Abstract
Background/Objectives
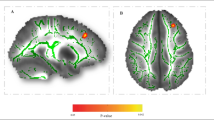
With rising obesity rates among pregnant women, more children are exposed in utero to maternal obesity. In prior epidemiological studies, exposure to maternal obesity was associated with lower intelligence quotient (IQ) scores and worse cognitive abilities in offspring. Further studies have shown that offspring exposed to maternal obesity, exhibit differences in the white matter microstructure properties, fractional anisotropy (FA) and mean diffusivity (MD). In contrast, physical activity was shown to improve cognition and white matter microstructure during childhood. We examined if child physical activity levels modify the relationship between prenatal exposure to maternal obesity with IQ and white matter microstructure in offspring.
Subjects/Methods
One hundred children (59% girls) age 7–11 years underwent brain magnetic resonance imaging and IQ testing. Maternal pre-pregnancy BMI was abstracted from electronic medical records. White matter was assessed using diffusion tensor imaging with the measures, global FA, MD. The 3-day physical activity recall was used to measure moderate-to-vigorous physical activity and vigorous physical activity (VPA). Linear regression was used to test for interactions between prenatal exposure to maternal overweight/obesity and child PA levels on child IQ and global FA/MD.
Results
The relationship between prenatal exposure to maternal overweight/obesity and child IQ and global FA varied by child VPA levels. Children exposed to mothers with overweight/obesity who engaged in more VPA had higher IQ scores and global FA compared to exposed children who engaged in less VPA. Associations were independent of child age, sex, BMI Z-score and socioeconomic status. Children born to normal-weight mothers did not differ in either IQ or global FA by time in VPA.
Conclusions
Our findings support findings in rodent models and suggest that VPA during childhood modifies the relationship between prenatal exposure to maternal obesity and child IQ and white matter microstructure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author (KAP), on reasonable request.
References
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–14.
Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA. 2018;319:1723.
Bider-Canfield Z, Martinez MP, Wang X, Yu W, Bautista MP, Brookey J, et al. Maternal obesity, gestational diabetes, breastfeeding and childhood overweight at age 2 years: maternal exposures and childhood overweight. Pediatr Obes. 2017;12:171–8.
Mingrone G, Manco M, Mora MEV, Guidone C, Iaconelli A, Gniuli D, et al. Influence of maternal obesity on insulin sensitivity and secretion in offspring. Diabetes Care. 2008;31:1872–6.
Alves JM, Luo S, Chow T, Herting M, Xiang AH, Page KA. Sex differences in the association between prenatal exposure to maternal obesity and hippocampal volume in children. Brain Behav. 2020;10:e01522.
Basatemur E, Gardiner J, Williams C, Melhuish E, Barnes J, Sutcliffe A. Maternal prepregnancy BMI and child cognition: a longitudinal cohort study. Pediatrics. 2013;131:56–63.
Casas M, Chatzi L, Carsin A-E, Amiano P, Guxens M, Kogevinas M, et al. Maternal pre-pregnancy overweight and obesity, and child neuropsychological development: two Southern European birth cohort studies. Int J Epidemiol. 2013;42:506–17.
Huang L, Yu X, Keim S, Li L, Zhang L, Zhang J. Maternal prepregnancy obesity and child neurodevelopment in the Collaborative Perinatal Project. Int J Epidemiol. 2014;43:783–92.
Neggers YH, Goldenberg RL, Ramey SL, Cliver SP. Maternal prepregnancy body mass index and psychomotor development in children. Acta Obstet Gynecol Scand. 2003;82:235–40.
Tanda R, Salsberry PJ, Reagan PB, Fang MZ. The impact of prepregnancy obesity on children’s cognitive test scores. Matern Child Health J. 2013;17:222–9.
Widen EM, Kahn LG, Cirillo P, Cohn B, Kezios KL, Factor-Litvak P. Prepregnancy overweight and obesity are associated with impaired child neurodevelopment. Matern Child Nutr. 2018;14:e12481.
Ou X, Thakali KM, Shankar K, Andres A, Badger TM. Maternal adiposity negatively influences infant brain white matter development. Obes Silver Spring Md. 2015;23:1047–54.
Rosen ML, Sheridan MA, Sambrook KA, Meltzoff AN, McLaughlin KA. Socioeconomic disparities in academic achievement: a multi-modal investigation of neural mechanisms in children and adolescents. NeuroImage. 2018;173:298–310.
Arden R, Plomin R. Sex differences in variance of intelligence across childhood. Personal Individ Differ. 2006;41:39–48.
Yau PL, Kang EH, Javier DC, Convit A. Preliminary evidence of cognitive and brain abnormalities in uncomplicated adolescent obesity: brain alterations in adolescent obesity. Obesity. 2014;22:1865–71.
