Abstract
Importance
It is unclear if systemic steroids decrease the risk of Bronchopulmonary Dysplasia (BPD) while increasing the risk of neurodevelopmental impairment (NDI).
Objective
Conduct a systematic review of randomized controlled trials of systemic steroids to evaluate the risk of BPD, mortality, and NDI in premature infants ≤30 weeks.
Data sources
MEDLINE, EBSCOhost, Web of Science, Cochrane Library, Embase, and CINAHL.
Study selection
Randomized clinical trials of Dexamethasone (DEX) or Hydrocortisone (HC) to prevent BPD in premature infants ≤ 30 weeks.
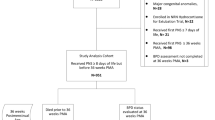
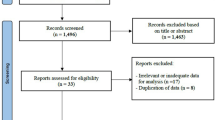
Data extraction and synthesis
Data were extracted using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. Random-effects meta-analyses and multivariable meta-regression were conducted.
Main outcomes and measures
Primary outcomes were BPD, mortality, and NDI. Secondary outcomes were hypertension, hyperglycemia, sepsis, intestinal perforation, necrotizing enterocolitis (NEC), and retinopathy of prematurity (ROP). The a priori hypothesis was that steroids would reduce the risk of BPD without increasing NDI.
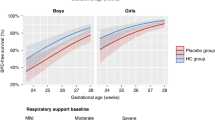
Results
There were 6377 preterm infants in the 44 (32 DEX, 13 HC) selected studies. DEX significantly reduced the risk of BPD, RR = 0.66, (95% CI, 0.56–0.78). The most effective DEX regimen was medium cumulative dose (2 to 3 mg/kg), RR = 0.43 (95% CI, 0.29–0.65); day of initiation <8 days: RR = 0.68, (95% CI, 0.59–0.79); and treatment for ≥14 days: RR = 0.67 (95% CI, 0.55–0.80). HC did not significantly decrease the risk of BPD, RR = 0.98, (95% CI, 0.87–1.10). Neither DEX, (RR = 0.92, 95% CI, 0.78–1.09) nor HC (RR = 0.83, 95% CI, 0.68–1.01) decrease the risk of mortality. The risk of CP was not increased by either DEX (RR = 1.09, 95% CI, 0.55–2.17) or HC (RR = 1.18, 95% CI, 0.75–1.87). There were no significant differences between steroids and placebo for MDI/PDI scores. Multivariable meta-regression models showed that DEX significantly reduced the risk of BPD without increased risk of CP. DEX increased the risk of hypertension and hyperglycemia. Studies showed high heterogeneity, differing treatment regimen, missing data and different rates of follow-up.
Conclusion and relevance
DEX, but not HC, significantly decreased the risk of BPD. Neither steroid showed an increased risk of NDI or mortality.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015;314:1039–51. https://doi.org/10.1001/jama.2015.10244.
Bell EF, Hintz SR, Hansen NI, Bann CM, Wyckoff MH, DeMauro SB, et al. Mortality, in-hospital morbidity, care practices, and 2-year outcomes for extremely preterm infants in the US, 2013-2018. JAMA. 2022;327:248–63. https://doi.org/10.1001/jama.2021.23580.
Jensen EA, Edwards EM, Greenberg LT, Soll RF, Ehret DEY, Horbar JD. Severity of bronchopulmonary dysplasia among very preterm infants in the United States. Pediatrics. 2021;148. https://doi.org/10.1542/peds.2020-030007.
Hwang JS, Rehan VK. Recent advances in bronchopulmonary dysplasia: pathophysiology, prevention, and treatment. Lung. 2018;196:129–38. https://doi.org/10.1007/s00408-018-0084-z.
Levy PT, Dioneda B, Holland MR, Sekarski TJ, Lee CK, Mathur A, et al. Right ventricular function in preterm and term neonates: reference values for right ventricle areas and fractional area of change. J Am Soc Echocardiogr. 2015;28:559–69. https://doi.org/10.1016/j.echo.2015.01.024.
Bui CB, Pang MA, Sehgal A, Theda C, Lao JC, Berger PJ, et al. Pulmonary hypertension associated with bronchopulmonary dysplasia in preterm infants. J Reprod Immunol. 2017;124:21–29. https://doi.org/10.1016/j.jri.2017.09.013.
Donda K, Agyemang CO, Adjetey NA, Agyekum A, Princewill N, Ayensu M, et al. Tracheostomy trends in preterm infants with bronchopulmonary dysplasia in the United States: 2008-2017. Pediatr Pulmonol. 2021;56:1008–17. https://doi.org/10.1002/ppul.25273.
Collaco JM, McGrath-Morrow SA. Respiratory phenotypes for preterm infants, children, and adults: bronchopulmonary dysplasia and more. Ann Am Thorac Soc. 2018;15:530–8. https://doi.org/10.1513/AnnalsATS.201709-756FR.
