Abstract
Childhood adversity is a prominent predisposing risk factor for latent stress vulnerability, expressed as an elevated likelihood of developing stress-related psychopathology upon subsequent exposure to trauma in adulthood. Sleep disturbances have emerged as one of the most pronounced maladaptive behavioral outcomes of childhood adversity and are also a highly prevalent core feature of stress-related psychopathology, including post-traumatic stress disorder (PTSD). After reviewing the extensive literature supporting these claims, the current review addresses the notion that childhood adversity-induced sleep disturbances may play a causal role in elevating individuals’ stress vulnerability in adulthood. Corroborating this, sleep disturbances that predate adult trauma exposure have been associated with an increased likelihood of developing stress-related psychopathology post-exposure. Furthermore, novel empirical evidence suggests that sleep disturbances, including irregularity of the sleep-wake cycle, mediate the link between childhood adversity and stress vulnerability in adulthood. We also discuss cognitive and behavioral mechanisms through which such a cascade may evolve, highlighting the putative role of impaired memory consolidation and fear extinction. Next, we present evidence to support the contribution of the hypothalamic-pituitary-adrenal (HPA) axis to these associations, stemming from its critical role in stress and sleep regulatory pathways. Childhood adversity may yield bi-directional effects within the HPA stress and sleep axes in which sleep disturbances and HPA axis dysfunction reinforce each other, leading to elevated stress vulnerability. To conclude, we postulate a conceptual path model from childhood adversity to latent stress vulnerability in adulthood and discuss the potential clinical implications of these notions, while highlighting directions for future research.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 13 print issues and online access
$259.00 per year
only $19.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Oh DL, Jerman P, Silverio Marques S, Koita K, Purewal Boparai SK, Burke, et al. Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatr. 2018;18:83.
Bright MA, Knapp C, Hinojosa MS, Alford S, Bonner B. The comorbidity of physical, mental, and developmental conditions associated with childhood adversity: a population based study. Matern Child Health J. 2016;20:843–53.
Cicchetti D. Socioemotional, personality, and biological development: illustrations from a multilevel developmental psychopathology perspective on child maltreatment. Annu Rev Psychol. 2016;67:187–211.
McLaughlin KA. Future directions in childhood adversity and youth psychopathology. J Clin Child Adolesc Psychol. 2016;45:361–82.
Kalmakis KA, Chandler GE. Health consequences of adverse childhood experiences: a systematic review. J Am Assoc Nurse Practitioners. 2015;27:457–65.
Nelson CA, Scott RD, Bhutta ZA, Harris NB, Danese A, Samara M. Adversity in childhood is linked to mental and physical health throughout life. BMJ. 2020;371:m3048
Gilbert LK, Breiding MJ, Merrick MT, Thompson WW, Ford DC, Dhingra SS, et al. Childhood adversity and adult chronic disease: an update from ten states and the District of Columbia, 2010. Am J Prev Med. 2015;48:345–9.
Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004;82:217–25.
Dong M, Giles WH, Felitti VJ, Dube SR, Williams JE, Chapman DP. et al. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation. 2004;110:1761–6.
Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. Am J Psychiatry. 2003;160:1453–60.
Springer KW, Sheridan J, Kuo D, Carnes M. Long-term physical and mental health consequences of childhood physical abuse: results from a large population-based sample of men and women. Child Abus Negl. 2007;31:517–30.
Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9:e1001349.
Heim C, Binder EB. Current research trends in early life stress and depression: review of human studies on sensitive periods, gene-environment interactions, and epigenetics. Exp Neurol. 2012;233:102–11.
Repetti RL, Taylor SE, Seeman TE. Risky families: family social environments and the mental and physical health of offspring. Psychol Bull. 2002;128:330–66.
Mandelli L, Petrelli C, Serretti A. The role of specific early trauma in adult depression: a meta-analysis of published literature. childhood trauma and adult depression. Eur Psychiatry. 2015;30:665–80.
Bremner JD, Southwick SM, Johnson DR, Yehuda R, Charney DS. Childhood physical abuse and combat-related posttraumatic stress disorder in Vietnam veterans. Am J Psychiatry.1993;150:235–9.
Ehlert U. Enduring psychobiological effects of childhood adversity. Psychoneuroendocrinology. 2013;38:1850–7.
Westfall NC, Nemeroff CB. Child abuse and neglect as risk factors for post-traumatic stress disorder. In: Nemeroff CB, Marmar CR, editors. Post-traumatic stress disorder. New York: Oxford Academic; 2018.
Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68:748–66.
Pratchett LC, Yehuda R. Foundations of posttraumatic stress disorder: does early life trauma lead to adult posttraumatic stress disorder? Dev Psychopathol. 2011;23:477–91.
Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biol Psychiatry. 2001;49:1023–39.
Lee RS, Oswald LM, Wand GS. Early life stress as a predictor of co-occurring alcohol use disorder and post-traumatic stress disorder. Alcohol Res. 2018;39:147–59.
McLaughlin KA, Koenen KC, Bromet EJ, Karam EG, Liu H, Petukhova M, et al. Childhood adversities and post-traumatic stress disorder: evidence for stress sensitisation in the World Mental Health Surveys. Br J Psychiatry. 2017;211:280–88.
Giannakopoulos G, Kolaitis G. Sleep problems in children and adolescents following traumatic life events. World J Psychiatry. 2021;11:27–34.
Brown SM, Rodriguez KE, Smith AD, Ricker A, Williamson AA. Associations between childhood maltreatment and behavioral sleep disturbances across the lifespan: a systematic review. Sleep Med Rev. 2022;64:101621.
Schonning V, Sivertsen B, Hysing M, Dovran A, Askeland KG. Childhood maltreatment and sleep in children and adolescents: a systematic review and meta-analysis. Sleep Med Rev. 2022;63:101617.
Kajeepeta S, Gelaye B, Jackson CL, Williams MA. Adverse childhood experiences are associated with adult sleep disorders: a systematic review. Sleep Med. 2015;16:320–30.
Pfaff A, Jud A, Schlarb A. Systematic review on the association between sleep-related hyperarousal and child maltreatment. Sleep Med. 2021;84:219–26.
Fuligni AJ, Chiang JJ, Tottenham N. Sleep disturbance and the long-term impact of early adversity. Neurosci Biobehav Rev. 2021;126:304–13.
Charuvastra A, Cloitre M. Safe enough to sleep: sleep disruptions associated with trauma, posttraumatic stress, and anxiety in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2009;18:877–91.
Agargun MY, Kara H, Ozer OA, Selvi Y, Kiran U, Kiran S. Nightmares and dissociative experiences: the key role of childhood traumatic events. Psychiatry Clin Neurosci. 2003;57:139–45.
