Abstract
Study design
Retrospective cohort study.
Objectives
To find minimal clinically important difference (MCID) and minimal detectable change (MDC) of Spinal Cord Ability Ruler (SCAR) in Thai participants with spinal cord injury (SCI).
Setting
Rehabilitation ward at Maharaj Nakorn Chiang Mai Hospital.
Methods
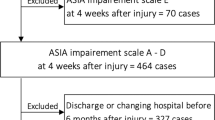
Data of individuals with SCI who were not diagnosed with central cord syndrome and were admitted for the first time for rehabilitation were analyzed. Upper extremities motor score, self-care and mobility items of Spinal Cord Independence Measure version III were collected and used to calculate SCAR difference between data on date of admission and discharge. MCID and MDC were calculated by distribution-based method and categorized for each subgroup according to SCI characteristics.
Results
From data of 311 individuals, MCID of SCAR is approximately 4 for individual with tetraplegia AIS A, B, C; and individual with AIS D at any level, and 2 for individual with paraplegia AIS A, B, C. MDC of SCAR should be 1 for individual with tetraplegia AIS A, B, C; and individual with AIS D at any level and 0.5 for individual with paraplegia AIS A, B, C.
Conclusion
This study provides MCID and MDC of SCAR in each subgroup. These values could be used as a benchmark for clinicians and researchers to determine whether participant has significant improvement or not after receiving an intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bryce TN, Huang V, Escalon MX. Spinal cord injury. In: Cifu DX, Eapen BC, Johns JS, Kowalske K, (eds). Braddom’s physical medicine and rehabilitation. 6th ed. Philadelphia: Elsevier; 2021. p. 1049–1100.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT, et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord. 2007;45:275–91.
Reed R, Mehra M, Kirshblum S, Maier D, Lammertse D, Blight A, et al. Spinal cord ability ruler: an interval scale to measure volitional performance after spinal cord injury. Spinal Cord. 2017;55:730–8.
Bach Jønsson A, Møller Thygesen M, Krogh S, Kasch H. Feasibility of predicting improvements in motor function following SCI using the SCAR outcome measure: a retrospective study. Spinal Cord. 2019;57:966–71.
Pattanakuhar S, Kammuang-lue P, Kovindha A, Komaratat N, Mahachai R, Chotiyarnwong C. Is admission to an SCI specialized rehabilitation facility associated with better functional outcomes? Analysis of data from the Thai Spinal Cord Injury Registry. Spinal Cord. 2019;57:684–91.
Van Middendorp JJ, Pouw MH, Hayes KC, Williams R, Chhabra HS, Putz C, et al. Diagnostic criteria of traumatic central cord syndrome. Part 2: a questionnaire survey among spine specialists. Spinal Cord. 2010;48:657–63.
Kirshblum S, Snider B, Rupp R, Read MS. Updates of the International Standards for Neurologic Classification of Spinal Cord Injury: 2015 and 2019. Phys Med Rehabil Clin N Am. 2020;31:319–30.
Dhand NK, Khatkar MS. Sample size calculator for estimating a single mean. 2020. http://statulator.com/SampleSize/ss1M.html.
Biering-Sørensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, et al. International Spinal Cord Injury Core Data Set (version 2.0)-including standardization of reporting. Spinal Cord. 2017;55:759–64.
Copay AG, Subach BR, Glassman SD, Polly DW Jr., Schuler TC. Understanding the minimum clinically important difference: a review of concepts and methods. Spine J. 2007;7:541–6.
Engel L, Beaton DE, Touma Z. Minimal clinically important difference: a review of outcome measure score interpretation. Rheum Dis Clin North Am. 2018;44:177–88.
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–92.
Ousmen A, Touraine C, Deliu N, Cottone F, Bonnetain F, Efficace F, et al. Distribution- and anchor-based methods to determine the minimally important difference on patient-reported outcome questionnaires in oncology: a structured review. Health Qual Life Outcomes. 2018;16:228.
Hägg O, Fritzell P, Nordwall A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12:12–20.
Beninato M, Fernandes A, Plummer LS. Minimal clinically important difference of the functional gait assessment in older adults. Phys Ther. 2014;94:1594–603.
Scivoletto G, Tamburella F, Laurenza L, Molinari M. The spinal cord independence measure: how much change is clinically significant for spinal cord injury subjects. Disabil Rehabil. 2013;35:1808–13.
Corallo V, Torre M, Ferrara G, Guerra F, Nicosia G, Romanelli E, et al. What do spinal cord injury patients think of their improvement? A study of the minimal clinically important difference of the Spinal Cord Independence Measure III. Eur J Phys Rehabil Med. 2017;53:508–15.
Wyrwich KW, Nienaber NA, Tierney WM, Wolinsky FD. Linking clinical relevance and statistical significance in evaluating intra-individual changes in health-related quality of life. Med Care. 1999;37:469–78.
Storm FA, Petrarca M, Beretta E, Strazzer S, Piccinini L, Maghini C, et al. Minimum clinically important difference of gross motor function and gait endurance in children with motor impairment: a comparison of distribution-based approaches. Biomed Res Int. 2020; https://doi.org/10.1155/2020/2794036.
Kay ED, Deutsch A, Fau - Wuermser LA, Wuermser LA. Predicting walking at discharge from inpatient rehabilitation after a traumatic spinal cord injury. Arch Phys Med Rehabil. 2007;88:745–50.
Burns SP, Golding DG, Rolle WA Jr., Graziani V, Ditunno JF, et al. Recovery of ambulation in motor-incomplete tetraplegia. Arch Phys Med Rehabil. 1997;78:1169–72.
Piovesana A, Senior G. How small is big: sample size and skewness. Assessment. 2018;25:793–800.
Acknowledgements
All authors would like to acknowledge Prof. Dr. Tinakon Wongpakaran for providing statistical advice. SP would like to acknowledge the Swiss Government Excellence Scholarship 2022, postdoctoral fellowship.
Author information
Authors and Affiliations
Contributions
CC designed the research question, collected and analyzed the data, and wrote the preliminary version of the manuscripts. PP designed the research question, analyzed the data, and revised the final version of the manuscripts. SP and ST designed the research question, collected and analyzed the data, wrote the preliminary version, and revised the final version of the manuscripts.
Corresponding author
Ethics declarations
Competing interests
All authors declare no competing interests.
ETHICAL APPROVAL
The authors certify that the protocol of this analysis was approved by the Research Ethics Committee, Faculty of Medicine, Chiang Mai University (Study code REH-2563-07303).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chaidaroon, C., Phinyo, P., Pattanakuhar, S. et al. Minimal clinically important difference (MCID) and minimal detectable change (MDC) of Spinal Cord Ability Ruler (SCAR). Spinal Cord 61, 652–657 (2023). https://doi.org/10.1038/s41393-023-00934-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-023-00934-x