Abstract
Objective
To determine the anesthetic approach with the least adverse events and better cardiorespiratory stability profile, used in infants undergoing laser photocoagulation for retinopathy of prematurity.
Study design
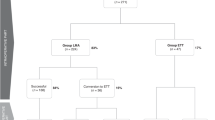
A systematic review was conducted. PubMed, Scopus, and Cochrane Library were searched until 27th October 2021. Reference lists of relevant studies, and abstract books of international annual meetings of pediatric Οphthalmology for the years 2020 and 2021 were also looked at, as well as Clinical trials registry (https://clinicaltrials.gov/).
Result
Overall 18 primary studies (3 randomized controlled trials, 3 cohorts, 12 case series) were included, investigating different anesthetic modalities. Cardiopulmonary instability was more common, and hypothermia was less common in the sedation groups of pentazocine/midazolam and fentanyl/midazolam, compared to the general anesthesia group of air/oxygen/sevoflurane (AOS). Cardiorespiratory instability was also more common in sedation with propofol/ketamine compared to general anesthesia with AOS, while postoperative mechanical ventilation was more frequently needed in the latter. Αpnea, need for supplemental oxygen and cardiorespiratory instability was more frequent in infants receiving fentanyl as opposed to ketamine. Fentanyl compared to morphine presented no differences in safety parameters. Finally, topical anesthesia showed the greatest instability with a higher mean postoperative cardiorespiratory index, compared to both sedation and general anesthesia. Episodes of life-threatening events were reported after topical anesthesia, while hypothermia and oliguria presented less often after topical, compared to general anesthesia and sedation.
Conclusion
Significant heterogeneity among studies precludes direct comparisons and generalizability of the results. No specific anesthetic modality for treatment of ROP with laser photocoagulation was shown to be superior in terms of safety. Well-designed studies are required to establish the optimal anesthetic approach, considering that laser photocoagulation still remains one of the main therapeutic modalities for ROP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article and its supplementary material files. Further enquiries can be directed to the corresponding author. This article is part of a thesis for the requirements of the postgraduate program “Medical Research Methodology in Medicine and Health Sciences” of the Aristotle University of Thessaloniki [34], available in: (http://ikee.lib.auth.gr/record/338708/files/GRI-2022-34613.pdf).
References
Mintz-Hittner HA, Kennedy KA, Chuang AZ, Group, RC B-. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011;364:603–15.
Terry TL. Extreme prematurity and fibroblastic overgrowth of persistent vascular sheath behind each crystalline lens: I. Preliminary report. Am J Ophthalmol. 2018;192:xxviii.
Dannelley JF, Johnson PN, Anderson MP, Oestreich K, Siatkowski RM, Miller JL. Assessment of outcomes with a sedation protocol during laser photocoagulation in preterm infants with retinopathy of prematurity. J Pediatr Pharmacol Ther. 2018;23:410–6.
Parulekar MV, Chen SD, Patel CK. Sub-Tenon’s local anaesthesia for the treatment of retinopathy of prematurity with diode laser. Eye. 2008;22:375–9.
Scottish Intercollegiate Guidelines Network. SIGN Guideline 58: safe sedation of children undergoing diagnostic and therapeutic procedures. Paediatr Anaesth. 2008;18:11–2.
Hartrey R. Anaesthesia for the laser treatment of neonates with retinopathy of prematurity. Eye 2007;21:1025–7.
Ulgey A, Gunes I, Bayram A, Aksu R, Bicer C, Ugur F, et al. Decreasing the need for mechanical ventilation after surgery for retinopathy of prematurity: sedoanalgesia vs. general anesthesia. Turk J Med Sci. 2015;45:1292–9.
Reighard C, Junaid S, Jackson WM, Arif A, Waddington H, Whitehouse AJO, et al. Anesthetic exposure during childhood and neurodevelopmental outcomes: a systematic review and meta-analysis. JAMA Netw Open. 2022;5:e2217427.
Nasr VG, Davis JM. Anesthetic use in newborn infants: the urgent need for rigorous evaluation. Pediatr Res. 2015;78:2–6.
Chen SD, Sundaram V, Wilkinson A, Patel CK. Variation in anaesthesia for the laser treatment of retinopathy of prematurity-a survey of ophthalmologists in the UK. Eye. 2007;21:1033–6.
Sato Y, Oshiro M, Takemoto K, Hosono H, Saito A, Kondo T, et al. Multicenter observational study comparing sedation/analgesia protocols for laser photocoagulation treatment of retinopathy of prematurity. J Perinatol. 2015;35:965–9.
Jiang JB, Strauss R, Luo XQ, Nie C, Wang YL, Zhang JW, et al. Anaesthesia modalities during laser photocoagulation for retinopathy of prematurity: a retrospective, longitudinal study. BMJ Open. 2017;7:e013344.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
ClinicalTrials.gov 2021 Available from: https://clinicaltrials.gov/.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898.
GA Wells, B Shea, D O’Connell, J Peterson, V Welch, M Losos, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses 2013 Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. 2018;23:60–3.
But A, Arikan M, Aslan B, Öztürk L, Tabuk M, Horasanli E. Comparison of anesthesia with sevofl urane-N2O and midazolam-remifentanil in low-birth-weight premature infants undergoing diode laser photocoagulation. Turk J Med Sci. 2012;42:573–9.
