Abstract
Objective
To gain greater insights in the etiology and clinical consequences of altered cardiac function in obese adolescents. Therefore, we aimed to examine cardiac structure and function in obese adolescents, and to examine associations between altered cardiac function/structure and cardiometabolic disease risk factors or cardiopulmonary exercise capacity.
Methods
In 29 obese (BMI 31.6 ± 4.2 kg/m², age 13.4 ± 1.1 years) and 29 lean (BMI 19.5 ± 2.4 kg/m², age 14.0 ± 1.5 years) adolescents, fasted blood samples were collected to study hematology, biochemistry, liver function, glycemic control, lipid profile, and hormones, followed by a transthoracic echocardiography to assess cardiac structure/function, and a cardiopulmonary exercise test (CPET) to assess cardiopulmonary exercise parameters. Regression analyses were applied to examine relations between altered echocardiographic parameters and blood parameters or CPET parameters in the entire group.
Results
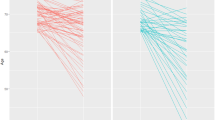
In obese adolescents, left ventricular septum thickness, left atrial diameter, mitral A-wave velocity, E/e’ ratio were significantly elevated (p < 0.05), as opposed to lean controls, while mitral e’-wave velocity was significantly lowered (p < 0.01). Elevated homeostatic model assessment of insulin resistance and blood insulin, c-reactive protein, and uric acid concentrations (all significantly elevated in obese adolescents) were independent risk factors for an altered cardiac diastolic function (p < 0.01). An altered cardiac diastolic function was not related to exercise tolerance but to a delayed heart rate recovery (HRR; p < 0.01).
Conclusions
In obese adolescents, an altered cardiac diastolic function was independently related to hyperinsulinemia and whole-body insulin resistance, and only revealed by a delayed HRR during CPET. This indicates that both hyperinsulinemia, whole-body insulin resistance, and delayed HRR could be regarded as clinically relevant outcome parameters.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766-81.
Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11–25.
McCrindle BW. Cardiovascular consequences of childhood obesity. Can J Cardiol. 2015;31:124–30.
Herouvi D, Karanasios E, Karayianni C, Karavanaki K. Cardiovascular disease in childhood: the role of obesity. Eur J Pediatr. 2013;172:721–32.
Ingul CB, Tjonna AE, Stolen TO, Stoylen A, Wisloff U. Impaired cardiac function among obese adolescents: effect of aerobic interval training. Arch Pediatr Adolesc Med. 2010;164:852–9.
Bjorge T, Engeland A, Tverdal A, Smith GD. Body mass index in adolescence in relation to cause-specific mortality: a follow-up of 230,000 Norwegian adolescents. Am J Epidemiol. 2008;168:30–7.
Chinali M, de Simone G, Roman MJ, Lee ET, Best LG, Howard BV, et al. Impact of obesity on cardiac geometry and function in a population of adolescents: the Strong Heart Study. J Am Coll Cardiol. 2006;47:2267–73.
Dhuper S, Abdullah RA, Weichbrod L, Mahdi E, Cohen HW. Association of obesity and hypertension with left ventricular geometry and function in children and adolescents. Obesity. 2011;19:128–33.
Dusan P, Tamara I, Goran V, Gordana ML, Amira PA. Left ventricular mass and diastolic function in obese children and adolescents. Pediatr Nephrol. 2015;30:645–52.
Porcar-Almela M, Codoner-Franch P, Tuzon M, Navarro-Solera M, Carrasco-Luna J, Ferrando J. Left ventricular diastolic function and cardiometabolic factors in obese normotensive children. Nutr Metab Cardiovasc Dis. 2015;25:108–15.
Brady TM. The role of obesity in the development of left ventricular hypertrophy among children and adolescents. Curr Hypertens Rep. 2016;18:3.
Rowland TW. Effect of obesity on cardiac function in children and adolescents: a review. J Sports Sci Med. 2007;6:319–26.