Duval M, McDuff P, Zadra A. Nightmare frequency, nightmare distress, and psychopathology in female victims of childhood maltreatment. J Nerv Ment Dis. 2013;201:767–72.
Nielsen T, Carr M, Picard-Deland C, Marquis LP, Saint-Onge K, Blanchette-Carriere C, et al. Early childhood adversity associations with nightmare severity and sleep spindles. Sleep Med. 2019;56:57–65.
Belleville G, Dube-Frenette M, Rousseau A. Sleep disturbances and nightmares in victims of sexual abuse with post-traumatic stress disorder: an analysis of abuse-related characteristics. Eur J Psychotraumatol. 2019;10:1581019.
Mishra AA, Friedman EM, Mihalec-Adkins BP, Evich CD, Christ SL, Marceau K. Childhood maltreatment exposure and physical functional limitations in late adulthood: examining subjective sleep quality in midlife as a mediator. Psychol Health. 2020;35:573–92.
Talvitie E, Hintsanen M, Pulkki-Raback L, Lipsanen J, Merjonen P, Hakulinen C, et al. Adverse childhood environment and self-reported sleep in adulthood: the young finns study. Health Psychol. 2019;38:705–15.
Lind MJ, Aggen SH, Kendler KS, York TP, Amstadter AB. An epidemiologic study of childhood sexual abuse and adult sleep disturbances. Psychol Trauma. 2016;8:198–205.
Greenfield EA, Lee C, Friedman EL, Springer KW. Childhood abuse as a risk factor for sleep problems in adulthood: evidence from a U.S. national study. Ann Behav Med. 2011;42:245–56.
Swanson LM, Hamilton L, Muzik M. The role of childhood trauma and PTSD in postpartum sleep disturbance. J Trauma Stress. 2014;27:689–94.
McNally RJ, Clancy SA. Sleep paralysis in adults reporting repressed, recovered, or continuous memories of childhood sexual abuse. J Anxiety Disord. 2005;19:595–602.
Abrams MP, Mulligan AD, Carleton RN, Asmundson GJ. Prevalence and correlates of sleep paralysis in adults reporting childhood sexual abuse. J Anxiety Disord. 2008;22:1535–41.
Chapman DP, Wheaton AG, Anda RF, Croft JB, Edwards VJ, Liu Y, et al. Adverse childhood experiences and sleep disturbances in adults. Sleep Med. 2011;12:773–9.
Poon CY, Knight BG. Impact of childhood parental abuse and neglect on sleep problems in old age. J Gerontol B Psychol Sci Soc Sci. 2011;66:307–10.
Koskenvuo K, Hublin C, Partinen M, Paunio T, Koskenvuo M. Childhood adversities and quality of sleep in adulthood: a population-based study of 26,000 Finns. Sleep Med. 2010;11:17–22.
Noll JG, Trickett PK, Susman EJ, Putnam FW. Sleep disturbances and childhood sexual abuse. J Pediatr Psychol. 2006;31:469–80.
Pfaff A, Schlarb AA. Consequences of child maltreatment: a glimpse at stress and sleep. J Sleep Res. 2022;31:e13456.
Javakhishvili M, Spatz Widom C. Childhood maltreatment, sleep disturbances, and anxiety and depression: a prospective longitudinal investigation. J Appl Dev Psychol. 2021;77:101351.
Wolke D, Lereya ST. Bullying and parasomnias: a longitudinal cohort study. Pediatrics. 2014;134:e1040–8.
Gregory AM, Caspi A, Moffitt TE, Poulton R. Family conflict in childhood: a predictor of later insomnia. Sleep. 2006;29:1063–7.
Chapman DP, Liu Y, Presley-Cantrell LR, Edwards VJ, Wheaton AG, Perry GS, et al. Adverse childhood experiences and frequent insufficient sleep in 5 U.S. States, 2009: a retrospective cohort study. BMC Public Health. 2013;13:3.
Baiden P, Fallon B, den Dunnen W, Boateng GO. The enduring effects of early-childhood adversities and troubled sleep among Canadian adults: a population-based study. Sleep Med. 2015;16:760–7.
Wang Y, Raffeld MR, Slopen N, Hale L, Dunn EC. Childhood adversity and insomnia in adolescence. Sleep Med. 2016;21:12–8.
Gregory AM, Caspi A, Eley TC, Moffitt TE, Oconnor TG, Poulton R. Prospective longitudinal associations between persistent sleep problems in childhood and anxiety and depression disorders in adulthood. J Abnorm Child Psychol. 2005;33:157–63.
Langevin R, Hebert M, Guidi E, Bernard-Bonnin AC, Allard-Dansereau C. Sleep problems over a year in sexually abused preschoolers. Paediatr Child Health. 2017;22:273–76.
Goldston DB, Turnquist DC, Knutson JF. Presenting problems of sexually abused girls receiving psychiatric services. J Abnorm Psychol. 1989;98:314–7.
Bader K, Schafer V, Schenkel M, Nissen L, Schwander J. Adverse childhood experiences associated with sleep in primary insomnia. J Sleep Res. 2007;16:285–96.
Bader K, Schafer V, Schenkel M, Nissen L, Kuhl HC, Schwander J. Increased nocturnal activity associated with adverse childhood experiences in patients with primary insomnia. J Nerv Ment Dis. 2007;195:588–95.
Fusco RA. Sleep in young adults: comparing foster care alumni to a low-income sample. J Child Fam Stud. 2020;29:493–501.
Brindle RC, Cribbet MR, Samuelsson LB, Gao C, Frank E, Krafty RT, et al. The relationship between childhood trauma and poor sleep health in adulthood. Psychosom Med. 2018;80:200–07.
Armitage R, Flynn H, Hoffmann R, Vazquez D, Lopez J, Marcus S. Early developmental changes in sleep in infants: the impact of maternal depression. Sleep. 2009;32:693–6.
Schafer V, Bader K. Relationship between early-life stress load and sleep in psychiatric outpatients: a sleep diary and actigraphy study. Stress Health. 2013;29:177–89.
Dube SR, Anda RF, Felitti VJ, Edwards VJ, Croft JB. Adverse childhood experiences and personal alcohol abuse as an adult. Addict Behav. 2002;27:713–25.
Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics. 2003;111:564–72.
Anda RF, Brown DW, Felitti VJ, Bremner JD, Dube SR, Giles WH. Adverse childhood experiences and prescribed psychotropic medications in adults. Am J Prev Med. 2007;32:389–94.
