Abstract
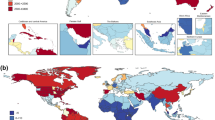
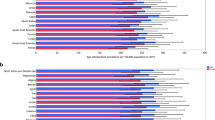
Schizophrenia substantially contributes to the burden of mental disorders. Schizophrenia’s burden and epidemiological estimates in some countries have been published, but updated estimates of prevalence, incidence, and schizophrenia-related disability at the global level are lacking. Here, we present the data from and critically discuss the Global Burden of Diseases, Injuries, and Risk Factors Study data, focusing on temporal changes in schizophrenia’s prevalence, incidence, and disability-adjusted life years (DALYs) globally. From 1990 to 2019, schizophrenia raw prevalence (14.2 to 23.6 million), incidence (941,000 to 1.3 million), and DALYs (9.1 to 15.1 million) increased by over 65%, 37%, and 65% respectively, while age-standardized estimates remained stable globally. In countries with high socio-demographic index (SDI), both prevalence and DALYs increased, while in those with low SDI, the age-standardized incidence decreased and DALYs remained stable. The male/female ratio of burden of schizophrenia has remained stable in the overall population over the past 30 years (i.e., M/F = 1.1), yet decreasing from younger to older age groups (raw prevalence in females higher than males after age 65, with males having earlier age of onset, and females longer life expectancy). Results of this work suggest that schizophrenia’s raw prevalence, incidence, and burden have been increasing since 1990. Age-adjusted estimates did not reduce. Schizophrenia detection in low SDI countries is suboptimal, and its prevention/treatment in high SDI countries should be improved, considering its increasing prevalence. Schizophrenia sex ratio inverts throughout the lifespan, suggesting different age of onset and survival by sex. However, prevalence and burden estimates for schizophrenia are probably underestimated. GBD does not account for mortality from schizophrenia (and other mental disorders, apart from anorexia nervosa).
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data are publicly available at the Institute for Health Metrics and Evaluation (IHME) website (http://www.ghdx.healthdata.org/gbd-results-tool).
References
Correll CU. Pharmacotherapy of schizophrenia | Pharmakotherapie der Schizophrenie. Nervenarzt. 2020;91:34–42.
Correll CU, Solmi M, Veronese N, Bortolato B, Rosson S, Santonastaso P, et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: A large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry. 2017;16:163–80.
Firth J, Solmi M, Wootton RE, Vancampfort D, Schuch FB, Hoare E, et al. A meta-review of “lifestyle psychiatry”: the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry. 2020;19:360–80.
Vancampfort D, Stubbs B, Mitchell AJ, De Hert M, Wampers M, Ward PB, et al. Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: A systematic review and meta-analysis. World Psychiatry. 2015;14:339–47.
Vancampfort D, Correll CU, Galling B, Probst M, De Hert M, Ward PB, et al. Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: A systematic review and large scale meta-analysis. World Psychiatry. 2016;15:166–74.
Solmi M, Firth J, Miola A, Fornaro M, Frison E, Fusar-Poli P, et al. Disparities in cancer screening in people with mental illness across the world versus the general population: prevalence and comparative meta-analysis including 4 717 839 people. Lancet Psychiatry. 2020;7:52–63.
Solmi M, Fiedorowicz J, Poddighe L, Delogu M, Miola A, Høye A, et al. Disparities in Screening and Treatment of Cardiovascular Diseases in Patients With Mental Disorders Across the World: Systematic Review and Meta-Analysis of 47 Observational Studies. Am J Psychiatry. 2021;178:793–803.
Correll CU, Solmi M, Croatto G, Schneider LK, Rohani-Montez SC, Fairley L, et al. Mortality in people with schizophrenia: a systematic review and meta-analysis of relative risk and aggravating or attenuating factors. World Psychiatry. 2022;21:248–71.
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
GBD Collaborators Mental Disorders. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137–50.
He H, Liu Q, Li N, Guo L, Gao F, Bai L, et al. Trends in the incidence and DALYs of schizophrenia at the global, regional and national levels: results from the Global Burden of Disease Study 2017. Epidemiol Psychiatr Sci. 2020;29:e91–e91.
Charlson FJ, Ferrari AJ, Santomauro DF, Diminic S, Stockings E, Scott JG, et al. Global Epidemiology and Burden of Schizophrenia: Findings From the Global Burden of Disease Study 2016. Schizophr Bull. 2018;44:1195–203.
Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 2013;382:1575–86.
Grisales-Romero H, González D, Porras S. Años de vida saludable perdidos a causa de trastornos mentales y enfermedades del sistema nervioso de la población de Medellín, 2006-2012. Rev Colomb Psiquiatr. 2020;49:29–38.