Dias KA, Spence AL, Sarma S, Oxborough D, Timilsina AS, Davies PSW, et al. Left ventricular morphology and function in adolescents: relations to fitness and fatness. Int J Cardiol. 2017;240:313–9.
Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350:2362–74.
Van Putte-Katier N, Rooman RP, Haas L, Verhulst SL, Desager KN, Ramet J, et al. Early cardiac abnormalities in obese children: importance of obesity per se versus associated cardiovascular risk factors. Pediatr Res. 2008;64:205–9.
Fuentes L, Brown AL, Mathews SJ, Waggoner AD, Soto PF, Gropler RJ, et al. Metabolic syndrome is associated with abnormal left ventricular diastolic function independent of left ventricular mass. Eur Heart J. 2007;28:553–9.
Shah AS, Dolan LM, Khoury PR, Gao Z, Kimball TR, Urbina EM. Severe obesity in adolescents and young adults is associated with subclinical cardiac and vascular changes. J Clin Endocrinol Metab. 2015;100:2751–7.
Drinkard B, Roberts MD, Ranzenhofer LM, Han JC, Yanoff LB, Merke DP, et al. Oxygen-uptake efficiency slope as a determinant of fitness in overweight adolescents. Med Sci Sports Exerc. 2007;39:1811–6.
Hansen D, Marinus N, Remans M, Courtois I, Cools F, Calsius J, et al. Exercise tolerance in obese vs. lean adolescents: a systematic review and meta-analysis. Obes Rev. 2014;15:894–904.
Jouven X, Empana JP, Schwartz PJ, Desnos M, Courbon D, Ducimetiere P. Heart-rate profile during exercise as a predictor of sudden death. N Engl J Med. 2005;352:1951–8.
Norman AC, Drinkard B, McDuffie JR, Ghorbani S, Yanoff LB, Yanovski JA. Influence of excess adiposity on exercise fitness and performance in overweight children and adolescents. Pediatrics. 2005;115:e690–6.
Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7:284–94.
McCarthy HD, Cole TJ, Fry T, Jebb SA, Prentice AM. Body fat reference curves for children. Int J Obes. 2006;30:598–602.
Slaughter MH, Lohman TG, Boileau RA, Horswill CA, Stillman RJ, Van Loan MD, et al. Skinfold equations for estimation of body fatness in children and youth. Hum Biol. 1988;60:709–23.
Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44:291–303.
Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970;45:13–23.
Bervoets L, Van Noten C, Van Roosbroeck S, Hansen D, Van Hoorenbeeck K, Verheyen E, et al. Reliability and validity of the Dutch Physical Activity Questionnaires for Children (PAQ-C) and Adolescents (PAQ-A). Arch Public health = Arch Belg De Sante Publique. 2014;72:47.
Matthews D, Hosker J, Rudenski A, Naylor B, Treacher D, Turner R. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Martinez-Vizcaino V, Martinez MS, Aguilar FS, Martinez SS, Gutierrez RF, Lopez MS, et al. Validity of a single-factor model underlying the metabolic syndrome in children: a confirmatory factor analysis. Diabetes Care. 2010;33:1370–2.
Andersen OS, Smiseth OA, Dokainish H, Abudiab MM, Schutt RC, Kumar A, et al. Estimating left ventricular filling pressure by echocardiography. J Am Coll Cardiol. 2017;69:1937–48.
Bongers BC, Hulzebos EH, Helbing WA, Ten Harkel A, van Brussel M, Takken T. Response profiles of oxygen uptake efficiency during exercise in healthy children. Eur J Prev Cardiol. 2016;23:865–73.
Lamb KL, Eston RG, Corns D. Reliability of ratings of perceived exertion during progressive treadmill exercise. Br J Sports Med. 1999;33:336–9.
Imai K, Sato H, Hori M, Kusuoka H, Ozaki H, Yokoyama H, et al. Vagally mediated heart rate recovery after exercise is accelerated in athletes but blunted in patients with chronic heart failure. J Am Coll Cardiol. 1994;24:1529–35.