Germain A, Buysse DJ, Nofzinger E. Sleep-specific mechanisms underlying posttraumatic stress disorder: integrative review and neurobiological hypotheses. Sleep Med Rev. 2008;12:185–95.
Germain A. Sleep disturbances as the hallmark of PTSD: where are we now? Am J Psychiatry. 2013;170:372–82.
Mellman TA, Hipolito MM. Sleep disturbances in the aftermath of trauma and posttraumatic stress disorder. CNS Spectr. 2006;11:611–5.
Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Med Rev. 2008;12:169–84.
Weber FC, Wetter TC. The many faces of sleep disorders in post-traumatic stress disorder: an update on clinical features and treatment. Neuropsychobiology. 2022;81:85–97.
Zhang Y, Ren R, Sanford LD, Yang L, Zhou J, Zhang J, et al. Sleep in posttraumatic stress disorder: a systematic review and meta-analysis of polysomnographic findings. Sleep Med Rev. 2019;48:101210.
Harvey AG, Jones C, Schmidt DA. Sleep and posttraumatic stress disorder: a review. Clin Psychol Rev. 2003;23:377–407.
Milanak ME, Zuromski KL, Cero I, Wilkerson AK, Resnick HS, Kilpatrick DG. Traumatic event exposure, posttraumatic stress disorder, and sleep disturbances in a National Sample of U.S. Adults. J Trauma Stress. 2019;32:14–22.
American Psychiatric Association, Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American Psychiatric Association; 2013.
Cox RC, Tuck BM, Olatunji BO. Sleep disturbance in posttraumatic stress disorder: epiphenomenon or causal factor? Curr Psychiatry Rep. 2017;19:22.
Kobayashi I, Boarts JM, Delahanty DL. Polysomnographically measured sleep abnormalities in PTSD: a meta-analytic review. Psychophysiology. 2007;44:660–9.
Casement MD, Harrington KM, Miller MW, Resick PA. Associations between Pittsburgh Sleep Quality Index factors and health outcomes in women with posttraumatic stress disorder. Sleep Med. 2012;13:752–8.
Martindale SL, Morissette SB, Rowland JA, Dolan SL. Sleep quality affects cognitive functioning in returning combat veterans beyond combat exposure, PTSD, and mild TBI history. Neuropsychology. 2017;31:93–104.
Giosan C, Malta LS, Wyka K, Jayasinghe N, Evans S, Difede J, et al. Sleep disturbance, disability, and posttraumatic stress disorder in utility workers. J Clin Psychol. 2015;71:72–84.
Shaffer JA, Kronish IM, Burg M, Clemow L, Edmondson D. Association of acute coronary syndrome-induced posttraumatic stress disorder symptoms with self-reported sleep. Ann Behav Med. 2013;46:349–57.
Qu Z, Wang X, Tian D, Zhao Y, Zhang Q, He H, et al. Posttraumatic stress disorder and depression among new mothers at 8 months later of the 2008 Sichuan earthquake in China. Arch Women’s Ment Health. 2012;15:49–55.
Troxel WM, Germain A. Insecure attachment is an independent correlate of objective sleep disturbances in military veterans. Sleep Med. 2011;12:860–5.
Swinkels CM, Ulmer CS, Beckham JC, Buse N, Calhoun PS. The association of sleep duration, mental health, and health risk behaviors among U.S. Afghanistan/Iraq Era Veterans. Sleep. 2013;36:1019–25.
Sinha SS. Trauma-induced insomnia: a novel model for trauma and sleep research. Sleep Med Rev. 2016;25:74–83.
Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and PTSD: a critical review of the empirical literature. J Anxiety Disord. 2010;24:1–15.
Werner GG, Riemann D, Ehring T. Fear of sleep and trauma-induced insomnia: a review and conceptual model. Sleep Med Rev. 2021;55:101383.
Roberge EM, Bryan CJ. An integrated model of chronic trauma-induced insomnia. Clin Psychol Psychother. 2021;28:79–92.
Richards A, Kanady JC, Neylan TC. Sleep disturbance in PTSD and other anxiety-related disorders: an updated review of clinical features, physiological characteristics, and psychological and neurobiological mechanisms. Neuropsychopharmacology. 2020;45:55–73.
Gehrman P, Seelig AD, Jacobson IG, Boyko EJ, Hooper TI, Gackstetter GD, et al. Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment. Sleep. 2013;36:1009–18.
Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as predictor versus outcome of PTSD and depression among Iraq combat veterans. J Clin Psychol. 2011;67:1240–58.
Koffel E, Polusny MA, Arbisi PA, Erbes CR. Pre-deployment daytime and nighttime sleep complaints as predictors of post-deployment PTSD and depression in National Guard troops. J Anxiety Disord. 2013;27:512–9.
Wang HE, Campbell-Sills L, Kessler RC, Sun X, Heeringa SG, Nock MK, et al. Pre-deployment insomnia is associated with post-deployment post-traumatic stress disorder and suicidal ideation in US Army soldiers. Sleep. 2019;42:zsy229.
Acheson DT, Kwan B, Maihofer AX, Risbrough VB, Nievergelt CM, Clark JW, et al. Sleep disturbance at pre-deployment is a significant predictor of post-deployment re-experiencing symptoms. Eur J Psychotraumatol. 2019;10:1679964.
Bryant RA, Creamer M, O'Donnell M, Silove D, McFarlane AC. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep. 2010;33:69–74.
Elliott R, McKinley S, Fien M, Elliott D. Posttraumatic stress symptoms in intensive care patients: an exploration of associated factors. Rehabil Psychol. 2016;61:141–50.
Fan F, Zhou Y, Liu X. Sleep disturbance predicts posttraumatic stress disorder and depressive symptoms: a cohort study of chinese adolescents. J Clin Psychiatry. 2017;78:882–88.
Wang D, Zhao J, Zhai S, Ye H, Bu L, Fan F. Does sleep disturbance predicts posttraumatic stress disorder and depression among college students during COVID-19 lockdown? A longitudinal survey. Front Public Health. 2022;10:986934.
Slavish DC, Briggs M, Fentem A, Messman BA, Contractor AA. Bidirectional associations between daily PTSD symptoms and sleep disturbances: a systematic review. Sleep Med Rev. 2022;63:101623.
Biggs QM, Ursano RJ, Wang J, Wynn GH, Carr RB, Fullerton CS. Post traumatic stress symptom variation associated with sleep characteristics. BMC Psychiatry. 2020;20:174.
Werner GG, Göhre I, Takano K, Ehring T, Wittekind CE, Stefanovic M. Temporal associations between trauma-related sleep disturbances and PTSD symptoms: An experience sampling study. Psychol Trauma. 2022. https://doi.org/10.1037/tra0001386. Online ahead of print.
