Abstract
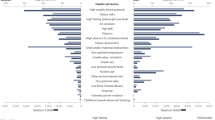
High blood pressure (BP) affects over one billion people and is the leading risk factor for global mortality. While many lifestyle and genetic risk factors are well-accepted to increase BP, the role of the external environment is typically overlooked. Mounting evidence now supports that numerous environmental factors can promote an elevation in BP. Broadly speaking these include aspects of the natural environment (e.g., cold temperatures, higher altitude, and winter season), natural disasters (e.g., earthquakes, volcanic eruptions), and man-made exposures (e.g., noise, air pollutants, and toxins/chemicals). This is important for health care providers to recognize as one (or several) of these environmental factors could be playing a clinically meaningful role in elevating BP or disrupting hypertension control among their patients. At the population level, certain environmental exposures may even be contributing to the growing pandemic of hypertension. Here we provide an updated review of the literature linking environment exposures with high BP and outline practical recommendations for clinicians.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, Naghavi M, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation. 2015;132:1667–78.
Rahimi K, Emdin CA, MacMahon S. The epidemiology of blood pressure and its worldwide management. Circ Res. 2015;116:925–36.
Bloch MJ. Worldwide prevalence of hypertension exceeds 1.3 billion. J Am Soc Hypertens. 2016;10:753–4.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et.al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017 (in press).
Taler SJ. Secondary causes of hypertension. Prim Care. 2008;35:489–500.
Akpunonu BE, Mulrow PJ, Hoffman EA. Secondary hypertension: evaluation and treatment. Dis Mon. 1996;42:609–722.
Bolívar JJ. Essential hypertension: an approach to its etiology and neurogenic pathophysiology. Int J Hypertens. 2013;2013:547809.
Gaziano TA. Cardiovascular disease in the developing world and its cost-effective management. Circulation. 2005;112:3547–53.
Bertrand E. Cardiovascular Disease in Developing Countries. New York, NY: McGraw-Hill; 1999.
Brundtland GH. The World Health Report 2002: reducing risks, promoting healthy life. Geneva: World Health Organization; 2002.
Muluneh AT, Haileamlak A, Tessema F, Alemseged F, Woldemichael K, Asefa M. Population based survey of chronic non-communicable diseases at gilgel gibe field research center, southwest Ethiopia. Ethiop J Health Sci. 2012;22(S):7–18.
Damasceno A, Azevedo A, Silva-Matos C, Prista A, Diogo D, Lunet N. Hypertension prevalence, awareness, treatment, and control in mozambique: urban/rural gap during epidemiological transition. Hypertension. 2009;54:77–83.
Dewhurst MJ, Dewhurst F, Gray WK, Chaote P, Orega GP, Walker RW. The high prevalence of hypertension in rural-dwelling Tanzanian older adults and the disparity between detection, treatment and control: a rule of sixths? J Hum Hypertens. 2013;27:374–80.
Iwelunmor J, Airhihenbuwa CO, Cooper R, Tayo B, Plange-Rhule J, Adanu R, et al. Prevalence, determinants and systems-thinking approaches to optimal hypertension control in West Africa. Glob Health. 2014;10:42.
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–50.
Jin C-N, Yu C-M, Sun J-P, Fang F, Wen Y-N, Liu M, et al. The healthcare burden of hypertension in Asia. Heart Asia. 2013;5:238–43.
Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension. 2006;47:296–308.
Appel LJ. Lifestyle modification as a means to prevent and treat high blood pressure. J Am Soc Nephrol. 2003;14:S99–S102.
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. American Heart Association. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–e603.
Münzel T, Sorensen M, Gori T, Schmidt F, Rao X, Brook J, et al. Environmental stressors and cardio-metabolic disease: part 1: epidemiologic evidence supporting a role for noise and air pollution and effects of mitigation strategies. Eur Heart J. 2017;38:550–6.
Brook RD, Newby DE, Rajagopalan S. Air pollution and cardiometabolic disease: an update and call for clinical trials. Am J Hypertens. 2017;31:1–10.
Brook RD. The environment and blood pressure. Cardiol Clin. 2017;35:213–21.
Wang Q, Li C, Guo Y, Barnett AG, Tong S, Phung D, et al. Environmental ambient temperature and blood pressure in adults: a systematic review and meta-analysis. Sci Total Environ. 2017;575:276–86.
Alpérovitch A, Lacombe J-M, Hanon O, Dartigues JF, Richtie K, Ducimetiere P, et al. Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals. The Three-City Study. Arch Intern Med. 2009;169:75–80.
