ) and to identify the key features of the patients who are referred to secondary care for their extractions.
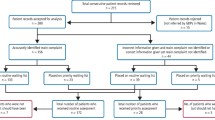
Materials and methods A mixed-method study consisting of quantitative analysis of anonymised electronic referrals and thematic analysis of in-depth telephone interviews with GDPs.
Results In total, 122 electronic referrals for patients at risk of MRONJ were identified. The majority of the referrals contained insufficient information to categorise the patient's risk of developing MRONJ. In-depth telephone interviews with six GDPs were analysed and the themes identified were consequences, difficult decisions, patient awareness and bridging the gap.
Conclusion Our results show that fewer than half of the referrals to secondary care investigated in this study showed a clear indication for secondary care involvement and the quality of the patient information provided was often insufficient to determine the patients' risk of developing MRONJ. Improved local guidance for the management of these patients and a dedicated pathway for their post-operative complications may encourage GDPs to perform more of these dental extractions in practice.
Key points
-
Identifies the key features of patients at risk of MRONJ who are referred to secondary care for dental extractions.
-
Discusses some of the barriers to performing dental extractions for these patients in primary care, including the risks to the patient, the dentist and the difficulties of onward referral if patients develop post-operative complications.
-
Highlights changes to the clinical pathways for patients at risk of MRONJ that could be implemented by the Oral Surgery Managed Clinical Networks.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Scottish Dental Clinical Effectiveness Programme. Oral Health Management of Patients Prescribed Bisphosphonates. 2011. Available at https://www.sdcep.org.uk/published-guidance/bisphosphonates/ (accessed September 2020).
Scottish Dental Clinical Effectiveness Programme. Oral health management of patients at risk of medication-related osteonecrosis of the jaw: Dental clinical guidance. 2017. Available at https://www.dental-referrals.org/wp-content/uploads/2018/04/SDCEP-Oral-Health-Management-of-Patients-at-Risk-of-MRONJ-Guidance-full.pdf (accessed May 2020).
Dyer T A. A five-year evaluation of an NHS dental practice-based specialist minor oral surgery service. Community Dent Health 2013; 30: 219-216.
NHS England. Guide for Commissioning Oral Surgery and Oral Medicine. 2015. Available at https://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/09/guid-comms-oral.pdf (accessed August 2019).
Tanna N, Steel C, Stagnell S, Bailey E. Awareness of medication related osteonecrosis of the jaws (MRONJ) among general dental practitioners. Br Dent J 2017; 222: 121-125.
Sturrock A, Preshaw P M, Hayes C, Wilkes S. General dental practitioners' perceptions of, and attitudes towards, improving patient safety through a multidisciplinary approach to the prevention of medication-related osteonecrosis of the jaw (MRONJ): a qualitative study in the North East of England. BMJ Open 2019; DOI: 10.1136/bmjopen-2019-029951.
Information Comissioner's Office. Anonymisation: managing data protection risk code of practice. 2012. Available at https://ico.org.uk/media/1061/anonymisation-code.pdf (accessed August 2019).
Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health 2019; 11: 589-597.
Ruggiero S L, Mehrotra B, Rosenberg T J, Engroff S L. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg 2004; 62: 527-534.
Wåhlberg H, Valle P C, Malm S, Broderstad A R. Impact of referral templates on the quality of referrals from primary to secondary care: a cluster randomised trial. BMC Health Serv Res 2015; DOI: 10.1186/s12913-015-1017-7.
Patel A, Stagnell S, Eaton K. The appropriateness of oral surgery referrals and treatment in contracted intermediate minor oral surgery practices in East Kent. Br Dent J 2019; 227: 211-216.
Halai T, Yates J M. Assessment of oral surgery referrals from primary care to a regional dental hospital. Oral Surg 2014; 7: 168-176.
Sivarajasingam V, Lewis K, Athwal J, Mort J, Emanuel C, Morgan M Z. Oral surgery referrals at a UK dental hospital in the context of a managed clinical network: a mixed-methods study. Oral Surg 2020; 13: 212-220.
Bader J D, Shugars D A. What do we know about how dentists make caries-related treatment decisions? Community Dent Oral Epidemiol 1997; 25: 97-103.
Fox C. Evidence summary: does dentists' fear have an adverse effect on clinical decision-making? Br Dent J 2010; 209: 181-182.
Sturrock A, Preshaw P M, Hayes C, Wilkes S. Perceptions and attitudes of patients towards medication-related osteonecrosis of the jaw (MRONJ): a qualitative study in England. Br Med J Open 2019; DOI: 10.1136/bmjopen-2018-024376.
Walker A J, Pretis F, Powell-Smith A, Goldacre B. Variation in responsiveness to warranted behaviour change among NHS clinicians: novel implementation of change detection methods in longitudinal prescribing data. Br Med J 2019; DOI: 10.1136/bmj.l5205.
Author information
Authors and Affiliations
Contributions
Sheryl Wilmott: research conception and design, data acquisition, analysis and interpretation and initial draft of manuscript. Julian Yates: research design, analysis and interpretation and critical revision of manuscript. Iain A. Pretty: research design, analysis and interpretation and critical revision of manuscript. All authors gave final approval and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Wilmott, S., Yates, J. & Pretty, I. Dental extractions in primary care for patients at risk of MRONJ. Br Dent J (2021). https://doi.org/10.1038/s41415-021-3674-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-021-3674-8
This article is cited by
-
Oral surgery: top tips for primary care
British Dental Journal (2022)