Abstract
Study design
Prospective observational study.
Objectives
Classification of spinal-cord injury and prediction of independence in activities of daily living (ADL) based on performance evaluations such as upper-limb function have not been reported. Therefore, this study aimed to establish a severity classification and calculate cutoff values for independence in ADL using the Capabilities of Upper Extremity Test (CUE-T) for individuals with cervical spinal-cord injury (CSCI).
Setting
A spinal-cord injury rehabilitation center in Japan.
Methods
This study included individuals with subacute CSCI. Collected data included the CUE-T and Spinal Cord Independence Measure III (SCIM III) scores. The severity classification was used for the hierarchical cluster analysis using the CUE-T. The cutoff values of CUE-T scores for independence in ADL were calculated using an adjustment model with logistic regression analysis. The dependent variable was binary (independent/non-independent) for each SCIM III Self-care item, and the independent variable was CUE-T.
Results
A total of 71 participants were included in the analysis. The severity of upper-limb dysfunction was classified into four categories using CUE-T. Significant differences in upper-limb function and ADL were observed between clusters. The cutoff values for CUE-T score for independence in ADL ranged from 37 to 91 points. All cutoff values showed good results in the internal validation, sensitivity analysis.
Conclusions
This study determined the severity of upper limb function in CSCI and the cutoff values of CUE-T scores for independence in ADL. These results may help set criteria and goals for interventions in the clinical and research fields.
Sponsorship
None.

Similar content being viewed by others
Introduction
Cervical spinal-cord injury (CSCI) is the most common type of spinal-cord injury (SCI) [1, 2]. CSCI has been reported to have a crucial impact on activities of daily living (ADL) owing to severe upper limb dysfunction [3, 4], and various clinical trials [5]. Symptoms of CSCI vary depending on whether the injury is complete or incomplete and the level of injury. Therefore, evaluation of upper-limb dysfunction in CSCI is important for appropriate intervention [6].
The International Standards for Neurological Classification of SCI upper extremity motor score (UEMS); Capabilities of Upper Extremity Test (CUE-T); and Graded Redefined Assessment of Strength, Sensibility, and Prehension (GRASSP) are recommended for evaluation of upper-limb function in individuals with CSCI [6]. These evaluations have been reported to have good reliability, validity, and responsiveness and are used in clinical practice [6,7,8]. UEMS indicates the total manual muscle test score. GRASSP is specific to grasping movements in addition to the neurological findings, and does not include evaluation of bimanual and gross movements. It is difficult to assess upper limb function of the whole CSCI with these evaluations. CUE-T consists of several subtests and requires considerable time for evaluation. However, it evaluates several factors, including fine, gross, and bimanual movements and allows for more detailed performance-based evaluation of upper-limb function in individuals with CSCI [8,9,10].
In clinical practice and trials for stroke, the interpretability of the evaluations has been applied. Severity classification, derived from the Fugl-Meyer Assessment (FMA) for upper limb function evaluation [11], has guided the establishment of adaptation criteria for interventions [12]. Additionally, cutoff values have been calculated for achieving independence in ADL based on assessments of balance ability and upper limb function [13, 14]. Effective improvement in ADL performance can be achieved through the implementation of therapeutic or compensatory interventions for functions that have not met these cutoff values [13, 14]. Therefore, standardized severity classifications and cutoff values in evaluations are useful for establishing intervention details and rehabilitation objectives.
SCI is generally classified as complete or incomplete based on the American Spinal Injury Association (ASIA) Impairment Scale (AIS). However, no classification based on performance evaluations, such as upper-limb function, has been reported. Furthermore, although a prediction model focusing on independence of gait has been validated [15], no prediction model using upper-limb function, which is strongly related to ADL, has been reported. Severity classification and predictors for independence in ADL may be useful because the status of upper-limb function in CSCI is complex.