Halonen JI, Zanobetti A, Sparrow D, Vokonas PS, Schwartz J. Relationship between outdoor temperature and blood pressure. Occup Environ Med. 2011;68:296–301.
Modesti PA, Borabito M, Bertolozzi I, Massetti L, Panci G, Lumachi C, et al. Weather-related changes in 24-hour blood pressure profle: effects of age and implications for hypertension management. Hypertension. 2006;47:1–7.
Sun Z. Cardiovascular responses to cold exposure. Front Biosci. 2010;2:495–503.
Saeki K, Obayashi K, Iwamoto J, Tone N, Okamoto N, Tomioka K, et al. Stronger association of indoor temperature than outdoor temperature with blood pressure in colder months. J Hypertens. 2014;32:1582–9.
Brook RD, Shin HH, Bard RL, Burnett R, Vette A, Croghan C, et al. Can personal exposures to higher nighttime and early morning temperatures increase blood pressure? J Clin Hypertens. 2011;13:881–8.
Lewington S, Li L, Sherliker P, Guo Y, Millwood I, Bian Z, et al. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: the China Kadoorie Biobank. J Hypertens. 2012;30:1383–91.
Yang L, Li L, Lewington S, Guo Y, Sherliker P, Bian Z, et al. Outdoor temperature, blood pressure, and cardiovascular disease mortality among 23000 individuals with diagnosed cardiovascular diseases from China. Eur Heart J. 2015;36:1178–85.
Su D, Du H, Zhang X, Qian Y, Chen L, Chen Y, et al. Season and outdoor temperature in relation to detection and control of hypertension in a large rural Chinese population. Int J Epidemiol. 2014;43:1835–45.
Chen Q, Wang J, Tian J, Tang X, Yu C, Marshall RJ, et al. Association between ambient temperature and blood pressure and blood pressure regulators: 1831 hypertensive patients followed up for three years. PLoS ONE. 2013;8:e84522.
van den Hurk K, de Kort WL, Deinum J, Atsma F. Higher outdoor temperatures are progressively associated with lower blood pressure: a longitudinal study in 100,000 healthy individuals. J Am Soc Hypertens. 2015;9:536–43.
Modesti PA, Morabito M, Massetti L, Rapi S, Orlandini S, Mancia G, et al. Seasonal blood pressure changes: an independent relationship with temperature and daylight hours. Hypertension. 2013;61:908–14.
Fedecostante M, Barbatelli P, Guerra F, Espinosa E, Dessì-Fulgheri P, Sarzani R. Summer does not always mean lower: seasonality of 24 h, daytime, and night-time blood pressure. J Hypertens. 2012;30:1392–8.
Giorgini P, Rubenfire M, Das R, Gracik T, Wang L, Morishita M, et al. Particulate matter air pollution and ambient temperature: opposing effects on blood pressure in high-risk cardiac patients. J Hypertens. 2015;33:2032–8.
Nafstad MC. Associations between environmental exposure and blood pressure among participants in the Oslo Health Study (HUBRO). Eur J Epidemiol. 2006;21:485–91.
Woodhouse PR, Khaw K-T, Plummer M. Seasonal variation of blood pressure and its relationship to ambient temperature in an elderly population. J Hypertens. 1993;11:1267–74.
Al-Tamre YY, Al-Hayali JMT, Al-Ramadhan EAH. Seasonality of hypertension. J Clin Hypert. 2008;10:125–9.
Rostand SG. Ultraviolet light may contribute to geographic and racial blood pressure differences. Hypertension. 1997;30:150–6.
Goldstein MR, Mascitelli L, Pezzetta F. Regarding the inverse relationship between blood pressure and outdoor temperature: it is the sun. Arch Intern Med. 2009;169:1167.
Algert CS, Roberts CL, Shand AW, Morris JM, Ford JB. Seasonal variation in pregnancy hypertension is correlated with sunlight intensity. Am J Obstet Gynecol. 2010;203:e211–5.
Handler J. Seasonal variability of blood pressure in California. J Clin Hypertens. 2011;13:856–60.
Charach G, Rabinovich PD, Weintraub M. Seasonal changes in blood pressure and frequency of related complications in elderly Israeli patients with essential hypertension. Gerontology. 2004;50:315–21.
Morabito M, Crisci A, Vallorani R, Modesti PA, Gensini GF, Orlandini S. Innovative approaches helpful to enhance knowledge on weather-related stroke events over a wide geographical area and a large population. Stroke. 2011;42:593–600.