Okutucu S, Karakulak UN, Aytemir K, Oto A. Heart rate recovery: a practical clinical indicator of abnormal cardiac autonomic function. Expert Rev Cardiovasc Ther. 2011;9:1417–30.
Wasserman K, Stringer WW, Casaburi R, Koike A, Cooper CB. Determination of the anaerobic threshold by gas exchange: biochemical considerations, methodology and physiological effects. Z Kardiol. 1994;83(Suppl 3):1–12.
Beaver WL, Wasserman K, Whipp BJ. A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol. 1986;60:2020–7.
Marinus N, Bervoets L, Massa G, Verboven K, Stevens A, Takken T, et al. Altered gas-exchange at peak exercise in obese adolescents: implications for verification of effort during cardiopulmonary exercise testing. J Sports Med Phys Fit. 2017;57:1687–94.
Peterson LR, Waggoner AD, Schechtman KB, Meyer T, Gropler RJ, Barzilai B, et al. Alterations in left ventricular structure and function in young healthy obese women: assessment by echocardiography and tissue Doppler imaging. J Am Coll Cardiol. 2004;43:1399–404.
de Simone G, Izzo R, De Luca N, Gerdts E. Left ventricular geometry in obesity: is it what we expect? Nutr Metab Cardiovasc Dis. 2013;23:905–12.
Azevedo A, Bettencourt P, Almeida PB, Santos AC, Abreu-Lima C, Hense HW, et al. Increasing number of components of the metabolic syndrome and cardiac structural and functional abnormalities--cross-sectional study of the general population. BMC Cardiovasc Disord. 2007;7:17.
Atabek ME, Akyuz E, Selver Eklioglu B, Cimen D. The relationship between metabolic syndrome and left ventricular mass index in obese children. J Clin Res Pediatr Endocrinol. 2011;3:132–8.
Sung JK, Kim JY. Obesity and preclinical changes of cardiac geometry and function. Korean Circ J. 2010;40:55–61.
Urbina EM, Gidding SS, Bao W, Elkasabany A, Berenson GS. Association of fasting blood sugar level, insulin level, and obesity with left ventricular mass in healthy children and adolescents: the Bogalusa Heart Study. Am Heart J. 1999;138(1 Pt 1):122–7.
Pires KM, Buffolo M, Schaaf C, David Symons J, Cox J, Abel ED, et al. Activation of IGF-1 receptors and Akt signaling by systemic hyperinsulinemia contributes to cardiac hypertrophy but does not regulate cardiac autophagy in obese diabetic mice. J Mol Cell Cardiol. 2017;113:39–50.
Sasson Z, Rasooly Y, Bhesania T, Rasooly I. Insulin resistance is an important determinant of left ventricular mass in the obese. Circulation. 1993;88(4 Pt 1):1431–6.
Chakko S, Mayor M, Allison MD, Kessler KM, Materson BJ, Myerburg RJ. Abnormal left ventricular diastolic filling in eccentric left ventricular hypertrophy of obesity. Am J Cardiol. 1991;68:95–8.
Fischer M, Baessler A, Hense HW, Hengstenberg C, Muscholl M, Holmer S, et al. Prevalence of left ventricular diastolic dysfunction in the community. Results from a Doppler echocardiographic-based survey of a population sample. Eur Heart J. 2003;24:320–8.
Alpert MA, Omran J, Bostick BP. Effects of obesity on cardiovascular hemodynamics, cardiac morphology, and ventricular function. Curr Obes Rep. 2016;5:424–34.
Mizushige K, Yao L, Noma T, Kiyomoto H, Yu Y, Hosomi N, et al. Alteration in left ventricular diastolic filling and accumulation of myocardial collagen at insulin-resistant prediabetic stage of a type II diabetic rat model. Circulation. 2000;101:899–907.