Short NA, Allan NP, Schmidt NB. Sleep disturbance as a predictor of affective functioning and symptom severity among individuals with PTSD: an ecological momentary assessment study. Behav Res Ther. 2017;97:146–53.
DeViva JC, Rosen MI, Cooney NL, Black AC. Ecological momentary assessment of sleep and PTSD symptoms in a veteran sample. Psychol Trauma. 2020;12:186–92.
Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med. 2005;6:23–27.
Roth T. Comorbid insomnia: current directions and future challenges. Am J Manag Care. 2009;15:S6.
Davies SK, Ang JE, Revell VL, Holmes B, Mann A, Robertson FP, et al. Effect of sleep deprivation on the human metabolome. Proc Natl Acad Sci. 2014;111:10761–66.
Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 2010;33:585–92.
McEwen BS, Karatsoreos IN. Sleep deprivation and circadian disruption stress, allostasis, and allostatic load. Sleep Med Clin. 2022;17:253–62.
Chattu VK, Manzar MD, Kumary S, Burman D, Spence DW, Pandi-Perumal SR. The global problem of insufficient sleep and its serious public health implications. Healthcare (Basel). 2018;7:1.
Medic G, Wille M, Hemels ME. Short-and long-term health consequences of sleep disruption. Nat Sci sleep. 2017;9:151.
Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, et al. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. 2016;142:969–90.
Sun J, Wang M, Yang L, Zhao M, Bovet P, Xi B. Sleep duration and cardiovascular risk factors in children and adolescents: a systematic review. Sleep Med Rev. 2020;53:101338.
Spilsbury JC. Sleep as a mediator in the pathway from violence-induced traumatic stress to poorer health and functioning: a review of the literature and proposed conceptual model. Behav Sleep Med. 2009;7:223–44.
Kendall-Tackett K. The health effects of childhood abuse: four pathways by which abuse can influence health. Child Abus Negl. 2002;26:715–29.
Fairholme CR, Manber R. Sleep, emotions, and emotion regulation: An overview. In: Babson KA, Feldner MT, editors. Sleep and affect: Assessment, theory, and clinical implications. Elsevier Academic Press; 2015. 45–61.
Walker MP. The role of sleep in cognition and emotion. Ann N. Y Acad Sci. 2009;1156:168–97.
Walker MP, van der Helm E. Overnight therapy? The role of sleep in emotional brain processing. Psychol Bull. 2009;135:731–48.
Tempesta D, Socci V, De Gennaro L, Ferrara M. Sleep and emotional processing. Sleep Med Rev. 2018;40:183–95.
Chambers AM. The role of sleep in cognitive processing: focusing on memory consolidation. Wiley Interdiscip Rev Cogn Sci. 2017;8. https://doi.org/10.1002/wcs.1433.
Sara SJ. Sleep to remember. J Neurosci. 2017;37:457–63.
Galvan A. The need for sleep in the adolescent brain. Trends Cogn Sci. 2020;24:79–8.
Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Med Rev. 2012;16:129–36.
Poe GR. Sleep is for forgetting. J Neurosci. 2017;37:464–73.
Feld GB, Born J. Sculpting memory during sleep: concurrent consolidation and forgetting. Curr Opin Neurobiol. 2017;44:20–27.
Kim T, Kim S, Kang J, Kwon M, Lee SH. The common effects of sleep deprivation on human long-term memory and cognitive control processes. Front Neurosci. 2022;16:883848.
Vandekerckhove M, Wang YL. Emotion, emotion regulation and sleep: an intimate relationship. AIMS Neurosci. 2018;5:1–17.
Augusti EM, Melinder A. Maltreatment is associated with specific impairments in executive functions: a pilot study. J Trauma Stress. 2013;26:780–3.
DePrince AP, Weinzierl KM, Combs MD. Executive function performance and trauma exposure in a community sample of children. Child Abus Negl. 2009;33:353–61.
Nolin P, Ethier L. Using neuropsychological profiles to classify neglected children with or without physical abuse. Child Abus Negl. 2007;31:631–43.
Skowron EA, Cipriano-Essel E, Gatzke-Kopp LM, Teti DM, Ammerman RT. Early adversity, RSA, and inhibitory control: evidence of children’s neurobiological sensitivity to social context. Dev Psychobiol. 2014;56:964–78.
Kim J, Cicchetti D. Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. J Child Psychol Psychiatry. 2010;51:706–16.
Kavanaugh BC, Dupont-Frechette JA, Jerskey BA, Holler KA. Neurocognitive deficits in children and adolescents following maltreatment: neurodevelopmental consequences and neuropsychological implications of traumatic stress. Appl Neuropsychol Child. 2017;6:64–78.
Kavanaugh B, Holler K. Brief report: neurocognitive functioning in adolescents following childhood maltreatment and evidence for underlying planning & organizational deficits. Child Neuropsychol. 2015;21:840–8.
Mothes L, Kristensen CH, Grassi-Oliveira R, Fonseca RP, de Lima A II, Irigaray TQ. Childhood maltreatment and executive functions in adolescents. Child Adolesc Ment Health. 2015;20:56–62.
Spann MN, Mayes LC, Kalmar JH, Guiney J, Womer FY, Pittman B, et al. Childhood abuse and neglect and cognitive flexibility in adolescents. Child Neuropsychol. 2012;18:182–9.
Gould F, Clarke J, Heim C, Harvey PD, Majer M, Nemeroff CB. The effects of child abuse and neglect on cognitive functioning in adulthood. J Psychiatr Res. 2012;46:500–6.
Nikulina V, Widom CS. Child maltreatment and executive functioning in middle adulthood: a prospective examination. Neuropsychology. 2013;27:417–27.
Wells TT, Vanderlind WM, Selby EA, Beevers CG. Childhood abuse and vulnerability to depression: cognitive scars in otherwise healthy young adults. Cogn Emot. 2014;28:821–33.
Tinajero R, Williams PG, Cribbet MR, Rau HK, Silver MA, Bride DL, et al. Reported history of childhood trauma and stress-related vulnerability: associations with emotion regulation, executive functioning, daily hassles and pre-sleep arousal. Stress Health. 2020;36:405–18.
Lovallo WR, Farag NH, Sorocco KH, Acheson A, Cohoon AJ, Vincent AS. Early life adversity contributes to impaired cognition and impulsive behavior: studies from the Oklahoma family health patterns project. Alcohol Clin Exp Res. 2013;37:616–23.
Cross D, Fani N, Powers A, Bradley B. Neurobiological development in the context of childhood trauma. Clin Psychol. 2017;24:111–24.