Preval N, Keall M, Telfar-Barnard L, Grimes A, Howden-Chapman P. Impact of improved insulation and heating on mortality risk of older cohort members with prior cardiovascular or respiratory hospitalisations. BMJ Open. 2017;7:e018079.
Hasler E,Suter PM,Vetter W, Race specific altitude effects on blood pressure. J Hum Hypertens. 1997;11:435–8.
Sizlan A, Ogur R, Ozer M, et al. Blood pressure changes in young male subjects exposed to a median altitude. Clin Auton Res. 2008;18:84–89.
Handler J. Altitude-related hypertension. J Clin Hypertens. 2009;11:161–5.
Luks AM. Should travelers with hypertension adjust their medications when traveling to high altitude?. High Alt Med Biol. 2009;10:11–14.
Yanamandra U, Singh SP, Yanamandra S, Mulajkar D, Grewal RS, Singh S, et al. Endothelial markers in high altitude induced systemic hypertension (HASH) at moderate high altitude. Med J Armed Forces India. 2017;73:363–9.
Rimoldi SF, Sartori C, Seiler C, Delacretaz E, Mattle HP, Scherrer U, et al. High-altitude exposure in patients with cardiovascular disease: risk assessment and practical recommendations. Prog Cardiovasc Dis. 2010;52:512–24.
Dhar P, Sharma VK, Hota KB, Das SK, Hota SK, Srivastava RB, et al. Autonomic cardiovascular responses in acclimatized lowlanders on prolonged stay at high altitude: a longitudinal follow up study. PLoS ONE. 2014;9:e84274.
Mingji C, Onakpoya IJ, Perera R, Ward AM, Heneghan CJ. Relationship between altitude and the prevalence of hypertension in Tibet: a systematic review. Heart. 2015;101:1054–60.
Parati G, Bilo G, Faini A, Bilo B, Revera M, Giuliano A, et al. Changes in 24 h ambulatory blood pressure and effects of angiotensin II receptor blockade during acute and prolonged high-altitude exposure: a randomized clinical trial. Eur Heart J. 2014;35:3113–22.
Bilo G, Villafuerte FC, Faini A, Ana-Ramirez C, Giuliano A, Caravita S, et al. Ambulatory blood pressure in untreated and treated hypertensive patients at high altitude: the High Altitude Cardiovascular Research-Andes study. Hypertension. 2015;65:1266–72.
Burtscher M. Effects of living at higher altitudes on mortality: a narrative review. Aging Dis. 2013;5:274–80.
Bärtsch P, Swenson ER. Clinical practice: acute high-altitude illnesses. N Engl J Med. 2013;368:2294–302.
Bernabé-Ortiz A, Carrillo-Larco RM, Gilman RH, Checkley W, Smeeth L, Miranda JJ, CRONICAS Cohort Study Group. Impact of urbanisation and altitude on the incidence of, and risk factors for, hypertension. Heart. 2017;103:827–33.
Ashraf MZ. Hypertension at high altitude: the interplay between genetic and biochemical factors in the setting of oxidative stress. Hypertens Res. 2016;39:199–200.
Norboo T, Stobdan T, Tsering N, Angchuk N, Tsering P, Ahmed I, et al. Prevalence of hypertension at high altitude: cross-sectional survey in Ladakh, Northern India 2007-2011. BMJ Open. 2015;5:e007026.
Gilbert-Kawai E, Martin D, Grocott M, Levett D. High altitude-related hypertensive crisis and acute kidney injury in an asymptomatic healthy individual. Extrem Physiol Med. 2016;5:10.
Young JH. Evolution of blood pressure regulation in humans. Curr Hypertens Rep. 2007;9:13–8.
Shiue I, Shiue M. Indoor temperature below 18°C accounts for 9% population attributable risk for high blood pressure in Scotland. Int J Cardiol. 2014;171:e1–e2.
Elford J, Phillips A, Thomson AG, Shaper AG. Migration and geographic variations in blood pressure in Britain. BMJ. 1990;300:291–5.
Cabrera SE, Mindell JS, Toledo M, Alvo M, Ferro CJ. Associations of blood pressure with geographical latitude, solar radiation, and ambient temperature: results from the Chilean Health Survey, 2009-2010. Am J Epidemiol. 2016;183:1071–3.
Duranton F, Kramer A, Szwarc I, Bieber B, Gayrard N, Jover B, et al. Geographical variations in blood pressure level and seasonality in hemodialysis patients. Hypertension. 2018;71:289–96.
Ohira T, Hosoya M, Yasumura S, Satoh H, Suzuki H, Sakai A, Fukushima Health Management Survey Group. et al. Evacuation and risk of hypertension after the great east Japan earthquake: the Fukushima Health Management Survey. Hypertension. 2016;68:558–64.