Goldstein RH, Poliks CF, Pilch PF, Smith BD, Fine A. Stimulation of collagen formation by insulin and insulin-like growth factor I in cultures of human lung fibroblasts. Endocrinology. 1989;124:964–70.
Ceriello A, Taboga C, Tonutti L, Quagliaro L, Piconi L, Bais B, et al. Evidence for an independent and cumulative effect of postprandial hypertriglyceridemia and hyperglycemia on endothelial dysfunction and oxidative stress generation: effects of short- and long-term simvastatin treatment. Circulation. 2002;106:1211–8.
Aroor AR, Mandavia CH, Sowers JR. Insulin resistance and heart failure: molecular mechanisms. Heart Fail Clin. 2012;8:609–17.
Wu CK, Yang CY, Lin JW, Hsieh HJ, Chiu FC, Chen JJ, et al. The relationship among central obesity, systemic inflammation, and left ventricular diastolic dysfunction as determined by structural equation modeling. Obesity. 2012;20:730–7.
Prabhu SD. Cytokine-induced modulation of cardiac function. Circ Res. 2004;95:1140–53.
Iliesiu A, Campeanu A, Dusceac D. Serum uric acid and cardiovascular disease. Maedica. 2010;5:186.
Jia G, Habibi J, Bostick BP, Ma L, DeMarco VG, Aroor AR, et al. Uric acid promotes left ventricular diastolic dysfunction in mice fed a Western diet. Hypertension. 2015;65:531–9.
Gondoni LA, Titon AM, Nibbio F, Augello G, Caetani G, Liuzzi A. Heart rate behavior during an exercise stress test in obese patients. Nutr Metab Cardiovasc Dis. 2009;19:170–6.
Laguna M, Aznar S, Lara MT, Lucia A, Ruiz JR. Heart rate recovery is associated with obesity traits and related cardiometabolic risk factors in children and adolescents. Nutr Metab Cardiovasc Dis. 2013;23:995–1001.
Kizilbash MA, Carnethon MR, Chan C, Jacobs DR, Sidney S, Liu K. The temporal relationship between heart rate recovery immediately after exercise and the metabolic syndrome: the CARDIA study. Eur Heart J. 2006;27:1592–6.
Freeman JV, Dewey FE, Hadley DM, Myers J, Froelicher VF. Autonomic nervous system interaction with the cardiovascular system during exercise. Prog Cardiovasc Dis. 2006;48:342–62.
Acknowledgements
We would like to thank all adolescents for their participation and guidance of their parents during this study. Furthermore, we thank the clinicians from the Department of Pediatrics at the Jessa hospital for all the support in this study.
Author contributions
P.D., G.M., and D.H. conceived and designed the study design. W.M.A.F., M.B., and G.M. included the participants. W.M.A.F. and M.B. performed the measurements. T.A.H. performed the echocardiographic measurements and analyzed the echocardiographic data. W.M.A.F., M.B., D.H., and G.M. analyzed the data. W.M.A.F. and M.B. performed the statistical analysis. W.M.A.F., D.H., and G.M. wrote the manuscript. T.A.H., I.F., P.D., K.V., and B.O.E. critically reviewed the manuscript. All authors gave their final approval of the manuscript to be submitted.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Supplementary information
Rights and permissions
About this article
Cite this article
Franssen, W.M.A., Beyens, M., Hatawe, T.A. et al. Cardiac function in adolescents with obesity: cardiometabolic risk factors and impact on physical fitness. Int J Obes 43, 1400–1410 (2019). https://doi.org/10.1038/s41366-018-0292-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0292-x
This article is cited by
-
Influence of physical fitness and weight status on autonomic cardiac modulation in children
Pediatric Research (2023)
-
Cardiac diastolic function and heart rate recovery in obese adolescents: chronotropic response and statistical perspectives
International Journal of Obesity (2019)
-
Response to letter from Okutucu and Bursa
International Journal of Obesity (2019)