Therefore, this study aimed to classify the severity of upper-limb dysfunction and calculate the cutoff values for independence in ADL using CUE-T to determine adaptation criteria for interventions, verify effectiveness, and set goals for clinical practice. The severity classifications and cutoff values calculated in this study may facilitate ADL goal setting and intervention selection in clinicians and facilities with limited experience in CSCI. This may contribute to the standardization of upper limb functional rehabilitation for CSCI.
Participants and methods
Participants
This prospective observational study included participants who underwent CSCI rehabilitation at the Chiba Rehabilitation Center in Japan between 2019 and 2023. Subacute CSCI was defined as occurrence of symptoms within 9 months of injury, based on a previous study [16, 17]. The exclusion criteria were as follows: upper-limb dysfunction due to injury other than spinal-cord injury such as fracture, peripheral-nerve injury, or central nervous system disorders such as stroke; difficulty in understanding the examination content due to cognitive or mental dysfunction; and a total CUE-T score of 0.
Data collection
The following data were collected: sex, age, injury duration (days), AIS score, neurological level of injury, traumatic or non-traumatic, CUE-T, UEMS, and Spinal Cord Independence Measure III (SCIM III). CUE-T and other data were collected within 14 days of obtaining consent. Participants were in the subacute phase within 9 months of injury [17], excluding those in the acute phase (within 15 days of injury) [18]. All evaluations were performed by registered occupational therapists trained at Chiba Rehabilitation Center. We used a training video created by Thomas Jefferson University [19]. No blinding was performed during data collection.
Capabilities of Upper Extremity Test
CUE-T is a CSCI-specific upper-limb-function-evaluation tool developed by Tomas Jefferson University [8]. The evaluation items include gross movements, consisting mainly of reaching movements in various directions, and skillful movements (pinch strength, grip strength, speed to manipulate objects), and bimanual movements. Scoring is based on the number of times a specified movement is performed in 30 s, grip strength, and pinch strength, and each item is scored from 0 to 4 points. The total score ranges from 0 to 128 points, including scores for the hand (36 points per side) for fine movements and the side (60 points per side), excluding bimanual movements [8]. Previous studies have reported that CUE-T has good reliability, validity, and responsiveness [8, 10].
International standards for neurological classification of SCI
This evaluation is considered the gold standard for SCI [20]. It is based on the neurological parameters of muscle strength and sensation after spinal-cord injury. Based on the AIS score, injury was classified into complete (A), incomplete (B, C, D), or recovered (E). UEMS is the total manual muscle test score of the elbow flexors (C5), wrist extensors (C6), elbow extensors (C7), finger flexors (C8), and finger abductors (T1) and ranges from 0 to 50 points [20].
Spinal cord independence measure III
This ADL evaluation is specific to SCI. SCIM III evaluates “Self-care,” “Respiration and sphincter management,” and “Mobility.” “Self-care” refers to feeding, dressing, bathing, and grooming. “Respiration and sphincter management” refers to breathing, urination and defecation management, and toilet use. “Mobility” refers to the ability to transfer and move. These are scored based on the participants’ performance. In “Self-care,” scores for feeding, bathing, and grooming range from 0 (needing assistance) to 3 (completely independent). Dressing scores range from 0 (needing assistance) to 4 (completely independent). The total score ranges from 0 to 100 points [21].
Statistical analysis
Severity classification
The hierarchical cluster analysis used the total CUE-T score as an independent variable. The degree of dissimilarity between the participants was calculated using the squared Euclidean distance. Ward’s method was used to define the degree of dissimilarity between the clusters. A dendrogram was created from the results of the hierarchical cluster analysis, and a dividing line was drawn based on the dendrogram to determine the appropriate number of clusters.
To analyze whether the clusters were ordered according to severity and the characteristics of each cluster, we verified the differences in the CUE-T subtests, basic information, upper-limb function, and ADL between the clusters. Differences in the CUE-T subtests were compared between clusters using the percentage of each subtest. Ordinal variables such as sex, AIS score, and neurological level of injury were compared using the χ2 test. Interval variables such as age, injury duration (days), and total CUE-T, UEMS, and SCIM III scores were compared using the Kruskal–Wallis test with post-hoc Bonferroni correction. The effect size was determined using φ and Cramer’s V for ordinal variables and r (Z/√N) for interval variables [22]. The criteria were “0.10 (small)”, “0.30 (medium)”, and “0.50 (large)” [23]. The cutoff scores, which are the thresholds between clusters, were defined as the average of the highest and lowest scores of adjacent clusters [11].