Kario K. Disaster hypertension - its characteristics, mechanism, and management. Circ J. 2012;76:553–62.
Trevisan M, Celentano E, Meucci C, Farinaro E, Jossa F, Krogh V, et al. Short-term effect of natural disasters on coronary heart disease risk factors. Arteriosclerosis. 1986;6:491–4.
Trevisan M, Jossa F, Farinaro E, Krogh V, Panico S, Giumetti D, et al. Earthquake and coronary heart disease risk factors: a longitudinal study. Am J Epidemiol. 1992;135:632–7.
Saito K, Kim JI, Maekawa K, Ikeda Y, Yokoyama M. The great Hanshin-Awaji earthquake aggravates blood pressure control in treated hypertensive patients. Am J Hypertens. 1997;10:217–21.
Cwikel JG, Goldsmith JR, Kordysh E, Quastel M, Abdelgani A. Blood pressure among immigrants to Israel from areas affected by the Chernobyl disaster. Public Health Rev. 1997;25:317–35.
Bland SH, Farinaro E, Krogh V, Jossa F, Scottoni A, Trevisan M. Long term relations between earthquake experiences and coronary heart disease risk factors. Am J Epidemiol. 2000;151:1086–90.
Fonseca VA, Smith H, Kuhadiya N, Leger SM, Yau CL, Reynolds K, et al. Impact of a natural disaster on diabetes: Exacerbation of disparities and long-term consequences. Diabetes Care. 2009;32:1632–8.
Krousel-Wood MA, Islam T, Muntner P, Stanley E, Phillips A, Webber LS, et al. Medication adherence in older clinic patients with hypertension after Hurricane Katrina: implications for clinical practice and disaster management. Am J Med Sci. 2008;336:99–104.
Azuma T, Seki N, Tanabe N, Saito R, Honda A, Ogawa Y, et al. Prolonged effects of participation in disaster relief operations after the Mid-Niigata earthquake on increased cardiovascular risk among local governmental staff. J Hypertens. 2010;28:695–702.
Kario K, Matsuo T, Ishida T, Shimada K. “White coat” hypertension and the Hanshin-Awaji earthquake. Lancet. 1995;345:1365.
Kario K, Matsuo T, Shimada K. Follow-up of white-coat hypertension in the Hanshin-Awaji earthquake. Lancet. 1996;347:626–7.
Minami J, Kawano Y, Ishimitsu T, Yoshimi H, Takishita S. Effect of the Hanshin-Awaji earthquake on home blood pressure in patients with essential hypertension. Am J Hypertens. 1997;10:222–5.
Kamoi K, Tanaka M, Ikarashi T, Miyakoshi M. Effect of the 2004 Mid-Niigata Prefecture earthquake on home blood pressure measurement in the morning in type 2 diabetic patients. Clin Exp Hypertens. 2006;28:719–29.
Chen Y, Li J, Xian H, Li J, Liu S, Liu G, et al. Acute cardiovascular effects of the Wenchuan earthquake: ambulatory blood pressure monitoring of hypertensive patients. Hypertens Res. 2009;32:797–800.
Kario K, Matsuo T, Kobayashi H, Yamamoto K, Shimada K. Earthquake-induced potentiation of acute risk factors in hypertensive elderly patients: possible triggering of cardiovascular events after a major earthquake. J Am Coll Cardiol. 1997;29:926–33.
Yabe H, Suzuki Y, Mashiko H, Nakayama Y, Hisata M, Niwa S, et al. Mental Health Group of the Fukushima Health Management Survey. Psychological distress after the Great East Japan earthquake and Fukushima Daiichi Nuclear Power Plant accident: results of a mental health and lifestyle survey through the Fukushima Health Management Survey in FY2011 and FY2012. Fukushima J Med Sci. 2014;60:57–67.
Giorgini P, Striuli R, Petrarca M, Petrazzi L, Pasqualetti P, Properzi G, et al. Long-term blood pressure changes induced by the 2009 L’Aquila earthquake: assessment by 24 h ambulatory monitoring. Hypertens Res. 2013;36:795–8.
Baxter PJ, Baubron JC, Coutinho R. Health hazards and disaster potential of ground gas emissions at Furnas volcano, Sao Miguel, Azores. J Volcanol Geotherm Res. 1999;92:95–106.
Small C, Naumann T. The global distribution of human population and recent volcanism. Environ Hazard. 2001;3:93–109.