Manimtim WM, Agarwal A, Alexiou S, Levin JC, Aoyama B, Austin ED, et al. Respiratory outcomes for ventilator-dependent children with bronchopulmonary dysplasia. Pediatrics. 2023;151. https://doi.org/10.1542/peds.2022-060651.
Cheong JLY, Doyle LW. An update on pulmonary and neurodevelopmental outcomes of bronchopulmonary dysplasia. Semin Perinatol. 2018;42:478–84. https://doi.org/10.1053/j.semperi.2018.09.013.
Schmidt B, Asztalos EV, Roberts RS, Robertson CM, Sauve RS, Whitefield MF. Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months: results from the trial of indomethacin prophylaxis in preterms. JAMA. 2003;289:1124–9. https://doi.org/10.1001/jama.289.9.1124.
Sriram S, Schreiber MD, Msall ME, Kuban KCK, Joseph RM, O’Shea TM, et al. Cognitive development and quality of life associated with BPD in 10-year-olds born preterm. Pediatrics. 2018;141:e20172719. https://doi.org/10.1542/peds.2017-2719.
Doyle LW, Ranganathan S, Mainzer RM, Cheong JLY. Victorian infant collaborative study G. Relationships of severity of bronchopulmonary dysplasia with adverse neurodevelopmental outcomes and poor respiratory function at 7-8 years of age. J Pediatr. 2024;269:114005. https://doi.org/10.1016/j.jpeds.2024.114005.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants. an evidence-based approach. Am J Respir Crit Care Med. 2019;200:751–9. https://doi.org/10.1164/rccm.201812-2348OC.
Mammel MC, Green TP, Johnson DE, Thompson TR. Controlled trial of dexamethasone therapy in infants with bronchopulmonary dysplasia. Lancet. 1983;1:1356–8. https://doi.org/10.1016/s0140-6736(83)92139-6.
American Academy of Pediatrics. Committee on fetus and newborn. Postnatal corticosteroids to treat or prevent chronic lung disease in preterm infants. Pediatrics. 2002;109:330–8. https://doi.org/10.1542/peds.109.2.330.
Walsh MC, Yao Q, Horbar JD, Carpenter JH, Lee SK, Ohlsson A. Changes in the use of postnatal steroids for bronchopulmonary dysplasia in 3 large neonatal networks. Pediatrics. 2006;118:e1328–35. https://doi.org/10.1542/peds.2006-0359.
Yoder BA, Harrison M, Clark RH. Time-related changes in steroid use and bronchopulmonary dysplasia in preterm infants. Pediatrics. 2009;124:673–9. https://doi.org/10.1542/peds.2008-2793.
Abiramalatha T, Ramaswamy VV, Bandyopadhyay T, Somanath SH, Shaik NB, Pullattayil AK, et al. Interventions to prevent bronchopulmonary dysplasia in preterm neonates: an umbrella review of systematic reviews and meta-analyses. JAMA Pediatr. 2022;176:502–16. https://doi.org/10.1001/jamapediatrics.2021.6619.
Ramaswamy VV, Bandyopadhyay T, Nanda D, Bandiya P, Ahmed J, Garg A, et al. Assessment of postnatal corticosteroids for the prevention of bronchopulmonary dysplasia in preterm neonates: a systematic review and network meta-analysis. JAMA Pediatr. 2021;175:e206826. https://doi.org/10.1001/jamapediatrics.2020.6826.
Doyle LW, Davis PG, Morley CJ, McPhee A, Carlin JB. Low-dose dexamethasone facilitates extubation among chronically ventilator-dependent infants: a multicenter, international, randomized, controlled trial. Pediatrics. 2006;117:75–83. https://doi.org/10.1542/peds.2004-2843.
Job S, Clarke P. Current UK practices in steroid treatment of chronic lung disease. Arch Dis Child Fetal Neonatal Ed. 2015;100:F371. https://doi.org/10.1136/archdischild-2014-308060.
Cummings JJ, Pramanik AK. Postnatal corticosteroids to prevent or treat chronic lung disease following preterm birth. Pediatrics. 2022;149:e2022057530. https://doi.org/10.1542/peds.2022-057530.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. https://doi.org/10.1136/bmj.n160.
Onland W, Cools F, Kroon A, Ramful D, El Moussawi F, Nicaise C, et al. Effect of hydrocortisone therapy initiated 7 to 14 days after birth on mortality or bronchopulmonary dysplasia among very preterm infants receiving mechanical ventilation: a randomized clinical trial. JAMA. 2019;321:354–363. https://doi.org/10.1001/jama.2018.21443.
Doyle LW, Cheong JL, Ehrenkranz RA, Halliday HL. Late (>7 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst Rev. 2017;10:CD001145. https://doi.org/10.1002/14651858.CD001145.pub4.
Baud O, Biran V, Trousson C, Leroy E, Mohamed D, Alberti C. Two-year outcomes after prophylactic hydrocortisone in extremely preterm neonates. EAPS Congress 2016. Eur J Pediatr. 2016;175:1393–880. https://doi.org/10.1007/s00431-016-2785-8.