Baxter AJ, Charlson FJ, Cheng HG, Shidhaye R, Ferrari AJ, Whiteford HA. Prevalence of mental, neurological, and substance use disorders in China and India: a systematic analysis. Lancet Psychiatry. 2016;3:832–41.
Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T. The global burden of mental, neurological and substance use disorders: an analysis from the Global Burden of Disease Study 2010. PLoS One. 2015;10:e0116820–e0116820.
McGrath J, Saha S, Chant D, Welham J. Schizophrenia: A Concise Overview of Incidence, Prevalence, and Mortality. Epidemiol Rev. 2008;30:67–76.
Jaeschke K, Hanna F, Ali S, Chowdhary N, Dua T, Charlson F. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017. Glob Ment Heal. 2021;8:e27.
Ayano G, Demelash S, yohannes Z, Haile K, Tulu M, Assefa D, et al. Misdiagnosis, detection rate, and associated factors of severe psychiatric disorders in specialized psychiatry centers in Ethiopia. Ann Gen Psychiatry. 2021;20:10.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th edn. Washington, D.C.: American Psychiatric Publishing, 2013.
Association AP. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. 4th edn. 2000.
Tandon R, Gaebel W, Barch DM, Bustillo J, Gur RE, Heckers S, et al. Definition and description of schizophrenia in the DSM-5. Schizophr Res. 2013;150:3–10.
Tandon R. The Nosology of Schizophrenia: Toward DSM-5 and ICD-11. Psychiatr Clin. 2012;35:557–69.
Substance Abuse and Mental Health Services Administration. Impact of the DSM-IV to DSM-5 Changes on the National Survey on Drug Use and Health [Internet]. 22. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2016.
Tandon R, Bruijnzeel D, Rankupalli B. Does change in definition of psychotic symptoms in diagnosis of schizophrenia in DSM-5 affect caseness? Asian J Psychiatr. 2013;6:330–2.
Fusar-Poli P, Correll C, Arango C, Berk M, Patel V, Ioannidis J. Preventive psychiatry: a blueprint for improving the mental health of young people. World Psychiatry. 2021;20:200–21.
Radua J, Ramella-Cravaro V, Ioannidis JPA, Reichenberg A, Phiphopthatsanee N, Amir T, et al. What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry. 2018;17:49–66.
Belbasis L, Köhler CA, Stefanis N, Stubbs B, van Os J, Vieta E, et al. Risk factors and peripheral biomarkers for schizophrenia spectrum disorders: an umbrella review of meta-analyses. Acta Psychiatr Scand. 2018;137:88–97.
Arango C, Dragioti E, Solmi M, Cortese S, Domschke K, Murray RM, et al. Risk and protective factors for mental disorders beyond genetics: an evidence-based atlas. World Psychiatry. 2021;20:417–36.
Davies C, Segre G, Estradé A, Radua J, De Micheli A, Provenzani U, et al. Prenatal and perinatal risk and protective factors for psychosis: a systematic review and meta-analysis. Lancet Psychiatry. 2020;7:399–410.
Oliver D, Reilly TJ, Baccaredda Boy O, Petros N, Davies C, Borgwardt S, et al. What Causes the Onset of Psychosis in Individuals at Clinical High Risk? A Meta-analysis of Risk and Protective Factors. Schizophr Bull. 2020;46:110–20.
Fusar-Poli P, Radua J. Ten simple rules for conducting umbrella reviews. Evid Based Ment Health. 2018;21:95–100.
Ioannidis JPA. Integration of evidence from multiple meta-analyses: A primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. CMAJ 2009;181:488–93.
Solmi M, Dragioti E, Croatto G, Radua J, Borgwardt S, Carvalho AF, et al. Risk and protective factors for cannabis, cocaine, and opioid use disorders: An umbrella review of meta-analyses of observational studies. Neurosci Biobehav Rev. 2021;126:243–51.
Fusar-Poli P, Solmi M, Brondino N, Davies C, Chae C, Politi P, et al. Transdiagnostic psychiatry: a systematic review. World Psychiatry. 2019;18:192–207.
Dragioti E, Radua J, Solmi M, Arango C, Oliver D, Cortese S, et al. Global population attributable fraction of potentially modifiable risk factors for mental disorders: a meta-umbrella systematic review. Mol Psychiatry. 2022;27:3510–9.
Taipale H, Solmi M, Lähteenvuo M, Tanskanen A, Correll CU, Tiihonen J. Antipsychotic use and risk of breast cancer in women with schizophrenia: a nationwide nested case-control study in Finland. Lancet Psychiatry. 2021;8:883–91.