Williams PG, Suchy Y, Rau HK. Individual differences in executive functioning: implications for stress regulation. Ann Behav Med. 2009;37:126–40.
Williams PG, Thayer JF. Executive functioning and health: introduction to the special series. Ann Behav Med. 2009;37:101–5.
Jennissen S, Holl J, Mai H, Wolff S, Barnow S. Emotion dysregulation mediates the relationship between child maltreatment and psychopathology: a structural equation model. Child Abus Negl. 2016;62:51–62.
Heleniak C, Jenness JL, Stoep AV, McCauley E, McLaughlin KA. Childhood maltreatment exposure and disruptions in emotion regulation: a transdiagnostic pathway to adolescent internalizing and externalizing psychopathology. Cogn Ther Res. 2016;40:394–415.
Feld GB, Born J. Neurochemical mechanisms for memory processing during sleep: basic findings in humans and neuropsychiatric implications. Neuropsychopharmacology. 2020;45:31–44.
Brodt S, Inostroza M, Niethard N, Born J. Sleep-A brain-state serving systems memory consolidation. Neuron. 2023;111:1050–75.
Klinzing JG, Niethard N, Born J. Mechanisms of systems memory consolidation during sleep. Nat Neurosci. 2019;22:1598–610.
Dudai Y, Karni A, Born J. The consolidation and transformation of memory. Neuron. 2015;88:20–32.
Pace-Schott EF, Germain A, Milad MR. Effects of sleep on memory for conditioned fear and fear extinction. Psychol Bull. 2015;141:835–57.
Albrecht A, Stork O. Circadian rhythms in fear conditioning: an overview of behavioral, brain system, and molecular interactions. Neural Plast. 2017;2017:3750307.
Schenker MT, Ney LJ, Miller LN, Felmingham KL, Nicholas CL, Jordan AS. Sleep and fear conditioning, extinction learning and extinction recall: a systematic review and meta-analysis of polysomnographic findings. Sleep Med Rev. 2021;59:101501.
Murkar ALA, De Koninck J. Consolidative mechanisms of emotional processing in REM sleep and PTSD. Sleep Med Rev. 2018;41:173–84.
Grasser LR, Jovanovic T. Safety learning during development: implications for development of psychopathology. Behav Brain Res. 2021;408:113297.
Marusak HA, Hehr A, Bhogal A, Peters C, Iadipaolo A, Rabinak CA. Alterations in fear extinction neural circuitry and fear-related behavior linked to trauma exposure in children. Behav Brain Res. 2021;398:112958.
Zuj DV, Palmer MA, Lommen MJ, Felmingham KL. The centrality of fear extinction in linking risk factors to PTSD: a narrative review. Neurosci Biobehav Rev. 2016;69:15–35.
Perogamvros L, Castelnovo A, Samson D, Dang-Vu TT. Failure of fear extinction in insomnia: an evolutionary perspective. Sleep Med Rev. 2020;51:101277.
Jarczok M, Lange S, Domhardt M, Baumeister H, Jud A. Can You Sleep? - Effect of Retrospective recall of child maltreatment on sleep parameters and the mediating role of psychological distress among students of two German Universities. Nat Sci Sleep. 2022;14:1299–310.
McPhie ML, Weiss JA, Wekerle C. Psychological distress as a mediator of the relationship between childhood maltreatment and sleep quality in adolescence: results from the Maltreatment and Adolescent Pathways (MAP) longitudinal study. Child Abus Negl. 2014;38:2044–52.
John-Henderson NA, Williams SE, Brindle RC, Ginty AT. Changes in sleep quality and levels of psychological distress during the adaptation to university: the role of childhood adversity. Br J Psychol. 2018;109:694–707.
Hanson MD, Chen E. Daily stress, cortisol, and sleep: the moderating role of childhood psychosocial environments. Health Psychol. 2010;29:394–402.
Azza Y, Grueschow M, Karlen W, Seifritz E, Kleim B. How stress affects sleep and mental health: nocturnal heart rate increases during prolonged stress and interacts with childhood trauma exposure to predict anxiety. Sleep. 2020;43:zsz310.
Wang YS, Friedman AL, Jakubowski KP, Wescott DL, Iyiewuare P, Feldman JS, et al. Childhood maltreatment reports in adult seasonal affective disorder: associations with sleep disturbances, maladaptive cognitions, and brooding. J Affect Disord. 2021;288:31–40.
Magal N, Rab SL, Goldstein P, Simon L, Jiryis T, Admon R. Predicting chronic stress among healthy females using daily-life physiological and lifestyle features from wearable sensors. Chronic Stress (Thousand Oaks). 2022;6:24705470221100987.
Smeets T, Cornelisse S, Quaedflieg CW, Meyer T, Jelicic M, Merckelbach H. Introducing the Maastricht Acute Stress Test (MAST): a quick and non-invasive approach to elicit robust autonomic and glucocorticoid stress responses. Psychoneuroendocrinology.2012;37:1998–2008.
Simon L, Rab SL, Goldstein P, Magal N, Admon R. Multi-trajectory analysis uncovers latent associations between psychological and physiological acute stress response patterns. Psychoneuroendocrinology. 2022;145:105925.
Lemola S, Ledermann T, Friedman EM. Variability of sleep duration is related to subjective sleep quality and subjective well-being: an actigraphy study. PLoS One. 2013;8:e71292.
Mezick EJ, Matthews KA, Hall M, Kamarck TW, Buysse DJ, Owens JF, et al. Intra-individual variability in sleep duration and fragmentation: associations with stress. Psychoneuroendocrinology. 2009;34:1346–54.
Veeramachaneni K, Slavish DC, Dietch JR, Kelly K, Taylor DJ. Intraindividual variability in sleep and perceived stress in young adults. Sleep Health. 2019;5:572–79.
Lemola S, Schwarz B, Siffert A. Interparental conflict and early adolescents' aggression: is irregular sleep a vulnerability factor? J Adolesc. 2012;35:97–105.
Rab SL, Admon R. Parsing inter- and intra-individual variability in key nervous system mechanisms of stress responsivity and across functional domains. Neurosci Biobehav Rev. 2021;120:550–64.
Foley P, Kirschbaum C. Human hypothalamus-pituitary-adrenal axis responses to acute psychosocial stress in laboratory settings. Neurosci Biobehav Rev. 2010;35:91–6.
Herman JP, McKlveen JM, Ghosal S, Kopp B, Wulsin A, Makinson R, et al. Regulation of the Hypothalamic-Pituitary-Adrenocortical Stress Response. Compr Physiol. 2016;6:603–21.