Madathil S, Thomas D, Chandra P, Agarwal R, Sankar MJ, Thukral A, et al. ‘NOPAIN-ROP’ trial: Intravenous fentanyl and intravenous ketamine for pain relief during laser photocoagulation for retinopathy of prematurity (ROP) in preterm infants: A randomised trial. BMJ Open. 2021;11:e046235.
Orge FH, Lee TJ, Walsh M, Gordon K. Comparison of fentanyl and morphine in laser surgery for retinopathy of prematurity. J AAPOS. 2013;17:135–9.
Demirel N, Bas AY, Kavurt S, Celik IH, Yucel H, Turkbay D, et al. Remifentanil analgesia during laser treatment for retinopathy of prematurity: a practical approach in neonatal intensive care unit. Am J Perinatol. 2014;31:983–6.
Gorbe E, Vamos R, Joo GJ, Jeager J, Molvarec A, Berecz B, et al. Perioperative analgesia of infants during the therapy for retinopathy of prematurity. Med Sci Monit. 2010;16:CR186–9.
Kaur B, Carden SM, Wong J, Frawley G. Anesthesia management of laser photocoagulation for retinopathy of prematurity. A retrospective review of perioperative adverse events. Paediatr Anaesth. 2020;30:1261–8.
Kirwan C, O’Keefe M, Prendergast M, Twomey A, Murphy J. Morphine analgesia as an alternative to general anaesthesia during laser treatment of retinopathy of prematurity. Acta Ophthalmol Scand. 2007;85:644–7.
Lyon F, Dabbs T, O’Meara M. Ketamine sedation during the treatment of retinopathy of prematurity. Eye. 2008;22:684–6.
Ferrer Novella C, Gonzalez Viejo I, Oro Fraile J, Mayoral Lopez F, Dieste Marcial M. New anaesthetic technique in diode laser treatment of retinopathy of prematurity. Pediatrics. 2008;68:576–80.
Piersigilli F, Di Pede A, Catena G, Lozzi S, Auriti C, Bersani I, et al. Propofol and fentanyl sedation for laser treatment of retinopathy of prematurity to avoid intubation. J Matern Fetal Neonatal Med. 2019;32:517–21.
Pinho DFR, Real C, Ferreira L, Pina P. Peribulbar block combined with general anesthesia in babies undergoing laser treatment for retinopathy of prematurity: a retrospective analysis. Braz J Anesthesiol. 2018;68:431–6.
Sammartino M, Bocci MG, Ferro G, Mercurio G, Papacci P, Conti G, et al. Efficacy and safety of continuous intravenous infusion of remifentanil in preterm infants undergoing laser therapy in retinopathy of prematurity: clinical experience. Paediatr Anaesth. 2003;13:596–602.
Saylan S, Akdogan A, Kader S, Tugcugil E, Besir A, Kola M, et al. Sedoanalgesia modality during laser photocoagulation for retinopathy of prematurity: Intraoperative complications and early postoperative follow-up. Ulus Travma Acids Cerrahi Derg. 2020;26:754–9.
Salaün JP, de Queiroz M, Orliaguet G. Development: Epidemiology and management of postoperative apnoea in premature and term newborns. Anaesth Crit Care Pain Med. 2020;39:871–5.
Walz JM, Bemme S, Reichl S, Akman S, Breuß H, Süsskind D, et al. Treated cases of retinopathy of prematurity in Germany: 5-year data from the Retina.net ROP registry. Ophthalmologe 2018;115:476–88.
Ahmed SB, Higham A, Mulvihill A, Chan TKJ, Adams G, Patel CK. The UK practice of Anti-VEGF therapy for treatment of retinopathy of prematurity. Eye. 2021;35:2451–3.
Gavriilidou A Safety comparison between different anesthesia protocols regarding premature infants undergoing laser therapy for Retinopathy of Prematurity- Systematic Review. Institutional Repository of Scientific Publications: Aristotle University of Thessaloniki; 2022.
Acknowledgements
We would like to thank Professor D.G.Goulis and I. Doundoulakis who very kindly contributed to this systematic review.
Author information
Authors and Affiliations
Contributions
Contributions to the conception and design of the work were made by all authors (AG, AKS, ZA, NZ, ABH, AM). Acquisition and analysis of data were conducted by AG, AKS, and AM. Interpretation of data was done by all authors (AG, AKS, ZA, NZ, ABH, AM). Drafting the work was performed by AG, AKS, and AM, and revising it critically was performed by all authors (AG, AKS, ZA, NZ, ABH, AM). Final approval of the version to be published was given by all authors (AG, AKS, ZA, NZ, ABH, AM). All authors (AG, AKS, ZA, NZ, ABH, AM) agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
competing interests
The authors declare no competing interests.
Ethics
An ethics statement is not applicable because this study is based exclusively on published literature.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gavriilidou, A., Seliniotaki, A.K., Arvanitaki, Z. et al. Safety profile of anesthetic modalities during laser treatment for retinopathy of prematurity: a systematic review. J Perinatol 43, 685–693 (2023). https://doi.org/10.1038/s41372-023-01622-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01622-7
This article is cited by
-
Airway management may influence postoperative ventilation need in preterm infants after laser eye treatment
Pediatric Research (2024)
-
Safety profile of anesthetic modalities during laser treatment for retinopathy of prematurity: a systematic review
Journal of Perinatology (2023)