Calculation of cutoff value leading to ADL independence
The SCIM III classification system was used to determine the degrees of independence. Dependence was binary: for feeding, bathing (upper and lower body), dressing (upper and lower body), and grooming 0 and 1 points indicated “non-independent,” whereas for feeding and grooming and bathing (upper and lower body) and dressing (upper and lower body) 2 and 3 points and 2, 3, and 4 points, respectively, indicated “independent.” Logistic regression analysis was performed with binary ADL independence as the dependent variable and the total CUE-T score as the independent variable. The cutoff values were calculated by fitting the obtained regression equation to the adjustment equation reported by Terluin et al. [24]. Sensitivity, specificity, and positive and negative predictive values were calculated for these cutoff values. The cutoff values were validated using the statistical assumptions of the logistic regression analysis. Linearity in the logit transformation of continuous variables was verified using the Box–Tidwell test [25], because only one independent variable was input in the analysis. Strong influence outliers were defined as variables with four or more standard deviations [25]. The goodness of fit of the obtained regression equation was verified using the Hosmer–Lemeshow test. Internal validation of the model was performed using logistic regression analysis. The area under the curve (AUC) of the original data model was compared to that of bootstrapping (a random sample of 1000 from the original data set). Sensitivity analysis was performed by calculating and comparing the cutoff values for the AIS-C and AIS-D only the incomplete-injury groups.
Statistical analyses were performed using SPSS Statistics version 29 (IBM, Armonk, New York), the R4.3.1 rms package, and Microsoft Excel 2019 (Microsoft, Redmond, Washington, USA). Statistical significance was set at p < 0.05.
Sample size
The recommended sample size for segmentation studies, including cluster analysis, is at least 70 × the number of variables [26]. The only variable included in this study was CUE-T. Therefore, the sample size was set at ≥70.
Results
Participants
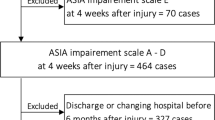
A total of 76 participants were enrolled in this study. Of these, five participants with upper-limb dysfunction due to causes other than SCI or a CUE-T score of 0 were excluded. Finally, 71 participants (60 men and 11 women) were included in the study (Supplement 1). Of these, 9,7,18, and 37 were classified as AIS-A, AIS-B, AIS-C, and AIS-D, respectively (Table 1). The median age of participants was 61.0 years (interquartile range, 49.5–67.0).
Severity classification
Severity was classified into four categories using CUE-T. The categories were in the order of upper-limb function and ADL ability. Based on a dendrogram (Supplement 2) derived from the hierarchical cluster analysis, participants were classified into four clusters as follows: Cluster 1, severe dysfunction; Cluster 2, severe to moderate dysfunction; Cluster 3, moderate to mild dysfunction; and Cluster 4, mild dysfunction. Comparisons of the basic information, upper-limb function, ADL, and CUE-T scores between the clusters are shown in Table 2. Regarding basic information, differences between clusters were observed only for AIS. Significant differences in CUE-T, UEMS, SCIM III, and SCIM III Self-care were observed between all clusters, except between Clusters 3 and 4. The effect size (r) was “large” for all cluster pairs (Supplement 3), and scores did not overlap between clusters. The thresholds between Clusters 1 and 2, 2 and 3, and 3 and 4 were 19, 61, and 98 points, respectively.