Clauss C, Thomas S, Khodak I, Tack V, Akerman M, Hanna N, et al. Hydrocortisone and bronchopulmonary dysplasia: variables associated with response in premature infants. J Perinatol. 2020;40:1349–57. https://doi.org/10.1038/s41372-020-0680-7.
Htun ZT, Schulz EV, Desai RK, Marasch JL, McPherson CC, Mastrandrea LD. et al. Postnatal steroid management in preterm infants with evolving bronchopulmonary dysplasia. J Perinatol. 2021;41:1783–96. https://doi.org/10.1038/s41372-021-01083-w.
Sterne J, Savović J, Page M, Elbers R, Blencowe N, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:14898. https://doi.org/10.1136/bmj.14898.
GRADEpro Guideline Development Tool [Software]. McMaster University and Evidence Prime, 2022. Available from gradepro.org. 2022.
Viechtbauer W. Conducting meta-analyses in R with metafor package. J Stat Softw. 2010;36:1–48.
Harrer M, Cuijpers P, Furukawa TA, Ebert DD. Doing meta-analysis with R: a hands-on guide. 1st ed. Chapman & Hall/CRC Press; 2021.
Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111. https://doi.org/10.1002/jrsm.12.
Christiansen S, Iverson C, Flanagin A, Livingston EH, Fishcer L, Manno C, et al. AMA manual of style: A guide for authors and editors. American Medical Association manual of style. 11th edition. New York, NY: Oxford University Press; 2020.
Doyle LW, Cheong JL, Hay S, Manley BJ, Halliday HL. Early (< 7 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst Rev. 2021;10:Cd001146. https://doi.org/10.1002/14651858.CD001146.pub6.
Doyle LW, Cheong JL, Hay S, Manley BJ, Halliday HL. Late (≥ 7 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst Rev. 2021;11:Cd001145. https://doi.org/10.1002/14651858.CD001145.pub5.
Zeng LN, Tian JH, Song FJ, Li WR, Jiang LC, Gui G, et al. Corticosteroids for the prevention of bronchopulmonary dysplasia in preterm infants: a network meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2018;103:F506–11. https://doi.org/10.1136/archdischild-2017-313759.
Hay S, Ovelman C, Zupancic JA, Doyle LW, Onland W, Konstantinidis M, et al. Systemic corticosteroids for the prevention of bronchopulmonary dysplasia, a network meta-analysis. Cochrane Database Syst Rev. 2023;8:CD013730. https://doi.org/10.1002/14651858.CD013730.pub2.
van de Loo M, van Kaam A, Offringa M, Doyle LW, Cooper C, Onland W. Corticosteroids for the prevention and treatment of bronchopulmonary dysplasia: an overview of systemic reviews. Cochrane Database Syst Rev. 2024:CD013271. https://doi.org/10.1002/14651858.CD013271.pub2.
Onland W, Offringa M, Jaegere APD, Van Kaam AH. Finding the optimal postnatal dexamethasone regimen for preterm infants at risk of bronchopulmonary dysplasia: a systematic review of placebo-controlled trials. Pediatrics. 2009;123:367–77. https://doi.org/10.1542/peds.2008-0016.
Doyle LW, Halliday HL, Ehrenkranz RA, Davis PG, Sinclair JC. An update on the impact of postnatal systemic corticosteroids on mortality and cerebral palsy in preterm infants: effect modification by risk of bronchopulmonary dysplasia. J Pediatr. 2014;165:1258–60. https://doi.org/10.1016/j.jpeds.2014.07.049.
Greenberg RG, McDonald SA, Laughon MM, Tanaka D, Jensen E, Van Meurs K, et al. Online clinical tool to estimate risk of bronchopulmonary dysplasia in extremely preterm infants. Arch Dis Child Fetal Neonatal Ed. 2022. https://doi.org/10.1136/archdischild-2021-323573.
Shimotsuma T, Tomotaki S, Akita M, Araki R, Tomotaki H, Iwanaga K, et al. Severe Bronchopulmonary Dysplasia adversely affects brain growth in preterm infants. Neonatology. 2024. https://doi.org/10.1159/000538527.
Acknowledgements
The authors thank the contributions of Hayrettin Okut, PhD, who advised us on statistical aspects of model development, including programming in R.
Author information
Authors and Affiliations
Contributions
TSR: conceptualized, formulated the research methodology, wrote the original draft, reviewed and edited the manuscript, supervised/administered the whole project and guarantor for the project. REZ: conceptualized, formulated the research methodology, performed formal analysis, curated data and wrote the original draft, reviewed and edited the manuscript. RL: conceptualized, formulated the research methodology, wrote the original draft, reviewed and edited the manuscript. SAB: conceptualized, formulated the research methodology, wrote the original draft, reviewed and edited the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
TSR, REZ, RL, and SAB have no relevant conflicts to disclose. This study was not supported by funding from any source.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Raghuveer, T.S., Zackula, R.E., Lakhotia, R. et al. Systemic steroids and bronchopulmonary dysplasia: a systematic review and meta-analysis. J Perinatol (2024). https://doi.org/10.1038/s41372-024-02097-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-024-02097-w