Joels M, Baram TZ. The neuro-symphony of stress. Nat Rev Neurosci. 2009;10:459–66.
Carlson SM, Moses LJ, Claxton LJ. Individual differences in executive functioning and theory of mind: an investigation of inhibitory control and planning ability. J Exp Child Psychol. 2004;87:299–319.
Schumacher S, Niemeyer H, Engel S, Cwik JC, Laufer S, Klusmann H, et al. HPA axis regulation in posttraumatic stress disorder: a meta-analysis focusing on potential moderators. Neurosci Biobehav Rev. 2019;100:35–57.
Speer KE, Semple S, Naumovski N, D'Cunha NM, McKune AJ. HPA axis function and diurnal cortisol in post-traumatic stress disorder: a systematic review. Neurobiol Stress. 2019;11:100180.
Zorn JV, Schur RR, Boks MP, Kahn RS, Joels M, Vinkers CH. Cortisol stress reactivity across psychiatric disorders: a systematic review and meta-analysis. Psychoneuroendocrinology. 2017;77:25–36.
Stetler C, Miller GE. Depression and hypothalamic-pituitary-adrenal activation: a quantitative summary of four decades of research. Psychosom Med. 2011;73:114–26.
Ehlert U, Gaab J, Heinrichs M. Psychoneuroendocrinological contributions to the etiology of depression, posttraumatic stress disorder, and stress-related bodily disorders: the role of the hypothalamus-pituitary-adrenal axis. Biol Psychol. 2001;57:141–52.
Carroll D, Ginty AT, Whittaker AC, Lovallo WR, de Rooij SR. The behavioural, cognitive, and neural corollaries of blunted cardiovascular and cortisol reactions to acute psychological stress. Neurosci Biobehav Rev. 2017;77:74–86.
Heim C, Newport DJ, Wagner D, Wilcox MM, Miller AH, Nemeroff CB. The role of early adverse experience and adulthood stress in the prediction of neuroendocrine stress reactivity in women: a multiple regression analysis. Depress Anxiety. 2002;15:117–25.
Dreger LC, Kozyrskyj AL, HayGlass KT, Becker AB, MacNeil BJ. Lower cortisol levels in children with asthma exposed to recurrent maternal distress from birth. J Allergy Clin Immunol. 2010;125:116–22.
Essex MJ, Klein MH, Cho E, Kalin NH. Maternal stress beginning in infancy may sensitize children to later stress exposure: effects on cortisol and behavior. Biol Psychiatry. 2002;52:776–84.
Halligan SL, Herbert J, Goodyer IM, Murray L. Exposure to postnatal depression predicts elevated cortisol in adolescent offspring. Biol Psychiatry. 2004;55:376–81.
Ashman SB, Dawson G, Panagiotides H, Yamada E, Wilkinson CW. Stress hormone levels of children of depressed mothers. Dev Psychopathol. 2002;14:333–49.
Bosch NM, Riese H, Reijneveld SA, Bakker MP, Verhulst FC, Ormel J, et al. Timing matters: long term effects of adversities from prenatal period up to adolescence on adolescents' cortisol stress response. The TRAILS study. Psychoneuroendocrinology. 2012;37:1439–47.
Harkness KL, Stewart JG, Wynne-Edwards KE. Cortisol reactivity to social stress in adolescents: role of depression severity and child maltreatment. Psychoneuroendocrinology. 2011;36:173–81.
Mielock AS, Morris MC, Rao U. Patterns of cortisol and alpha-amylase reactivity to psychosocial stress in maltreated women. J Affect Disord. 2017;209:46–52.
Taylor SE, Lerner JS, Sage RM, Lehman BJ, Seeman TE. Early environment, emotions, responses to stress, and health. J Personal. 2004;72:1365–93.
Armbruster D, Mueller A, Strobel A, Lesch KP, Brocke B, Kirschbaum C. Children under stress - COMT genotype and stressful life events predict cortisol increase in an acute social stress paradigm. Int J Neuropsychopharmacol. 2012;15:1229–39.
Peckins MK, Susman EJ, Negriff S, Noll J, Trickett PK. Cortisol profiles: a test for adaptive calibration of the stress response system in maltreated and nonmaltreated youth. Dev Psychopathol. 2015;27:1461–70.
Ouellet-Morin I, Odgers CL, Danese A, Bowes L, Shakoor S, Papadopoulos AS, et al. Blunted cortisol responses to stress signal social and behavioral problems among maltreated/bullied 12-year-old children. Biol Psychiatry. 2011;70:1016–23.
Ouellet-Morin I, Danese A, Bowes L, Shakoor S, Ambler A, Pariante CM, et al. A discordant monozygotic twin design shows blunted cortisol reactivity among bullied children. J Am Acad Child Adolesc Psychiatry. 2011;50:574–82e3.
Carnuta M, Crisan LG, Vulturar R, Opre A, Miu AC. Emotional non-acceptance links early life stress and blunted cortisol reactivity to social threat. Psychoneuroendocrinology. 2015;51:176–87.
Carpenter LL, Shattuck TT, Tyrka AR, Geracioti TD, Price LH. Effect of childhood physical abuse on cortisol stress response. Psychopharmacol (Berl). 2011;214:367–75.
Elzinga BM, Roelofs K, Tollenaar MS, Bakvis P, van Pelt J, Spinhoven P. Diminished cortisol responses to psychosocial stress associated with lifetime adverse events a study among healthy young subjects. Psychoneuroendocrinology. 2008;33:227–37.
MacMillan HL, Georgiades K, Duku EK, Shea A, Steiner M, Niec A, et al. Cortisol response to stress in female youths exposed to childhood maltreatment: results of the youth mood project. Biol Psychiatry. 2009;66:62–8.
McLaughlin KA, Sheridan MA, Tibu F, Fox NA, Zeanah CH, Nelson CA 3rd. Causal effects of the early caregiving environment on development of stress response systems in children. Proc Natl Acad Sci USA. 2015;112:5637–42.
Trickett PK, Gordis E, Peckins MK, Susman EJ. Stress reactivity in maltreated and comparison male and female young adolescents. Child Maltreat. 2014;19:27–37.
Voellmin A, Winzeler K, Hug E, Wilhelm FH, Schaefer V, Gaab J, et al. Blunted endocrine and cardiovascular reactivity in young healthy women reporting a history of childhood adversity. Psychoneuroendocrinology. 2015;51:58–67.
Lovallo WR, Cohoon AJ, Acheson A, Sorocco KH, Vincent AS. Blunted stress reactivity reveals vulnerability to early life adversity in young adults with a family history of alcoholism. Addiction.2019;114:798–806.