A subtest was used to compare the clusters (Fig. 1). In Cluster 1 (severe dysfunction), a good response was obtained for “Pull” (pulling a pan on the table). In Cluster 2 (severe-to-moderate dysfunction), high scores were obtained for “Reach Forward” and “Push,” (extend arm forward in the air or on a table), and a good response was obtained for “Wrist Up” (repetitive flexion and extension of the wrist joint). In Cluster 3 (moderate-to-mild dysfunction), high scores were obtained for “Lift Up” (lifting weight bimanually), “Container,” and “Acquire Release” (grip and release using finger movements). In Cluster 4 (mild dysfunction), high scores were obtained in all subtests.
Calculation of cutoff values for independence in ADL
Logistic regression analysis yielded significant regression equations for all items (p < 0.05). Linearity in the logit transformation of the continuous variables was confirmed, and no strong influence outlier with four or more standard deviations was identified. The results of the Hosmer–Lemeshow test confirmed the goodness of fit (p > 0.05).
The cutoff values calculated using an adjustment formula with regression equations were as follows: feeding, 37 points; bathing the upper body, 91 points; bathing the lower body, 90 points; dressing the upper body, 82 points; dressing the lower body, 81 points; grooming, 60 points.
For all cutoff values, the sensitivity, specificity, positive predictive value and negative predictive value were 0.73–0.96, 0.83–0.98, 0.67–0.96, and 0.83–0.96, respectively (Table 3). In the internal validation, AUC of the model for all cut-off values and that of the model calculated using bootstrapping were similar (Table 3). For the group with incomplete injuries (AIS C-D), the cutoff values calculated using sensitivity analysis were similar (Supplement 4).
Discussion
The severity using the CUE-T was classified into four categories. These were in order of upper limb function and ADL ability. We calculated cutoff values leading to ADL (Feeding, Dressing, Bathing, Grooming) independence. We created a figure (Fig. 2) combined these results. Feeding and Grooming are included in the Cluster 2, Dressing and Bathing are included in the Cluster 3. These findings may serve in using the CUE-T results to assess the status of upper limb function and stage the setting of goals for ADL using the upper limb.
Severity classification
Based on the CUE-T scores, the severity of CSCI upper-limb dysfunction was classified into four categories using hierarchical cluster analysis. In a previous study, a reanalysis was performed by removing duplicate scores between clusters [11]. We analyzed all data, and the results were adopted because no duplicate scores between clusters were observed. The total Functional Independence Measure score ranges from 18 to 126 points and is classified into three categories [27]. This suggests that classification into four clusters was appropriate because the total CUE-T score is higher than the total Functional Independence Measure score.
Significant differences in CUE-T scores between the clusters were observed, and the effect size was “large.” Analysis of the characteristics of each cluster revealed significant differences between clusters in UEMS, which evaluates upper-limb function and SCIM III and SCIM III Self-care, which evaluate ADL, and the effect size was “large.” The CUE-T subtests were analyzed for each cluster. Cluster 1 was characterized by “Pull” movement of the elbow flexors. Cluster 2 was characterized by “Push” movement of the elbow extensors and “Wrist Up”‘ of the wrist extensors. Cluster 3 was characterized by the grip and release movements of the finger extensors and flexors. These results correspond to those for the key muscles in ISNCSCI [20], in the order of degree of injury. A previous study showed good correlation between CUE-T and UEMS [10], implying a link between the CUE-T score and key muscle-related movements. Therefore, we believe that this severity classification reflects the order of difficulty in ADL and neurological findings.
Regarding the participants’ demographics, significant differences in AIS scores were observed between clusters. However, the proportion of individuals with AIS-D was the highest in Clusters 2, 3, and 4. Among ISNCSCI, AIS-D has the best functional status except AIS-E [20]. Thus, the high proportion of AIS-D in multiple clusters suggests that this severity classification reflects the function of the upper limb as a whole in CSCI, including both complete and incomplete injuries. Recently, the number of incomplete CSCI has been increasing [1, 2]. We believe that an analysis focused on incomplete injuries would be more useful in the future, because this study included participants with complete and incomplete injuries.