Solmi M, Tiihonen J, Lähteenvuo M, Tanskanen A, Correll C, Taipale H. Antipsychotics Use Is Associated With Greater Adherence to Cardiometabolic Medications in Patients With Schizophrenia: Results From a Nationwide, Within-subject Design Study. Schizophir Bull. 2021. 21 July 2021. https://doi.org/10.1093/SCHBUL/SBAB087.
Charlson, F. J., Baxter, A. J., Dua, T., Degenhardt, L., Whiteford, H. A., & Vos, T. Excess mortality from mental, neurological and substance use disorders in the Global Burden of Disease Study 2010. Epidemiology and psychiatric sciences, 2015;24:121–140.
Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. 2021;27:281–95.
Hunt GE, Large MM, Cleary M, Lai HMX, Saunders JB. Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990–2017: Systematic review and meta-analysis. Drug Alcohol Depend. 2018;191:234–58.
Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M. “Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis”: Correction. Lancet Psychiatry. 2017;4:e19–e19.
Crump C, Winkleby MA, Sundquist K, Sundquist J. Comorbidities and mortality in persons with schizophrenia: a Swedish national cohort study. Am J Psychiatry. 2013;170:324–33.
Lawrence D, Hancock KJ, Kisely S. The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: Retrospective analysis of population based registers. BMJ. 2013;346:f2539.
Kahn RS, Sommer IE, Murray RM, Meyer-Lindenberg A, Weinberger DR, Cannon TD, et al. Schizophrenia. Nat Rev Dis Prim. 2015;1:1–23.
De Hert M, Schreurs V, Vancampfort D, VAN Winkel R. Metabolic syndrome in people with schizophrenia: a review. World Psychiatry. 2009;8:15–22.
Vancampfort D, Firth J, Schuch FB, Rosenbaum S, Mugisha J, Hallgren M, et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta-analysis. World Psychiatry. 2017;16:308–15.
Author information
Authors and Affiliations
Contributions
All authors contributed and approved the study’s protocol. MS created the first draft of the manuscript. MS, DY, and SL analysed data. MS, JS, MF, and SC provided overall guidance. Finally, all authors read, edited, and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
MS received honoraria/has been consultant for AbbVie, Angelini, Lundbeck, Otsuka. CUC has been a consultant and/or advisor to or has received honoraria from: AbbVie, Acadia, Alkermes, Allergan, Angelini, Aristo, Boehringer-Ingelheim, Cardio Diagnostics, Cerevel, CNX Therapeutics, Compass Pathways, Darnitsa, Gedeon Richter, Hikma, Holmusk, IntraCellular Therapies, Janssen/J&J, Karuna, LB Pharma, Lundbeck, MedAvante-ProPhase, MedInCell, Merck, Mindpax, Mitsubishi Tanabe Pharma, Mylan, Neurocrine, Newron, Noven, Novo Nordisk,Otsuka, Pharmabrain, PPD Biotech, Recordati, Relmada, Reviva, Rovi, Seqirus, SK Life Science, Sunovion, Sun Pharma, Supernus, Takeda, Teva, and Viatris. He provided expert testimony for Janssen and Otsuka. He served on a Data Safety Monitoring Board for Compass, Lundbeck, Relmada, Reviva, Rovi, Supernus, and Teva. He has received grant support from Janssen and Takeda. He received royalties from UpToDate and is also a stock option holder of Cardio Diagnostics, Mindpax, LB Pharma and Quantic. MF received consulting fees & fees for non-CME/CE services from: Angelini, AstraZeneca, Boehringer Ingelheim, Bristol Meyers Squibb, Eli Lilly, GlaxoSmithKline, Innova Pharma, Lundbeck, Pfizer, Sanofi, Servier. All outside of the present work. SCo has received honoraria from the following non-profit associations: British Association for Psychopharmacology (BAP), Association for Child and Adolescent mental health (ACAMH), and Canadian ADHD Alliance Resource (CADDRA). SG received honoraria/has been consultant for Boehringer Ingelheim. Other authors have no conflict of interest o declare.
Ethical approval
We followed the standard procedure recommended registering additional publications from the GBD 2019 project after the publication of the capstone paper [9]. The Institutional Review Board approved our study at Yonsei University Health System for data use.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Solmi, M., Seitidis, G., Mavridis, D. et al. Incidence, prevalence, and global burden of schizophrenia - data, with critical appraisal, from the Global Burden of Disease (GBD) 2019. Mol Psychiatry 28, 5319–5327 (2023). https://doi.org/10.1038/s41380-023-02138-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-023-02138-4