Bunketorp Käll L, Malmgren H, Olsson E, Lindén T, Nilsson M. Effects of a curricular physical activity intervention on children’s school performance, wellness, and brain development. J Sch Health. 2015;85:704–13.
Davis CL, Tomporowski PD, McDowell JE, Austin BP, Miller PH, Yanasak NE, et al. Exercise improves executive function and achievement and alters brain activation in overweight children: a randomized, controlled trial. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 2011;30:91–8.
Have M, Nielsen JH, Ernst MT, Gejl AK, Fredens K, Grøntved A, et al. Classroom-based physical activity improves children’s math achievement – a randomized controlled trial. Plos ONE. 2018;13:e0208787.
Huang T, Tarp J, Domazet SL, Thorsen AK, Froberg K, Andersen LB, et al. Associations of adiposity and aerobic fitness with executive function and math performance in Danish adolescents. J Pediatr. 2015;167:810–5.
Raine LB, Khan NA, Drollette ES, Pontifex MB, Kramer AF, Hillman CHObesity. Visceral adipose tissue, and cognitive function in childhood. J Pediatr. 2017;187:134–140.e3.
Reed JA, Einstein G, Hahn E, Hooker SP, Gross VP, Kravitz J. Examining the impact of integrating physical activity on fluid intelligence and academic performance in an elementary school setting: a preliminary investigation. J Phys Act Health. 2010;7:343–51.
Makharia A, Nagarajan A, Mishra A, Peddisetty S, Chahal D, Singh Y. Effect of environmental factors on intelligence quotient of children. Ind Psychiatry J. 2016;25:189–94.
El-Kholy T, Elsayed E. Association of physical activity and health status with intelligence quotient of high school students in Jeddah. J Phys Ther Sci. 2015;27:2039–43.
Pindus DM, Drollette ES, Scudder MR, Khan NA, Raine LB, Sherar LB, et al. Moderate-to-vigorous physical activity, indices of cognitive control, and academic achievement in preadolescents. J Pediatr. 2016;173:136–42.
Pindus DM, Davis RDM, Hillman CH, Bandelow S, Hogervorst E, Biddle SJH, et al. The relationship of moderate-to-vigorous physical activity to cognitive processing in adolescents: findings from the ALSPAC birth cohort. Psychol Res. 2015;79:715–28.
Donnelly JE, Hillman CH, Greene JL, Hansen DM, Gibson CA, Sullivan DK, et al. Physical activity and academic achievement across the curriculum: results from a 3-year cluster-randomized trial. Prev Med. 2017;99:140–5.
Konijnenberg C, Fredriksen PM. The effects of a school-based physical activity intervention programme on children’s executive control: The Health Oriented Pedagogical Project (HOPP). Scand J Public Health. 2018;46:82–91.21_suppl.
Krafft CE, Schaeffer DJ, Schwarz NF, Chi L, Weinberger AL, Pierce JE, et al. Improved frontoparietal white matter integrity in overweight children is associated with attendance at an after-school exercise program. Dev Neurosci. 2014;36:1–9.
Urger SE, De Bellis MD, Hooper SR, Woolley DP, Chen SD, Provenzale J. The superior longitudinal fasciculus in typically developing children and adolescents: diffusion tensor imaging and neuropsychological correlates. J Child Neurol. 2015;30:9–20.
Kim T-W, Park H-S. Physical exercise improves cognitive function by enhancing hippocampal neurogenesis and inhibiting apoptosis in male offspring born to obese mother. Behav Brain Res. 2018;347:360–7.
Irby SM, Floyd RG. Test review: Wechsler abbreviated scale of intelligence, second edition. 2011; San Antonio, TX: Pearson. Can J Sch Psychol. 2013;28:295–9.
Tamnes CK, Roalf DR, Goddings A-L, Lebel C. Diffusion MRI of white matter microstructure development in childhood and adolescence: methods, challenges and progress. Dev Cogn Neurosci. 2018;33:161–75.
Page KA, Luo S, Wang X, Chow T, Alves J, Buchanan TA, et al. Children exposed to maternal obesity or gestational diabetes mellitus during early fetal development have hypothalamic alterations that predict future weight gain. Diabetes Care. 2019;42:1473–80.
Han E, Abrams B, Sridhar S, Xu F, Hedderson M. Validity of self-reported pre-pregnancy weight and body mass index classification in an integrated health care delivery system. Paediatr Perinat Epidemiol. 2016;30:314–9.
CDC. Defining adult overweight and obesity. Overweight & Obesity. 2018, https://www.cdc.gov/obesity/adult/defining.html.
CDC. About child & teen BMI. Healthy Weight. 2018, https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html.
Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44:291–303.
Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970;45:13–23.
Rasmussen AR, Wohlfahrt-Veje C, Tefre De Renzy-Martin K, Hagen CP, Tinggaard J, Mouritsen A, et al. Validity of self-assessment of pubertal maturation. Pediatrics. 2015;135:86–93.