Trickett PK, Noll JG, Susman EJ, Shenk CE, Putnam FW. Attenuation of cortisol across development for victims of sexual abuse. Dev Psychopathol. 2010;22:165–75.
Carpenter LL, Carvalho JP, Tyrka AR, Wier LM, Mello AF, Mello MF, et al. Decreased adrenocorticotropic hormone and cortisol responses to stress in healthy adults reporting significant childhood maltreatment. Biol Psychiatry. 2007;62:1080–7.
Bernard K, Frost A, Bennett CB, Lindhiem O. Maltreatment and diurnal cortisol regulation: a meta-analysis. Psychoneuroendocrinology. 2017;78:57–67.
Brindle RC, Pearson A, Ginty AT. Adverse childhood experiences (ACEs) relate to blunted cardiovascular and cortisol reactivity to acute laboratory stress: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2022;134:104530.
Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10:434–45.
Bunea IM, Szentagotai-Tatar A, Miu AC. Early-life adversity and cortisol response to social stress: a meta-analysis. Transl Psychiatry. 2017;7:1274.
Koss KJ, Gunnar MR. Annual research review: early adversity, the hypothalamic-pituitary-adrenocortical axis, and child psychopathology. J Child Psychol Psychiatry. 2018;59:327–46.
Schar S, Murner-Lavanchy I, Schmidt SJ, Koenig J, Kaess M. Child maltreatment and hypothalamic-pituitary-adrenal axis functioning: a systematic review and meta-analysis. Front Neuroendocrinol. 2022;66:100987.
Tarullo AR, Gunnar MR. Child maltreatment and the developing HPA axis. Hormon Behav. 2006;50:632–9.
Glaser D. Child abuse and neglect and the brain–a review. J Child Psychol Psychiatry. 2000;41:97–116.
van Bodegom M, Homberg JR, Henckens M. Modulation of the hypothalamic-pituitary-adrenal axis by early life stress exposure. Front Cell Neurosci. 2017;11:87.
Palagini L, Drake CL, Gehrman P, Meerlo P, Riemann D. Early-life origin of adult insomnia: does prenatal-early-life stress play a role? Sleep Med. 2015;16:446–56.
McEwen BS. Allostasis and the epigenetics of brain and body health over the life course: the brain on stress. JAMA Psychiatry. 2017;74:551–52.
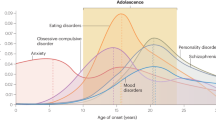
Andersen SL, Teicher MH. Stress, sensitive periods and maturational events in adolescent depression. Trends Neurosci. 2008;31:183–91.
Fries E, Hesse J, Hellhammer J, Hellhammer DH. A new view on hypocortisolism. Psychoneuroendocrinology.2005;30:1010–6.
Yehuda R, Seckl J. Minireview: stress-related psychiatric disorders with low cortisol levels: a metabolic hypothesis. Endocrinology. 2011;152:4496–503.
Kalsbeek A, Merrow M, Roenneberg T, Foster RG. Neurobiology of Circadian Timing. Preface. Progress in brain research. 2012;199:xi–xii. https://doi.org/10.1016/B978-0-444-59427-3.00031-9
Welsh DK, Takahashi JS, Kay SA. Suprachiasmatic nucleus: cell autonomy and network properties. Annu Rev Physiol. 2010;72:551–77.
Clow A, Hucklebridge F, Stalder T, Evans P, Thorn L. The cortisol awakening response: more than a measure of HPA axis function. Neurosci Biobehav Rev. 2010;35:97–103.
Fischer D, Lombardi DA, Marucci-Wellman H, Roenneberg T. Chronotypes in the US - Influence of age and sex. PLoS One. 2017;12:e0178782.
Roenneberg T, Kuehnle T, Pramstaller PP, Ricken J, Havel M, Guth A, et al. A marker for the end of adolescence. Curr Biol. 2004;14:R1038–9.
Lo Martire V, Caruso D, Palagini L, Zoccoli G, Bastianini S. Stress & sleep: a relationship lasting a lifetime. Neurosci Biobehav Rev. 2020;117:65–77.
Agorastos A, Olff M. Traumatic stress and the circadian system: neurobiology, timing and treatment of posttraumatic chronodisruption. Eur J Psychotr. 2020;11:1833644.
Agorastos A, Nicolaides NC, Bozikas VP, Chrousos GP, Pervanidou P. Multilevel interactions of stress and circadian system: implications for traumatic stress. Front Psychiatry. 2019;10:1003.
Agorastos A, Olff M. Sleep, circadian system and traumatic stress. Eur J Psychotr. 2021;12:1956746.
Buckley TM, Schatzberg AF. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J Clin Endocrinol Metab. 2005;90:3106–14.
van Dalfsen JH, Markus CR. The influence of sleep on human hypothalamic-pituitary-adrenal (HPA) axis reactivity: a systematic review. Sleep Med Rev. 2018;39:187–94.
Kuhlman KR, Chiang JJ, Bower JE, Irwin MR, Seeman TE, McCreath HE, et al. Sleep problems in adolescence are prospectively linked to later depressive symptoms via the cortisol awakening response. Dev Psychopathol. 2020;32:997–1006.
Minkel J, Moreta M, Muto J, Htaik O, Jones C, Basner M, et al. Sleep deprivation potentiates HPA axis stress reactivity in healthy adults. Health Psychol. 2014;33:1430.
Massar SA, Liu JC, Mohammad NB, Chee MW. Poor habitual sleep efficiency is associated with increased cardiovascular and cortisol stress reactivity in men. Psychoneuroendocrino. 2017;81:151–56.
Raikkonen K, Matthews KA, Pesonen AK, Pyhala R, Paavonen EJ, Feldt K, et al. Poor sleep and altered hypothalamic-pituitary-adrenocortical and sympatho-adrenal-medullary system activity in children. J Clin Endocrinol Metab. 2010;95:2254–61.
Cahill L, Gorski L, Le K. Enhanced human memory consolidation with post-learning stress: interaction with the degree of arousal at encoding. Learn Mem. 2003;10:270–4.
Kuhlmann S, Kirschbaum C, Wolf OT. Effects of oral cortisol treatment in healthy young women on memory retrieval of negative and neutral words. Neurobiol Learn Mem. 2005;83:158–62.
Bennion KA, Mickley Steinmetz KR, Kensinger EA, Payne JD. Sleep and cortisol interact to support memory consolidation. Cereb Cortex. 2015;25:646–57.
Shonkoff JP. Leveraging the biology of adversity to address the roots of disparities in health and development. Proc Natl Acad Sci USA. 2012;109:17302–7.
