Abstract
Background
The highly oncogenic human papillomavirus (HPV) is associated with numerous cancer types. While the role of viruses in the development of certain cancers is well established, the association between HPV infections and prostate cancer remains a subject of ongoing debate. This study aimed to investigate a potential association of prostate cancer with HPV infections utilizing a case-control study.
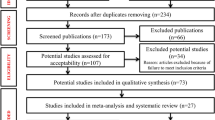
Methods
We extracted data from the Taiwan Longitudinal Health Insurance Database 2010. We retrieved 5137 patients with prostate cancer as cases and a 3:1 ratio of propensity score-matched patients without prostate cancer (15,411 patients) as controls. Multiple logistic regression analyses were carried out to scrutinize the association of prostate cancer with HPV infections while taking into account age, monthly income category, geographic location and urbanization level of the patient’s residence as well as hyperlipidemia, diabetes, hypertension and chronic prostatitis, tobacco use disorder, and alcohol abuse/alcohol dependence syndrome.
Results
The data indicate that out of all sampled patients, 1812 (8.8%) had a prior diagnosis of HPV infections before the index date. Among cases and matched controls, HPV infections were diagnosed in 743 (14.5%) and 1069 (6.9%) patients, respectively. The results from the chi-square test demonstrate that individuals with prostate cancer exhibited a significantly higher incidence rate of HPV infections than their control counterparts (p < 0.001). Furthermore, in comparison to controls, individuals with a history of HPV infections had an adjusted odds ratio of 2.321 (95% CI: 2.097~2.568) for developing prostate cancer. Notably, individuals diagnosed with chronic prostatitis were also more likely to be subsequently diagnosed with prostate cancer (adjusted odds ratio=1.586; 95% CI = 1.338~1.879), which aligns with expectations in this context.
Conclusions
We found prostate cancer to be significantly associated with HPV infections, contributing to the mounting body of evidence indicating a plausible connection between the two.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Data from the National Health Insurance Research Database, now managed by the Health and Welfare Data Science Center (HWDC), can be obtained by interested researchers through a formal application process addressed to the HWDC, Department of Statistics, Ministry of Health and Welfare, Taiwan (https://dep.mohw.gov.tw/DOS/lp-2506-113.html, accessed on 2 January 2022).
References
Lu Y, Li P, Luo G, Liu D, Zou H. Cancer attributable to human papillomavirus infection in China: Burden and trends. Cancer. 2020;126:3719–32.
Senkomago V, Henley SJ, Thomas CC, Mix JM, Markowitz LE, Saraiya M. Human Papillomavirus-attributable cancers - United States, 2012-2016. MMWR Morb Mortal Wkly Rep. 2019;68:724–8.
Bosch FX, Lorincz A, Muñoz N, Meijer CJ, Shah KV. The causal relation between human papillomavirus and cervical cancer. J Clin Pathol. 2002;55:244–65.
Grönberg H. Prostate cancer epidemiology. Lancet. 2003;361:859–64.
Moghoofei M, Keshavarz M, Ghorbani S, Babaei F, Nahand JS, Tavakoli A, et al. Association between human papillomavirus infection and prostate cancer: A global systematic review and meta-analysis. Asia Pac J Clin Oncol. 2019;15:e59–e67.
Korodi Z, Dillner J, Jellum E, Lumme S, Hallmans G, Thoresen S, et al. Human papillomavirus 16, 18, and 33 infections and risk of prostate cancer: a Nordic nested case-control study. Cancer Epidemiol Biomark Prev. 2005;14:2952–5.
Abdolmaleki N, Khodabandehloo M, Ramezanzadeh R, Roshani D. No association between human Papillomavirus and prostate cancer. Int J Cancer Manag. 2018;11:e10049.
Tsydenova IA, Ibragimova MK, Tsyganov MM, Litviakov NV. Human papillomavirus and prostate cancer: systematic review and meta-analysis. Sci Rep. 2023;13:16597.