Williams-Jones G, Rymer H. Hazards of volcanic gases. In: Sigurdsson H, editor. Encyclopedia of volcanoes. San Diego: Academic Press; 2000. p. 997–1004.
Chow CD, Grandinetti A, Fernandez E, Sutton AJ, Elias T, Brooks B, et al. Is volcanic air pollution associated with decreased heart-rate variability? Heat Asia. 2010;2:36–41.
Hansell A, Oppenheimer C. Health hazards from volcanic gases: a systematic literature review. Arch Environ Health. 2004;59:628–39.
Sprowl GM. Hazards of Hawaii Volcanoes National Park. Hawaii J Med Public Health. 2014;73(11 Suppl 2):17–20.
Longo BM, Yang W, Green JB, Crosby FL, Crosby VL. Acute health effects associated with exposure to volcanic air pollution (vog) from increased activity at Kilauea Volcano in 2008. J Toxicol Environ Health A. 2010;73:1370–81.
Tam E, Miike R, Labrenz S, Sutton AJ, Elias T, Davis J, et al. Volcanic air pollution over the island of Hawaiʹi: Emissions, dispersal, and composition. Association with respiratory symptoms and lung function in HawaiʹI Island school children. Environ Intern. 2016;92-93:543–52.
Longo BM, Rossignol A, Green JB. Cardiorespiratory health effects associated with sulphurous volcanic air pollution. Public Health. 2008;122:809e20.
Longo BM. Adverse health effects associated with increased activity at Kilauea volcano: A repeated population-based survey. ISRN Public Health 2013; Article ID 475962.
United States Environmental Protection Agency, “National Ambient Air Quality Standards, Sulfur dioxide,” 2010, http://www.epa.gov/air/criteria.html.
WHO, WHO Air Quality Guidelines for Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide, Global Update 2005, Summary of Risk Assessment. World Health Organization, Geneva, Switzerland, 2006.
Yang BY, Qian Z, Howard SW, Vaughn MG, Fan SJ, Liu KK, et al. Global association between ambient air pollution and blood pressure: a systematic review and meta-analysis. Environ Pollut. 2018;235:576–88.
Sentell TL, Juarez DT, Ahn HJ, Tseng CW, Chen JJ, Salvail FR, et al. Disparities in diabetes-related preventable hospitalizations among working-age Native Hawaiians and Asians in Hawaii. Hawaii J Med Public Health. 2014;73(12 Suppl 3):8–13.
Maskarinec G, Jacobs S, Morimoto Y, Chock M, Grandinetti A, Kolonel LN. Disparity in diabetes risk across Native Hawaiians and different Asian groups: the multiethnic cohort. Asia Pac J Public Health. 2015;27:375–84.
Maskarinec G, Morimoto Y, Jacobs S, Grandinetti A, Mau MK, Kolonel LN. Ethnic admixture affects diabetes risk in native Hawaiians: the Multiethnic Cohort. Eur J Clin Nutr. 2016;70:1022–7.
H. C. R. State of Hawaii, House of Representatives, 23rd Legislature, House Concurrent Resolution H.C.R. No. 141, H.D. 1, 2005, http://www.capitol.hawaii.gov/session2005/bills/hcr141.htm.
Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliott CT. Critical review of health impacts of wildfire smoke exposure. Environ Health Perspect. 2016;124:1334–43.
Cascio WE. Wildland fire smoke and human health. Sci Total Environ. 2018;624:586–95.
Claeys MJ, Rajagopalan S, Nawrot TS, Brook RD. Climate and environmental triggers of acute myocardial infarction. Eur Heart J. 2016;38:955–60.
Kingsley SL, Eliot MN, Whitsel EA, Wang Y, Coull BA, Hou L, et al. Residential proximity to major roadways and incident hypertension in post-menopausal women. Environ Res. 2015;142:522–8.
Dimakopoulou K, Kotentakis K, Papagergiou I, Kasdagli MI, Haralabidis AS, Sourtzi P, et al. Is aircraft noise exposure associated with cardiovascular disease and hypertension? Results from a cohort study in Athens, Greece. Occup Environ Med. 2017;74:830–7.
Fuks KB, Weinmayr G, Basagaña X, Gruzieva O, Hampel R, Oftedal B, et al. Long-term exposure to ambient air pollution and traffic noise and incident hypertension in seven cohorts of the European study of cohorts for air pollution effects (ESCAPE). Eur Heart J. 2017;38:983–90.
Chang TY, Lai YA, Hsieh HH, Lai SJ, Lis CS. Effects of environmental noise exposure on ambulatory blood pressure in young adults. Environ Res. 2009;109:900–5.