Pate RR, Ross R, Dowda M, Trost SG, Sirard JR. Validation of a 3-day physical activity recall instrument in female youth. Pediatr Exerc Sci. 2003;15:257–65.
Hearst M, Sirard J, Lytle L, Dengel D, Berrigan D. Comparison of three measures of physical activity and associations with blood pressure, HDL and body composition in a sample of adolescents. J Phys Act Health. 2012;9:78–85.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Tudor-Locke C, et al. 2011 compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exercise. 2011;43:1575–81.
Powell KE, Roberts AM, Ross JG, Phillips MAC, Ujamaa DA, Zhou M. Low physical fitness among fifth- and seventh-grade students, Georgia, 2006. Am J Prev Med. 2009;36:304–10.
Dollman J, Stanley R, Wilson A. The concurrent validity of the 3-day physical activity recall in Australian youth. Pediatr Exerc Sci. 2015;27:262–7.
Pavlidou S, Michalopoulou M, Aggelousis N, Taxildaris K, Bounova A. Convergent validity and reliability of a three-day physical activity record in greek children. Int Q Sport Sci. 2010;1–8.
Smith SM, Jenkinson M, Woolrich MW, Beckmann CF, Behrens TEJ, Johansen-Berg H, et al. Advances in functional and structural MR image analysis and implementation as FSL. NeuroImage. 2004;23:S208–19.
Smith SM. Fast robust automated brain extraction. Hum Brain Mapp. 2002;17:143–55.
Cabeen RP, Laidlaw DH, Toga AW. Quantitative imaging toolkit: software for interactive 3D visualization, processing, and analysis of neuroimaging datasets. Proc Intl Soc Mag Reson Med. 2018. Abstract number 2854.
Smith SM, Jenkinson M, Johansen-Berg H, Rueckert D, Nichols TE, Mackay CE, et al. Tract-based spatial statistics: voxelwise analysis of multi-subject diffusion data. Neuroimage. 2006;31:1487–1505.
Andersson JL, Jenkinson M, and Smith S. Non-linear registration, aka Spatial normalisation FMRIB technical report TR07JA2. FMRIB Anal Group Univ Oxf. https://www.fmrib.ox.ac.uk/datasets/techrep/tr07ja2/tr07ja2.pdf.
Winkler AM, Ridgway GR, Webster MA, Smith SM, Nichols TE. Permutation inference for the general linear model. NeuroImage. 2014;92:381–97.
Dimond D, Rohr CS, Smith RE, Dhollander T, Cho I, Lebel C, et al. Early childhood development of white matter fiber density and morphology. NeuroImage. 2020;210:116552.
Wang Y, Adamson C, Yuan W, Altaye M, Rajagopal A, Byars AW, et al. Sex differences in white matter development during adolescence: a DTI study. Brain Res. 2012;1478:1–15.
Smith SM, Nichols TE. Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. NeuroImage. 2009;44:83–98.
Hua K, Zhang J, Wakana S, Jiang H, Li X, Reich DS, et al. Tract probability maps in stereotaxic spaces: analyses of white matter anatomy and tract-specific quantification. NeuroImage. 2008;39:336–47.
Chaddock-Heyman L, Erickson KI, Kienzler C, Drollette ES, Raine LB, Kao S-C, et al. Physical activity increases white matter microstructure in children. Front Neurosci. 2018;12:950.
Rodriguez-Ayllon M, Cornejo IE, Verdejo-Román J, Muetzel RL, Migueles JH, Mora-Gonzalez J, et al. Physical activity, sedentary behavior, and white matter microstructure in children with overweight or obesity. Med Sci Sports Exerc. 2020;52:1218–26.
Rodriguez-Ayllon M, Derks IPM, van den Dries MA, Esteban-Cornejo I, Labrecque JA, Yang-Huang J, et al. Associations of physical activity and screen time with white matter microstructure in children from the general population. NeuroImage. 2020;205:116258.
Snook L, Paulson L-A, Roy D, Phillips L, Beaulieu C. Diffusion tensor imaging of neurodevelopment in children and young adults. NeuroImage. 2005;26:1164–73.
Bava S, Thayer R, Jacobus J, Ward M, Jernigan TL, Tapert SF. Longitudinal characterization of white matter maturation during adolescence. Brain Res. 2010;1327:38–46.
Bockhorst KH, Narayana PA, Liu R, Ahobila-Vijjula P, Ramu J, Kamel M, et al. Early postnatal development of rat brain: in vivo diffusion tensor imaging. J Neurosci Res. 2008;86:1520–8.
Kumar R, Nguyen HD, Macey PM, Woo MA, Harper RM. Regional brain axial and radial diffusivity changes during development. J Neurosci Res. 2012;90:346–55.
