Abstract
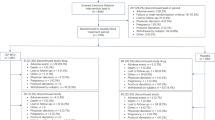
Ambulatory blood pressure monitoring (ABPM) is considered the most reliable and accurate measurement of blood pressure (BP). However, the use of ABPM has some limitations, which make it difficult to complete for the entire 24 h. We aimed to establish in which part of the day BP measurements are in highest correlation with full ABPM (over 24 h) results. We performed a retrospective cross-sectional study which included 3113 full ABPM. Each ABPM was divided into 6- and 8-hour segments, and mean BP in each time segment was calculated. Linear mix models for describing BP by BP in each time segment were performed. A total of 3113 ABPM measurements carried out on 2676 patients (mean age 57.78 ± 14.74) were included in the study. Linear mix models demonstrated significant association between mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) in full ABPM, and SBP and DBP between 2–10 PM, respectively (SBP: β = 0.902, p < 0.001; DBP: β = 0.839, p < 0.001), adjusted for gender, age, season, and relevant interactions. This section had higher coefficient correlations than other sections which were examined. The study findings indicate high correlation between BP between 2–10 PM, and BP in full-ABPM, by each season. This time segment may be ideal for short-term BP monitoring as an initial screening test and for patients who are unable to complete full ABPM. However, since this time segment does not include nighttime hours, there is a risk of underdiagnosis of non-dipper.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data generated or analyzed during this study can be available from the corresponding author on reasonable request.
References
Whelton PK, Carey RM, Aronow WS, Ovbiagele B, Casey DE, Smith SC, et al. 2017 Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines; 2017. https://doi.org/10.1161/HYP.0000000000000065/-/DC1
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–219.
Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. N. Engl J Med. 2006;354:2368–74.
Wolak T, Wilk L, Paran E, Wolak A, Gutmacher B, Shleyfer E, et al. Is it possible to shorten ambulatory blood pressure monitoring? J Clin Hypertens. 2013;15:570–4.
Ernst ME, Weber CA, Dawson JD, Connor MAO, Lin W, Carter BL, et al. How well does a shortened time interval characterize results of a full ambulatory blood pressure monitoring session? J Clin Hypertens. 2008;10:431–5.
Ernst ME, Sezate GS, Lin W, Weber CA, Dawson JD, Carter BL, et al. Indication-specific 6-h systolic blood pressure thresholds can approximate 24-h determination of blood pressure control. J Hum Hypertens. 2011;25:250–5.
Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, et al. Measurement of blood pressure in humans: a scientific statement from the american heart association. 2019. https://doi.org/10.1161/HYP.0000000000000087
Modesti PA. Season, temperature and blood pressure: a complex interaction. Eur J Intern Med. 2013;24:604–7.
Stergiou GS, Myrsilidi A, Kollias A, Destounis A, Roussias L, Kalogeropoulos P. Seasonal variation in meteorological parameters and office, ambulatory and home blood pressure: predicting factors and clinical implications. Hypertens Res. 2015;38:869–75.
Kristal-Boneh E, Harari G, Green MS, Ribak J. Body mass index is associated with differential seasonal change in ambulatory blood pressure levels. Am J Hypertens. 1996;9:1179–85.
Charach G, Rabinovich PD, Weintraub M. Seasonal changes in blood pressure and frequency of related complications in elderly Israeli patients with essential hypertension. Gerontology. 2004;50:315–21.
Alpert P, Osetinsky I, Ziv B, Shafir H. A new seasons definition based on classified daily synoptic systems: an example for the eastern Mediterranean. Int J Climatol. 2004;24:1013–21.
Sheps SG, Bailey KR, Zachariah PK. Short-term (six hour), ambulatory blood pressure monitoring. J Hum Hypertens. 1994;8:873–8.
Chanudet X, Chau NP, Larroque P. Short-term representatives of daytime and night-time ambulatory blood pressures. J Hypertens. 1992;10:595–600.
Wei Q, Sun J, Huang J, Zhou HY, Ding YM, Tao YC, et al. Prevalence of hypertension and associated risk factors in Dehui City of Jilin Province in China. J Hum Hypertens. 2015;29:64–8.
Ofili MI, Ncama BP, Sartorius B. Hypertension in rural communities in Delta State, Nigeria: prevalence, risk factors and barriers to health care. Afr J Prim Heal Care Fam Med. 2015;7:1–7.
Unnikrishnan S, Awadhiya O, Lahiri A, Pakhare AP, Joshi A, Joshi R. Accuracy of short-term ambulatory blood pressure measurements for the diagnosis of hypertension. Cureus. 2021;13:1–9.
Author information
Authors and Affiliations
Contributions
SZD—writing the protocol and report, conducting the search, screening potentially eligible studies, extracting and analysing data, interpreting results. MF—was responsible for designing the review protocol, analysing data and interpreting results. OB—She contributed to writing the report, extracting and analysing data, interpreting results. AB—contributed to data extraction and provided feedback on the report. TW—responsible for designing the review protocol, writing the protocol and report interpreting results.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zilka Darbiani, S., Friger, M., Barrett, O. et al. The accuracy of 8-hour ambulatory blood pressure monitoring, adjusted to seasons. J Hum Hypertens 37, 141–149 (2023). https://doi.org/10.1038/s41371-022-00790-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-022-00790-x
This article is cited by
-
Journal of Human Hypertension special issue on the accuracy of automated blood pressure measuring devices
Journal of Human Hypertension (2023)