Haraladbidis AS, Dimakopoulou K, Vigna-Taglianti F, Giampaolo M, Borgini A, Dudley ML, et al. Acute effects of night-time noise exposure on blood pressure in populations living near airports. Eur Heart J. 2008;29:658–64.
Davies HW, Vlaanderen JJ, Henderson SB, Brauer M. Correlation between co-exposures to noise and air pollution from traffic sources. Occup Environ Med. 2009;66:347–50.
Münzel T, Schmidt FP, Steven S, Herzog J, Daiber A, Sorensen M. Environmental noise and the cardiovascular system. J Am Coll Cardiol. 2018;71:688–97.
Münzel T, Gori T, Babisch W, Basner M. Cardiovascular effects of environmental noise exposure. Eur Heart J. 2014;35:829–36.
van Kempen E, Babisch W. The quantitative relationship between road traffic noise and hypertension: a meta-analysis. J Hypertens. 2012;30:1075–86.
Hammer MS, Swinburn TK, Neitzel RL. Environmental noise pollution in the United States: developing an effective public health response. Environ Health Perspect. 2014;122:115–9.
Foraster M, Künzli N, Aguilera I, Rivera M, Agis D, Vila J, et al. High blood pressure and long-term exposure to indoor noise and air pollution from road traffic. Environ Health Perspect. 2014;122:1193–200.
Stansfeld SA. Noise effects on health in the context of air pollution exposure. Int J Environ Res Public Health. 2015;12:12735–60.
Babisch W, Wolf K, Petz M, Heinrich J, Cyrys J, Peters A. Associations between traffic noise, particulate air pollution, hypertension, and isolated systolic hypertension in adults: the KORA study. Environ Health Perspect. 2014;122:492–8.
Akinseye OA, Williams SK, Seixas A, Pandi-Perumal SR, Vallon J, Zizi F, et al. Sleep as a mediator in the pathway linking environmental factors to hypertension: a review of the literature. Int J Hypertens. 2015;2015:926414.
Schmidt F, Kolle K, Kreuder K, Schnorbus B, Wild P, Hechtner M, et al. Nighttime aircraft noise impairs endothelial function and increases blood pressure in patients with or at high risk for coronary artery disease. Clin Res Cardiol. 2015;104:23–30.
Münzel T, Sørensen M, Gori T, Schmidt FP, Rao X, Brook JR, et al. Environmental stressors and cardio-metabolic disease: part II-mechanistic insights. Eur Heart J. 2017;38:557–64.
Halonen JI, Hansell AL, Gulliver J, Morley D, Blangiardo M, Fecht D, et al. Road traffic noise is associated with increased cardiovascular morbidity and mortality and all-cause mortality in London. Eur Heart J. 2015;36:2653–61.
Correia AW, Peters JL, Levy JI, Melly S, Dominici F. Residential exposure to aircraft noise and hospital admissions for cardiovascular diseases: multi-airport retrospective study. BMJ. 2013;347:f5561.
Kempen EV, Casas M, Pershagen G, Foraster M. WHO Environmental Noise Guidelines for the European Region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int J Environ Res Public Health. 2018;15(2) pii: E379.
Brown AL, van Kamp I. WHO environmental noise guidelines for the European region: a systematic review of transport noise interventions and their impacts on health. Int J Environ Res Public Health. 2017;14 pii: E873.
Lind PM, Penell J, Salihovic S, van Bavel B, Lind L. Circulating levels of p, p’-DDE are related to prevalent hypertension in the elderly. Environ Res. 2014;129:27–31.
Valera B, Ayotte P, Poirier P, Dewailly E. Associations between plasma persistent organic pollutant levels and blood pressure in Inuit adults from Nunavik. Environ Int. 2013;59:282–9.
Park SH, Lim J-E, Park H, Jee SH. Body burden of persistent organic pollutants on hypertension: a meta-analysis. Environ Sci Poll Res. 2016;23:14284–93.
Ha MH, Lee DH, Son HK, Jacobs DR Jr. Association between serum concentrations of persistent organic pollutants and prevalence of newly diagnosed hypertension: results from the National Health and Nutrition Examination Survey 1999–2002. J Hum Hypertens. 2009;23:274–86.
Everett CJ, Mainous AG 3rd, Frithsen IL, Player MS, Matheson EM. Association of polychlorinated biphenyls with hypertension in the 1999–2002 National Health and Nutrition Examination Survey. Environ Res. 2008;108:94–97.