Dillner J, Knekt P, Boman J, Lehtinen M, Af Geijersstam V, Sapp M, et al. Sero-epidemiological association between human-papillomavirus infection and risk of prostate cancer. Int J Cancer. 1998;75:564–7.
Morka N, Norris JM, Emberton M, Kelly D. Prostate cancer and the human papilloma virus: causative association, role of vaccines, and the impact of the COVID-19 pandemic. Prostate Cancer Prostat Dis. 2022;25:55–7.
Carozzi F, Lombardi FC, Zendron P, Confortini M, Sani C, Bisanzi S, et al. Association of human papillomavirus with prostate cancer: analysis of a consecutive series of prostate biopsies. Int J Biol Markers. 2004;19:257–61.
Glenn WK, Ngan CC, Amos TG, Edwards RJ, Swift J, Lutze-Mann L, et al. High risk human papilloma viruses (HPVs) are present in benign prostate tissues before development of HPV associated prostate cancer. Infect Agent Cancer. 2017;12:46.
Khatami A, Nahand JS, Kiani SJ, Khoshmirsafa M, Moghoofei M, Khanaliha K, et al. Human papilloma virus (HPV) and prostate cancer (PCa): The potential role of HPV gene expression and selected cellular MiRNAs in PCa development. Micro Pathog. 2022;166:105503.
Abidi SH, Bilwani F, Ghias K, Abbas F. Viral etiology of prostate cancer: Genetic alterations and immune response. A literature review. Int J Surg. 2018;52:136–40.
Whitaker NJ, Glenn WK, Sahrudin A, Orde MM, Delprado W, Lawson JS. Human papillomavirus and Epstein Barr virus in prostate cancer: Koilocytes indicate potential oncogenic influences of human papillomavirus in prostate cancer. Prostate. 2013;73:236–41.
Hung SH, Yang TH, Cheng YF, Chen CS, Lin HC. Association of Nasopharynx cancer with human Papillomavirus infections. Cancers. 2023;15:4082.
Mostafaei S, Kazemnejad A, Norooznezhad AH, Mahaki B, Moghoofei M. Simultaneous effects of viral factors of human Papilloma virus and Epstein-Barr virus on progression of breast and thyroid cancers: application of structural equation modeling. Asian Pac J Cancer Prev. 2020;21:1431–9.
Li X, Wei X, Liu X, Wang N, Xu F, Liu X, et al. The analysis of HPV integration sites based on nanopore sequencing and the profiling changes along the course of photodynamic therapy. BMC Cancer. 2023;23:1052.
Chesson HW, Ekwueme DU, Saraiya M, Dunne EF, Markowitz LE. The cost-effectiveness of male HPV vaccination in the United States. Vaccine. 2011;29:8443–50.
Kimura T, Egawa S. Epidemiology of prostate cancer in Asian countries. Int J Urol. 2018;25:524–31.
Vu HL, Sikora AG, Fu S, Kao J. HPV-induced oropharyngeal cancer, immune response and response to therapy. Cancer Lett. 2010;288:149–55.
Lang B, Cao C, Zhao X, Wang Y, Cao Y, Zhou X, et al. Genomic alterations related to HPV infection status in a cohort of Chinese prostate cancer patients. Eur J Med Res. 2023;28:239.
Author information
Authors and Affiliations
Contributions
Concept: SHY, HCL; data acquisition: TCL, HCL; Clinical interpretation: CSD, SHH, SHY; Statistical analysis: TCL; Manuscript drafting: SHY, HCL, CSD, SHH, TCL; Supervision: HCL. All authors have contributed to the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was approved by the institutional review board of Taipei Medical University (TMU-JIRB N202308029).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yin, SH., Chung, SD., Hung, SH. et al. Association of prostate cancer with human papillomavirus infections: a case-control study. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00772-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-023-00772-1