Abstract
Objective:
Small-for-gestational-age (SGA) neonates, infants of diabetic mothers (IDM) and very-low-birth weight premature neonates (VLBW) are reported to have increased risk for developing iron deficiency and possibly associated neurocognitive delays.
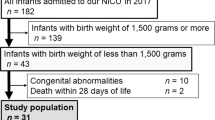
Study Design:
We conducted a pilot study to assess iron status at birth in at-risk neonates by measuring iron parameters in umbilical cord blood from SGA, IDM, VLBW and comparison neonates.
Results:
Six of the 50 infants studied had biochemical evidence of iron deficiency at birth. Laboratory findings consistent with iron deficiency were found in one SGA, one IDM, three VLBW, and one comparison infant. None of the infants had evidence of iron deficiency anemia.
Conclusions:
Evidence of biochemical iron deficiency at birth was found in 17% of screened neonates. Studies are needed to determine whether these infants are at risk for developing iron-limited erythropoiesis, iron deficiency anemia or iron-deficient neurocognitive delay.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Callahan LS, Thibert KA, Wobken JD, Georgieff MK . Early-life iron deficiency anemia alters the development and long-term expression of parvalbumin and perineuronal nets in the rat hippocampus. Dev Neurosci 2013; 35: 427–436.
Tran PV, Dakoji S, Reise KH, Storey KK, Georgieff MK . Fetal iron deficiency alters the proteome of adult rat hippocampal synaptosomes. Am J Physiol Regul Integr Comp Physiol 2013; 305: R1297–R1306.
Fretham SJ, Carlson ES, Georgieff MK . The role of iron in learning and memory. Adv Nutr 2011; 2: 112–121.
Radlowski EC, Johnson RW . Perinatal iron deficiency and neurocognitive development. Front Hum Neurosci 2013; 7: 1–10.
Zamora TG, Guiang SF 3rd, Widness JA, Georgieff MK . Iron is prioritized to red blood cells over the brain in phlebotomized anemic newborn lambs. Pediatr Res 2016; 79: 922–928.
Mukhopadhyay K, Yadav RK, Kishore SS, Garewal G, Jain V, Narang A . Iron status at birth and at 4 weeks in term small-for-gestation infants in comparison with appropriate-for-gestation infants. J Matern Fetal Neonatal Med 2011; 7: 886–890.
Rao R, Georgieff MK . Iron therapy for preterm infants. Clin Perinatol 2009; 36: 27–42.
Hokama T, Takenaka S, Hirayama K, Yara A, Yoshida K, Itokazu K et al. Iron status of newborns born to iron deficient anaemic mothers. J Trop Pediatr 1996; 42: 75–77.
Emamghorashi F, Heidari T . Iron status of babies born to iron-deficient anaemic mothers in an Iranian hospital. East Mediterr Health J 2004; 10: 808–814.
Gambling L, Lang C, McArdle HJ . Fetal regulation of iron transport during pregnancy. Am J Clin Nutr 2011; 94: 1903 S–1907 S.
McArdle HJ, Lang C, Hayes H, Gambling L . Role of the placenta in regulation of fetal iron status. Nutr Rev 2011; 69: S17–S22.
Balesaria S, Hanif R, Salama MF, Raja K, Bayele HK, McArdle H et al. Fetal iron levels are regulated by maternal and fetal Hfe genotype and dietary iron. Haematologica 2012; 97: 661–669.
Cao C, Fleming MD . The placenta: the forgotten essential organ of iron transport. Nutr Rev 2016; 74: 421–431.
. Goodnough LT, Nemeth E. Clinical features of iron deficiency. In: Greer JP, Arber DA, Glader B, List AF, Means Jr. RT, Paraskevas F et al. (eds). Wintrobe’s Clinical Hematology. 13th edn. Lippincott/Williams & Wilkins: Philadelphia, PA, USA. 2014. pp 626–627..
Christensen RD, Henry E, Bennett ST, Yaish HM . Reference intervals for reticulocyte parameters of infants during their first 90 days after birth. J Perinatol 2016; 36: 61–66.
Lorenz L, Arand J, Büchner K, Wacker-Gussmann A, Peter A, Poets CF et al. Reticulocyte haemoglobin content as a marker of iron deficiency. Arch Dis Child Fetal Neonatal Ed 2015; 100: F198–F202.
Lopez A, Cacoub P, Macdougall IC, Peyrin-Biroulet L . Iron deficiency anaemia. Lancet 2016; 387: 907–916.
Baer VL, Lambert DK, Carroll PD, Gerday E, Christensen RD . Using umbilical cord blood for the initial blood tests of VLBW neonates results in higher hemoglobin and fewer RBC transfusions. J Perinatol 2013; 33: 363–365.
Jopling J, Henry E, Wiedmeier SE, Christensen RD . Reference ranges for hematocrit and blood hemoglobin concentration during the neonatal period: data from a multihospital health care system. Pediatrics 2009; 123: e333–e337.
Christensen RD, Jopling J, Henry E, Wiedmeier SE . The erythrocyte indices of neonates, defined using data from over 12,000 patients in a multihospital health care system. J Perinatol 2008; 28: 24–28.