In stroke, upper limb dysfunction is classified based on performance evaluations such as FMA is utilized in clinical trials [11]. Classifying severity based on performance has the advantage of facilitating the development of specific interventions. ISNCSCI is the gold standard for SCI evaluation, and AIS is widely used [20]. AIS focuses on the neurological aspects and does not include a performance evaluation [20]. The performance status in individuals with incomplete CSCI varies [16], and classification using AIS alone is difficult. Particularly, upper limb function in CSCI is complex and important factor with high hope for recovery [3, 4], and a more detailed classification is necessary. CUE-T can be used to evaluate upper-limb function in individuals with CSCI [8, 10]. Therefore, a severity classification combining CUE-T and ISNCSCI may be more beneficial for determining the upper-limb function and setting the criteria for interventions in individuals with CSCI.
Cutoff values for independence in ADL
The cutoff values of CUE-T scores (total 128 points) for independence in ADL ranged from 37 to 91 points. These cutoff values were the lowest for feeding and the highest for bathing. Except for feeding and grooming, this order of difficulty was different from that in a previous study based on the Rasch analysis of SCIM III [21]. However, the previous study included all individuals with SCI, whereas this study included only individuals with CSCI. Therefore, we consider this to be a new finding because focusing only on the upper-limb function is difficult in a study that includes all types of SCI.
The cutoff values for dressing and bathing were higher. The cutoff values were higher for the upper body in bathing and dressing. Cluster 3, which states that bathing and dressing are independent, is characterized by “Lift Up” (lifting both upper limbs upward). It has been reported that upper limbs lifting movements are limited in individuals with CSCI [28]. We believe this result indicates the difficulty in ADL movements that require lifting the upper limbs. Additionally, it is suggested that upper and lower dressing requires balance ability which makes it more difficult [29].
However, some of the cutoff values had a sensitivity, specificity, negative predictive value, and positive predictive value <80%. The positive predictive value for bathing upper body was 67%. It is assumed that ADL, include many factors, such as balance ability [14, 29]. Furthermore, age-related body composition, motivation, and cognition may influence ADL. In future analyses, including factors other than upper-limb function is necessary to create a tool to accurately predict ADL in individuals with CSCI.
In this study, the number of participants in the independent and non-independent groups based on each SCIM III Self-care item was different. Thus, the cutoff values were determined using an adjustment formula [24]. If the number of participants in either of the two groups separated by an external anchor is <50% of the total number of participants, the proposed method, which corrects for participant bias, is more accurate [24]. In the internal validation, the AUC for bootstrapping and that for the original data did not differ, and the reproducibility of the calculated cutoff values using the model was satisfactory. In the sensitivity analysis, the incomplete-injury group showed similar results. This suggests that the cut-off values calculated in this study are effective.
CUE-T evaluates “activities” in the International Classification of Functioning, Disability, and Health [6]. We proposed a suitable tool for predicting independence in ADL. Currently, there is no such tool in CSCI upper limb function, and the established cutoff values may be beneficial in clinical practice.
Limitations
This study collected data from a single center. Hence, the results may not reflect the findings in the general population. The results of the severity classification and calculated cutoff values may vary depending on the population. In addition, the study included participants within 9 months of injury, and both complete and incomplete injuries were analyzed. ADL varies depending on the duration of the injury and whether the injury is complete or incomplete. Therefore, it is necessary to clarify the duration and severity of the injury in detail. Moreover, in this study, we analyzed only objective data, and we believe that analysis using subjective evaluations is necessary in the future. Finally, data collection was not blinded. This may have introduced bias, and should be addressed in future studies.
Conclusion
In this study, we established a severity classification for upper-limb dysfunction in CSCI and calculated the cutoff values for independence in ADL using CUE-T. The classification reflected the severity of upper-limb dysfunction and ADL in CSCI. The cutoff values showed good results in the internal validation and sensitivity analysis and were effective. Our findings may help apply the CUE-T scores for evaluation of upper-limb function and staging goals for ADL using the upper limb in clinical trials and practice.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available because participants in this study did not consent to sharing their data publicly, but are available from the corresponding author on reasonable request.