Chaddock-Heyman L, Erickson KI, Holtrop JL, Voss MW, Pontifex MB, Raine LB, et al. Aerobic fitness is associated with greater white matter integrity in children. Front Hum Neurosci. 2014;8:584.
Ruotsalainen I, Gorbach T, Perkola J, Renvall V, Syväoja HJ, Tammelin TH, et al. Physical activity, aerobic fitness, and brain white matter: their role for executive functions in adolescence. Dev Cogn Neurosci. 2020;42:100765.
Erickson KI, Voss MW, Prakash RS, Basak C, Szabo A, Chaddock L, et al. Exercise training increases size of hippocampus and improves memory. Proc Natl Acad Sci USA. 2011;108:3017–22.
Etnier JL, Wideman L, Labban JD, Piepmeier AT, Pendleton DM, Dvorak KK, et al. The effects of acute exercise on memory and brain-derived neurotrophic factor (BDNF). J Sport Exerc Psychol. 2016;38:331–40.
Moon HY, Becke A, Berron D, Becker B, Sah N, Benoni G, et al. Running-induced systemic Cathepsin B secretion is associated with memory function. Cell Metab. 2016;24:332–40.
Park H-S, Park S-S, Kim C-J, Shin M-S, Kim T-W. Exercise alleviates cognitive functions by enhancing hippocampal insulin signaling and neuroplasticity in high-fat diet-induced obesity. Nutrients. 2019;11:1603.
Jeong J-H, Koo J-H, Cho J-Y, Kang E-B. Neuroprotective effect of treadmill exercise against blunted brain insulin signaling, NADPH oxidase, and Tau hyperphosphorylation in rats fed a high-fat diet. Brain Res Bull. 2018;142:374–83.
Sauder KA, Hockett CW, Ringham BM, Glueck DH, Dabelea D. Research: epidemiology fetal overnutrition and offspring insulin resistance and β-cell function: the Exploring Perinatal Outcomes among Children (EPOCH) study. Diabet Med J Br Diabet Assoc. 2017;34:1392–9.
Cockcroft EJ, Williams CA, Tomlinson OW, Vlachopoulos D, Jackman SR, Armstrong N, et al. High intensity interval exercise is an effective alternative to moderate intensity exercise for improving glucose tolerance and insulin sensitivity in adolescent boys. J Sci Med Sport. 2015;18:720–4.
Jelleyman C, Edwardson CL, Henson J, Gray LJ, Rowlands AV, Khunti K, et al. Associations of physical activity intensities with markers of insulin sensitivity. Med Sci Sports Exerc. 2017;49:2451–8.
Rynders CA, Weltman JY, Jiang B, Breton M, Patrie J, Barrett EJ, et al. Effects of exercise intensity on postprandial improvement in glucose disposal and insulin sensitivity in prediabetic adults. J Clin Endocrinol Metab. 2014;99:220–8.
Belcher BR, Berrigan D, Dodd KW, Emken BA, Chou C-P, Spuijt-Metz D. Physical activity in US youth: impact of race/ethnicity, age, gender, & weight status. Med Sci Sports Exerc. 2010;42:2211–21.
Acknowledgements
The authors would like to thank the families who participate in the BrainChild Study. The authors would also like to thank Ana Romero for managing the BrainChild study, Alexis Defendis for study assistance, Mayra Martinez and Janet Mora-Marquez for recruiting volunteers, the staff at Dana and David Dornsife Cognitive Neuroimaging Center at USC and the staff at the USC Diabetes and Obesity Research Institute.
Funding
This work was supported by an American Diabetes Association Pathway Accelerator Award (#1-14-ACE-36) (PI: KAP) and in part by the National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) R01DK116858 (PIs: KAP, AHX) and the National Institute Of Mental Health of the National Institutes of Health under Award Number F31MH115640 (PI: JMA). A Research Electronic Data Capture, REDCap, database was used for this study, which is supported by the Southern California Clinical and Translational Science Institute (SC CTSI) through NIH UL1TR001855.
Author information
Authors and Affiliations
Contributions
KAP and AHX had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis; KAP, SL and AHX contributed to study concept and design; JMA, KAP and AHX drafted the manuscript; All authors critically revised the manuscript for intellectual content; Statistical and neuroimaging analyses were performed by JMA, BCA, JZ, TC, and AHX; MMH, and KC provided content knowledge and feedback for neuroimaging analyses; BRB and CDC provided content knowledge and feedback for physical activity and statistical methodology; KAP and AHX obtained funding; KAP and AHX provided study supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Alves, J.M., Angelo, B.C., Zink, J. et al. Child physical activity as a modifier of the relationship between prenatal exposure to maternal overweight/obesity and neurocognitive outcomes in offspring. Int J Obes 45, 1310–1320 (2021). https://doi.org/10.1038/s41366-021-00794-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00794-6