Valera B, Jørgensen ME, Jeppesen C, Bjerregaard P. Exposure to persistent organic pollutants and risk of hypertension among Inuit from Greenland. Environ Res. 2013;122:65–73.
Shankar A, Teppala S. Urinary bisphenol A and hypertension in a multiethnic sample of US adults. J Environ Public Health. 2012;2012:481641.
Bae S, Kim JH, Lim Y-H, Park HY, Hong Y-C. Associations of Bisphenol A exposure with heart rate variability and blood pressure. Hypertension. 2012;60:786–93.
Bae S, Hong YC. Exposure to bisphenol A from drinking canned beverages increases blood pressure: randomized crossover trial. Hypertension. 2015;65:313–9.
Trasande L, Attina TM. Association of exposure to di-2-ethylhexylphthalate replacements with increased blood pressure in children and adolescents. Hypertension. 2015;66:301–8.
Shiue I, Hristova K. Higher urinary heavy metal, phthalate and arsenic concentrations accounted for 3–19% of the population attributable risk for high blood pressure: US NHANES, 2009–2012. Hypertens Res. 2014;37:1075–81.
Han C, Hong YC. Bisphenol A, hypertension, and cardiovascular diseases: epidemiological, laboratory, and clinical trial evidence. Curr Hypertens Rep. 2016;18:11.
Gore AC, Chappell VA, Fenton SE, Flaws JA, Nadal A, Prins GS, et al. Executive summary to EDC-2: the endocrine society’s second scientific statement on endocrine-disrupting chemicals. Endocr Rev. 2015;36:593–602.
Wu W, Jiang S, Zhao Q, Zhang K, Wei X, Zhou T, et al. Environmental exposure to metals and the risk of hypertension: a cross-sectional study in China. Environ Pollut. 2018;233:670–8.
Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389:1907–18.
Giorgini P, Di Giosia P, Grassi D, Rubenfire M, Brook RD, Ferri C. Air pollution exposure and blood pressure: an updated review of the literature. Curr Pharm Des. 2015;22:28–51.
Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an Update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–78.
Brook RD, Sun Z, Brook JR, Zhao X, Ruan Y, Yan J, et al. Extreme air pollution conditions adversely affect blood pressure and insulin resistance: the air pollution and cardiometabolic disease study. Hypertension. 2016;67:77–85.
Rich DQ, Kipen HM, Huang W, Wang G, Wang Y, Zhu P, et al. Association between changes in air pollution levels during the Beijing Olympics and biomarkers of inflammation and thrombosis in healthy young adults. JAMA. 2012;307:2068–78.
Liang R, Zhang B, Zhao X, Ruan Y, Lian H, Fan Z. Effect of exposure to PM2.5 on blood pressure: a systematic review and meta-analysis. J Hypertens. 2014;32:2130–40.
Chen H, Burnett RT, Kwong JC, Villeneuve PJ, Goldberg MS, Brook RD, et al. Spatial association between ambient fine particulate matter and incident hypertension. Circulation. 2014;129:562–9.
Coogan PF, White LF, Jerrett M, Brook RD, Su JG, Seto E, et al. Air pollution and incidence of hypertension and diabetes mellitus in black women living in Los Angeles. Circulation. 2012;125:767–72.
Pope CA 3rd, Turner MC, Burnett RT, Jerrett M, Gapstur SM, Diver WR, et al. Relationships between fine particulate air pollution, cardiometabolic disorders, and cardiovascular mortality. Circ Res. 2015;116:108–15.
Brook RD, Kousha T. Air pollution and emergency department visits for hypertension in edmonton and calgary, canada: a case-crossover study. Am J Hypertens. 2015;28:1121–6.
Morishita M, Thompson KC, Brook RD. Understanding air pollution and cardiovascular diseases: is it preventable? Curr Cardiovasc Risk Rep. 2015;9:30.
Cai Y, Zhang B, Ke W, Feng B, Lin H, Xiao J, et al. Associations of short-term and long-term exposure to ambient air pollutants with hypertension: a systematic review and meta-analysis. Hypertension. 2016;68:62–70.
United Nations. The World’s Cities in 2016 – Data Booklet (ST/ESA/SER.A/392). United Nations, Department of Economic and Social Affairs, Population Division, New York, NY, 2016.
Diez Roux AV. Residential environments and cardiovascular risk. J Urban Health. 2003;80:569–89.
Leal C, Chaix B. The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obes Rev. 2011;12:217–30.
Sallis JF, Floyd MF, Rodríguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125:729–37.
Sarkar C, Webster C. Urban environments and human health: current trends and future directions. Curr Opin Environ Sustain . 2017;25:33–44.