McArdle HJ, Gambling L, Kennedy C . Iron deficiency during pregnancy: the consequences for placental function and fetal outcome. Proc Nutr Soc 2014; 73: 9-1.5.
O'Brien KO, Zavaleta N, Abrams SA, Caulfield LE . Maternal iron status influences iron transfer to the fetus during the third trimester of pregnancy. Am J Clin Nutr 2003; 77: 924–930.
Sweet DG, Savage GA, Tubman R, Lappin TR, Halliday HL . Cord blood transferrin receptors to assess fetal iron status. Arch Dis Child Fetal Neonatal Ed 2001; 85: F46–F68.
Lozoff B, Beard J, Connor J, Felt B, Georgieff M, Schallert T . Lost-lasting neural and behavioral effects of iron deficiency in infancy. Nutr Rev 2006; 64: S34–S91.
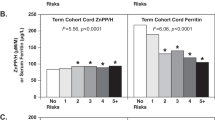
Cheng CF, Zerzan JC, Johnson DB, Juul SE . Zinc protoporphyrin-to-heme ratios in high-risk and preterm infants. J Pediatr 2012; 161: 81–87.
Lott DG, Zimmerman M, Labbe RF, Kling PJ, Widness JA . Erythrocyte zinc protoporphyrin is elevated with prematurity and fetal hypoxemia. Pediatrics 2005; 116: 414–422.
Ward DM, Kaplan J . Ferroportin-mediated iron transport: expression and regulation. Biochim Biophys Acta 2012; 1823: 1426–1433.
Kroot JJ, Tjalsma H, Fleming RE, Swinkels DW . Hepcidin in human iron disorders: diagnostic implications. Clin Chem 2011; 57: 1650–1669.
Lorenz L, Peter A, Poets CF, Franz AR . A review of cord blood concentrations of iron status parameters to define reference ranges for preterm infants. Neonatology 2013; 104: 194–202.
Rehu M, Punnonon K, Ostland V, Heinonen S, Westerman M, Pulkki K et al. Maternal serum hepcidin is low at term and independent of cord blood iron status. Eur J Haematol 2010; 85: 345–352.
McCarthy PJ, Zundel HR, Johnson KR, Blohowiak SE, Kling PJ . Impact of growth restriction and other prenatal risk factors on cord blood iron status in prematurity. J Pediatr Hematol Oncol 2016; 38: 210–215.
Akkermans MD, Uijterschout L, Abbink M, Vos P, Rovekamp-Abels L, Boersma B et al. Predictive factors of iron depletion in late preterm infants at the postnatal age of 6 weeks. Eur J Clin Nutr 2016; 70: 941–946.
Siddappa AM, Rao R, Long JD, Widness JA, Georgieff MK . The assessment of newborn iron stores at birth: a review of the literature and standards for ferritin concentrations. Neonatology 2007; 92: 73–82.
Lorenz L, Herbst J, Engel C, Peter A, Abele H, Poets CF et al. Gestational age-specific reference ranges of hepcidin in cord blood. Neonatology 2014; 106: 133–139.
Miller SM, McPherson RJ, Juul SE . Iron sulfate supplementation decreases zinc protoporphyrin to heme ratio in premature infants. J Pediatr 2006; 148: 44–48.
Sweet DG, Savage G, Tubman TR, Lappin TR, Halliday HL . Study of maternal influences on fetal iron status at term using cord blood transferrin receptors. Arch Dis Child Fetal Neonatal Ed 2001; 84: F40–F43.
American Academy of Pediatrics, Committee on NutritionNutritional needs of the preterm infant In: Kleinman RD (ed). Pediatric Nutrition Handbook vol. 5. American Academy of Pediatrics: Chapel Hill, NC, USA, 2004, pp 23–54.
Acknowledgements
We thank the Metabolics Core from the University of Utah for assistance with mass spectrometry (DK110858). Funding was provided by the Division of Neonatology, University of Utah, ARUP Laboratories, Salt Lake City, UT, and Intermountain Healthcare, Salt Lake City, UT. This work was supported in part by the US National Institutes of Health (DK030534 to Diane Ward).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
MacQueen, B., Christensen, R., Ward, D. et al. The iron status at birth of neonates with risk factors for developing iron deficiency: a pilot study. J Perinatol 37, 436–440 (2017). https://doi.org/10.1038/jp.2016.234
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.234
This article is cited by
-
Serum ferritin values in neonates <29 weeks’ gestation are highly variable and do not correlate with reticulocyte hemoglobin content
Journal of Perinatology (2023)
-
Impact and interactions between risk factors on the iron status of at-risk neonates
Journal of Perinatology (2022)
-
Maternal obesity and impaired offspring neurodevelopment: could fetal iron deficiency be a pathogenic link?
Journal of Perinatology (2021)
-
Urinary ferritin; a potential noninvasive way to screen NICU patients for iron deficiency
Journal of Perinatology (2021)
-
Reconciling markedly discordant values of serum ferritin versus reticulocyte hemoglobin content
Journal of Perinatology (2021)