Change history
22 July 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41393-024-01017-1
References
Golestani A, Shobeiri P, Sadeghi-Naini M, Jazayeri SB, Maroufi SF, Ghodsi Z, et al. Epidemiology of traumatic spinal cord injury in developing countries from 2009 to 2020: a systematic review and meta-analysis. Neuroepidemiology. 2022;56:219–39.
Miyakoshi N, Suda K, Kudo D, Sakai H, Nakagawa Y, Mikami Y, et al. A nationwide survey on the incidence and characteristics of traumatic spinal cord injury in Japan in 2018. Spinal Cord. 2021;59:626–34.
Simpson LA, Eng JJ, Hsieh JTC, Wolfe DL. The health and life priorities of individuals with spinal cord injury: a systematic review. J Neurotrauma. 2012;29:1548–55.
Anderson KIMD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21:1371–83.
Lu X, Battistuzzo CR, Zoghi M, Galea MP. Effects of training on upper limb function after cervical spinal cord injury: a systematic review. Clin Rehabil. 2015;29:3–13.
Jones LAT, Bryden A, Wheeler TL, Tansey KE, Anderson KD, Beattie MS, et al. Considerations and recommendations for selection and utilization of upper extremity clinical outcome assessments in human spinal cord injury trials. Spinal Cord. 2018;56:414–25.
Lena E, Baroncini I, Pavese C, Musumeci G, Volini S, Masciullo M, et al. Reliability and validity of the international standards for neurological classification of spinal cord injury in patients with non-traumatic spinal cord lesions. Spinal Cord. 2022;60:30–6.
Marino RJ, Sinko R, Bryden A, Backus D, Chen D, Nemunaitis GA, et al. Comparison of responsiveness and minimal clinically important difference of the capabilities of upper extremity test (CUE-T) and the graded redefined assessment of strength, sensibility and prehension (GRASSP). Top Spinal Cord Inj Rehabil. 2018;24:227–38.
Marino RJ, Patrick M, Albright W, Leiby BE, Mulcahey M, Schmidt-Read M, et al. Development of an objective test of upper-limb function in tetraplegia: the capabilities of upper extremity test. Am J Phys Med Rehabil. 2012;91:478–86.
Marino RJ, Kern SB, Leiby B, Schmidt-Read M, Mulcahey MJ. Reliability and validity of the capabilities of upper extremity test (CUE-T) in subjects with chronic spinal cord injury. J Spinal Cord Med. 2015;38:498–504.
Woytowicz EJ, Rietschel JC, Goodman RN, Conroy SS, Sorkin JD, Whitall J, et al. Determining levels of upper extremity movement impairment by applying a cluster analysis to the fugl-meyer assessment of the upper extremity in chronic stroke. Arch Phys Med Rehabil. 2017;98:456–62.
Chen G, Lin T, Wu M, Cai G, Ding Q, Xu J, et al. Effects of repetitive transcranial magnetic stimulation on upper-limb and finger function in stroke patients: a systematic review and meta-analysis of randomized controlled trials. Front Neurol. 2022;13:940467.
Fujita T, Sato A, Yamamoto Y, Otsuki K, Tsuchiya K, Tozato F. Motor function cutoff values for independent dressing in stroke patients. Am J Occup Ther. 2016;70:7003290010p1–7.
Fujita T, Sato A, Tsuchiya K, Ohashi T, Yamane K, Yamamoto Y, et al. Relationship between grooming performance and motor and cognitive functions in stroke patients with receiver operating characteristic analysis. J Stroke Cerebrovasc Dis. 2017;26:2828–33.
Hasegawa T, Uchiyama Y, Uemura K, Harada Y, Sugiyama M, Tanaka H. Physical impairment and walking function required for community ambulation in patients with cervical incomplete spinal cord injury. Spinal Cord. 2014;52:396–9.
Kirshblum S, Snider B, Eren F, Guest J. Characterizing natural recovery after traumatic spinal cord injury. J Neurotrauma. 2021;38:1267–84.
Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D, et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: Spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord. 2007;45:190–205.
Van Middendorp JJ, Hosman AJF, Pouw MH, Van De Meent H. ASIA impairment scale conversion in traumatic SCI: is it related with the ability to walk? A descriptive comparison with functional ambulation outcome measures in 273 patients. Spinal Cord. 2009;47:555–60.
Marino RJ, Thomas Jefferson University: Capabilities of Upper Extremity Test (CUE-T) v1.1 (Jul 2016)—Training Video. 2024. https://jdc.jefferson.edu/rmvideos/1/.
ASIA and ISCoS International Standards Committee. The 2019 revision of the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI)-what’s new? Spinal Cord. 2019;57:815–7.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT, et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord. 2007;45:275–91.
Becker S, Bode M, Brockmann K, Gasser T, Michaelis K, Solbrig S, et al. Cognitive-driven activities of daily living impairment as a predictor for dementia in Parkinson disease: a longitudinal cohort study. Neurology. 2022;99:E2548–60.
Peball M, Krismer F, Knaus HG, Djamshidian A, Werkmann M, Carbone F, et al. Non-motor symptoms in Parkinson’s disease are reduced by nabilone. Ann Neurol. 2020;88:712–22.
Terluin B, Eekhout I, Terwee CB. The anchor-based minimal important change, based on receiver operating characteristic analysis or predictive modeling, may need to be adjusted for the proportion of improved patients. J Clin Epidemiol. 2017;83:90–100.
Rosas S, Hughes RT, Farris M, Lee H, McTyre ER, Plate JF, et al. Cartilage oligomeric matrix protein in patients with osteoarthritis is independently associated with metastatic disease in prostate cancer. Oncotarget. 2019;10:4776–85.
Dolnicar S, Grün B, Leisch F, Schmidt K. Required sample sizes for data-driven market segmentation analyses in tourism. J Travel Res. 2014;53:296–306.
Sandhaug M, Andelic N, Vatne A, Seiler S, Mygland A. Functional level during sub-acute rehabilitation after traumatic brain injury: course and predictors of outcome. Brain Inj. 2010;24:740–7.
Mateo S, Roby-Brami A, Reilly KT, Rossetti Y, Collet C, Rode G. Upper limb kinematics after cervical spinal cord injury: a review. J Neuroeng Rehabil. 2015;12:9.
Fujita T, Nagayama H, Sato A, Yamamoto Y, Yamane K, Otsuki K, et al. Hierarchy of dysfunction related to dressing performance in stroke patients: a path analysis study. PLoS One. 2016;11:e0151162.
Acknowledgements
The authors would like to express their gratitude to the staff at Chiba Rehabilitation Center for their help with data collection and other activities. We are grateful to Editage (www.editage.com) for their English language editing.
Author information
Authors and Affiliations
Contributions
All authors were involved in the research design and preparation of this manuscript. Kazumasa Jimbo, Kousuke Takahama, Tomohiro Yoshimura, Honoka Shiba, Taichi Yasumori, and Naohisa Kikuchi were strongly involved in data collection at the Chiba Rehabilitation Center and in creating the data collection manual. Kazumasa Jimbo, Kazuhiro Miyata, Hiroshi Yuine, and Hideki Shiraishi were strongly involved in the post-collection data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the ethical review committees of the Ibaraki Prefectural University of Health Sciences (approval number 1036) and Chiba Rehabilitation Center (approval number, medical 4-6) based on the Declaration of Helsinki. Participants were informed about the study in writing and were provided with an opt-out option. We certify that all applicable institutional and government regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The Graphic Abstract and the first sentence of the second paragraph in “Cutoff values for independence in ADL” in the Discussion were corrected.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jimbo, K., Miyata, K., Yuine, H. et al. Classification of upper-limb dysfunction severity and prediction of independence in activities of daily living after cervical spinal-cord injury. Spinal Cord 62, 507–513 (2024). https://doi.org/10.1038/s41393-024-01005-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-024-01005-5