Ewing R, Cervero R. Travel and the built environment: a synthesis. Transp Res Rec: J Transp Res Board. 2001;1780:87–114.
Lee C, Moudon AV. The 3Ds+R: quantifying land use and urban form correlates of walking. Transp Res Part D: Transp Environ. 2006;11:204–15.
Booth GL, Creatore MI, Moineddin R, Gozdyra P, Weyman JT, Matheson FI, et al. Unwalkable neighborhoods, poverty, and the risk of diabetes among recent immigrants to Canada compared with long-term residents. Diabetes Care. 2013;36:302–8.
Frank L, Engelke P, Schmid T. Health and Community Design: The Impact of the Built Environment on Physical Activity. Washington DC: Island Press; 2003.
Frank LD, Sallis JF, Conway TL, Chapman JE, Saelens BE, Bachman W. Many pathways from land use to health: associations between neighborhood walkability and active transportation, body mass index, and air quality. J Am Plan Assoc. 2006;72:75–87.
Sarkar C, Webster C, Gallacher J. Healthy Cities: Public Health Through Urban Planning. Cheltenham, UK: Edward Elgar Publishing; 2014.
Chiu M, Rezai M-R, Maclagan LC, Austin PC, Shah BR, Redelmeier DA, et al. Moving to a highly walkable neighborhood and incidence of hypertension: a propensity-score matched cohort study. Environ Health Perspect. 2016;124:754.
Loo CJ, Greiver M, Aliarzadeh B, Lewis D. Association between neighbourhood walkability and metabolic risk factors influenced by physical activity: a cross-sectional study of adults in Toronto, Canada. BMJ. 2017;Open7:e013889.
Mujahid MS, Roux AVD, Morenoff JD, Raghunathan TE, Cooper RS, Ni H, et al. Neighborhood characteristics and hypertension. Epidemiology. 2008;19:590–8.
Kaiser P, Diez Roux AV, Mujahid M, Carnethon M, Bertoni A, Adar SD, et al. Neighborhood environments and incident hypertension in the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2016;183:988–97.
Sarkar, C, International Journal of Hygiene and Environmental Health. 2018. (In Press) https://doi.org/10.1016/j.ijheh.2018.01.009
Coffee NT, Howard N, Paquet C, Hugo G, Daniel M. Is walkability associated with a lower cardiometabolic risk? Health Place. 2013;21:163–9.
Azuma K, Ikeda K, Kagi N, Yanagi U, Osawa H. Prevalence and risk factors associated with nonspecific building-related symptoms in office employees in Japan: relationships between work environment, Indoor Air Quality, and occupational stress. Indoor Air. 2015;25:499–511.
Mitter SS, Vedanthan R, Islami F, Pourshams A, Khademi H, Kamangar F, et al. Household fuel use and cardiovascular disease mortality: Golestan Cohort Study. Circulation. 2016;133:2360–9.
Song X, Ma W, Xu X, Liu T, Xiao J, Zeng W, et al. The association of domestic incense burning with hypertension and blood pressure in Guangdong, China. Int J Environ Res Public Health. 2017;14:788.
Baumgartner J, Schauer JJ, Ezzati M, Lu L, Cheng C, Patz JA, et al. Indoor air pollution and blood pressure in adult women living in rural China. Environ Health Perspect. 2011;119:1390–5.
Houston MC. Role of mercury toxicity in hypertension, cardiovascular disease, and stroke. J Clin Hypertens. 2011;13:621–7.
Norsk P, Asmar A, Damgaard M, Christensen NJ. Fluid shifts, vasodilatation and ambulatory blood pressure reduction during long duration spaceflight. J Physiol. 2015;593:573–84.
Talukder MR, Rutherford S, Huang C, Phung D, Islam MZ, Chu C. Drinking water salinity and risk of hypertension: a systematic review and meta-analysis. Arch Environ Occup Health. 2017;72:126–38.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
R.D.B. Inc. investigator initiate grant.
Rights and permissions
About this article
Cite this article
Sharma, P., Brook, R.D. Echoes from Gaea, Poseidon, Hephaestus, and Prometheus: environmental risk factors for high blood pressure. J Hum Hypertens 32, 594–607 (2018). https://doi.org/10.1038/s41371-018-0078-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-018-0078-6
This article is cited by
-
Climate change and cardiovascular disease: implications for global health
Nature Reviews Cardiology (2022)
-
Reducing cardiovascular risk caused by air pollution: individuals can make a difference
Journal of Human Hypertension (2020)
-
Clearing the air to treat hypertension
Journal of Human Hypertension (2020)