Wilhelm I, Azza Y, Brennwald K, Ehrt-Schafer Y, Seifritz E, Kleim B. Investigating the effect of a nap following experimental trauma on analogue PTSD symptoms. Sci Rep. 2021;11:4710.
Azza Y, Wilhelm FH, Seifritz E, Junghanns K, Kleim B, Wilhelm I. Sleep’s role in updating aversive autobiographical memories. Transl Psychiatry. 2022;12:117.
Sopp MR, Brueckner AH, Schafer SK, Lass-Hennemann J, Michael T. Differential effects of sleep on explicit and implicit memory for potential trauma reminders: findings from an analogue study. Eur J Psychotr. 2019;10:1644128.
Arora T, Grey I, Ostlundh L, Alamoodi A, Omar OM, Hubert Lam KB, et al. A systematic review and meta-analysis to assess the relationship between sleep duration/quality, mental toughness and resilience amongst healthy individuals. Sleep Med Rev. 2022;62:101593.
Hauner KK, Howard JD, Zelano C, Gottfried JA. Stimulus-specific enhancement of fear extinction during slow-wave sleep. Nat Neurosci. 2013;16:1553–5.
Diekelmann S, Born J. Cueing fear memory during sleep–to extinguish or to enhance fear? Sleep.2015;38:337–9.
Feld GB, Lange T, Gais S, Born J. Sleep-dependent declarative memory consolidation–unaffected after blocking NMDA or AMPA receptors but enhanced by NMDA coagonist D-cycloserine. Neuropsychopharmacology.2013;38:2688–97.
Hofmann SG. D-cycloserine for treating anxiety disorders: making good exposures better and bad exposures worse. Depress Anxiety 2014;31:175–7.
Mueller A, Armbruster D, Moser DA, Canli T, Lesch KP, Brocke B, et al. Interaction of serotonin transporter gene-linked polymorphic region and stressful life events predicts cortisol stress response. Neuropsychopharmacology. 2011;36:1332–9.
Lovallo WR, Enoch MA, Sorocco KH, Vincent AS, Acheson A, Cohoon AJ, et al. Joint impact of early life adversity and COMT Val158Met (rs4680) genotypes on the adult cortisol response to psychological stress. Psychosom Med. 2017;79:631–37.
Nemeroff CB. Paradise lost: the neurobiological and clinical consequences of child abuse and neglect. Neuron. 2016;89:892–909.
Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106:29–39.
Kuhlman KR, Cole SW, Irwin MR, Craske MG, Fuligni AJ, Bower JE. The role of early life adversity and inflammation in stress-induced change in reward and risk processes among adolescents. Brain Behav Immun. 2023;109:78–88.
Laricchiuta D, Panuccio A, Picerni E, Biondo D, Genovesi B, Petrosini L. The body keeps the score: the neurobiological profile of traumatized adolescents. Neurosci Biobehav Rev. 2023;145:105033.
Nusslock R, Miller GE. Early-life adversity and physical and emotional health across the lifespan: a neuroimmune network hypothesis. Biol Psychiatry. 2016;80:23–32.
Qiu Y, Fan Z, Zhong M, Yang J, Wu K, Huiqing H, et al. Brain activation elicited by acute stress: an ALE meta-analysis. Neurosci Biobehav Rev. 2022;132:706–24.
Suarez-Jimenez B, Albajes-Eizagirre A, Lazarov A, Zhu X, Harrison BJ, Radua J, et al. Neural signatures of conditioning, extinction learning, and extinction recall in posttraumatic stress disorder: a meta-analysis of functional magnetic resonance imaging studies. Psychol Med. 2020;50:1442–51.
Admon R, Milad MR, Hendler T. A causal model of post-traumatic stress disorder: disentangling predisposed from acquired neural abnormalities. Trends Cogn Sci. 2013;17:337–47.
Gerin MI, Viding E, Pingault JB, Puetz VB, Knodt AR, Radtke SR, et al. Heightened amygdala reactivity and increased stress generation predict internalizing symptoms in adults following childhood maltreatment. J Child Psychol Psychiatry. 2019;60:752–61.
Hein TC, Monk CS. Research review: neural response to threat in children, adolescents, and adults after child maltreatment - a quantitative meta-analysis. J Child Psychol Psychiatry. 2017;58:222–30.
McCrory EJ, De Brito SA, Kelly PA, Bird G, Sebastian CL, Mechelli A, et al. Amygdala activation in maltreated children during pre-attentive emotional processing. Br J Psychiatry. 2013;202:269–76.
Suzuki H, Luby JL, Botteron KN, Dietrich R, McAvoy MP, Barch DM. Early life stress and trauma and enhanced limbic activation to emotionally valenced faces in depressed and healthy children. J Am Acad Child Adolesc Psychiatry. 2014;53:800–13.e10
Chiang JJ, Taylor SE, Bower JE. Early adversity, neural development, and inflammation. Dev Psychobiol. 2015;57:887–907.
Horovitz O, Tsoory MM, Hall J, Jacobson-Pick S, Richter-Levin G. Post-weaning to pre-pubertal (‘juvenile’) stress: a model of induced predisposition to stress-related disorders. Neuroendocrinology.2012;95:56–64.
Radwan B, Jansen G, Chaudhury D. Sleep-wake dynamics pre- and post-exposure to chronic social stress. iScience. 2021;24:103204.
Radwan B, Jansen G, Chaudhury D. Abnormal sleep signals vulnerability to chronic social defeat stress. Front Neurosci. 2020;14:610655.
Sawangjit A, Oyanedel CN, Niethard N, Born J, Inostroza M. Deepened sleep makes hippocampal spatial memory more persistent. Neurobiol Learn Mem. 2020;173:107245.
Fuligni AJ, Hardway C. Daily variation in adolescents’ sleep, activities, and psychological well‐being. J Res Adolesc. 2006;16:353–78.
Bei B, Wiley JF, Trinder J, Manber R. Beyond the mean: a systematic review on the correlates of daily intraindividual variability of sleep/wake patterns. Sleep Med Rev. 2016;28:108–24.
Danese A, Widom CS. Objective and subjective experiences of child maltreatment and their relationships with psychopathology. Nat Hum Behav. 2020;4:811–18.
Author information
Authors and Affiliations
Contributions
L.S. and R.A. jointly wrote the paper.
Corresponding author
Ethics declarations
Competing interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Simon, L., Admon, R. From childhood adversity to latent stress vulnerability in adulthood: the mediating roles of sleep disturbances and HPA axis dysfunction. Neuropsychopharmacol. 48, 1425–1435 (2023). https://doi.org/10.1038/s41386-023-01638-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-023-01638-9