Abstract
Studies fail to find uniform effects of age-related or induced hypogonadism on human sexual function. We examined the effects of induced hypogonadism on sexual function in healthy men and women and attempted to identify predictors of the sexual response to induced hypogonadism or hormone addback. The study design used was a double-blind, controlled, crossover (self-as-own control). The study setting was an ambulatory care clinic in a research hospital, and the participants were 20 men (average±SD age=28.5±6.2 years) and 20 women (average±SD age=33.5±8.7 years), all healthy and with no history of psychiatric illness. A multidimensional scale assessing several domains of sexual function was the main outcome measure. Participants of the study received depot leuprolide acetate (Lupron) every 4 weeks for 3 months (men) or 5 months (women). After the first month of Lupron alone, men received (in addition to Lupron) testosterone enanthate (200 mg intramuscularly) or placebo every 2 weeks for 1 month each. Women received Lupron alone for 2 months, and then, in addition to Lupron, they received estradiol and progesterone for 5 weeks each. The results of the study: in women, hypogonadism resulted in a significant decrease in global measures of sexual functioning, principally reflecting a significant decrease in the reported quality of orgasm. In men, hypogonadism resulted in significant reductions in all measured domains of sexual function. Testosterone restored sexual functioning scores in men to those seen at baseline, whereas neither estradiol nor progesterone significantly improved the reduced sexual functioning associated with hypogonadism in women. Induced hypogonadism decreased sexual function in a similar number of men and women. No predictors of response were identified except for levels of sexual function at baseline. In conclusion, our data do not support a simple deficiency model for the role of gonadal steroids in human sexual function; moreover, while variable, the role of testosterone in sexual function in men is more apparent than that of estradiol or progesterone in women.
Similar content being viewed by others
INTRODUCTION
Studies of the effects of hypogonadism on sexual functioning in women have been confounded by the conditions under which hypogonadism occurs, including aging, surgical procedures, and coexisting gynecologic pathologies. In young men, decreased sexual functioning secondary to hypogonadism is more consistently demonstrated (Bagatell et al, 1994); however, the reductions are not uniformly observed, and predictors of the sexual response to hypogonadism or androgen replacement have not been identified. While imperfect in modeling natural conditions, hormone manipulation paradigms can eliminate many of the confounds that obscure the relationship between hormones and sexual function. In this study, we take advantage of two studies of the effects of induced hypogonadism on mood in young, healthy men and women, and ask whether similar hormonal manipulations alter sexual function.
A role for sex steroids in the regulation of sexual function in men and women has been inferred from several observations. First, therapeutic trials, many of which were placebo-controlled, reported the beneficial effects of sex hormone therapy in men and women in whom hypogonadism was secondary to medical or surgical castration (Floter et al, 2002; Shifren et al, 1985, 2000; Simon et al, 2005; Sherwin et al, 1985; Sherwin and Gelfand, 1987; Braunstein et al, 2005; O’Carroll et al, 1985; Anderson et al, 1999; Bhasin, 2000; Bagatell et al, 1994; Dennerstein et al, 1980; Davidson et al, 1979), reproductive senescence (Nathorst-Boos et al, 1993b, 2006; Sarrel, 1990, 1998; Wiklund et al, 1993; Myers et al, 1990; Sarrel et al, 1998; Lobo et al, 2003; Sherwin, 1991; Wang et al, 2000; Gray et al, 2005; Steidle et al, 2003; Seftel et al, 2004; Guay et al, 1995), or concurrent medical conditions (eg Kallman's syndrome or HIV) (Wang et al, 2000; O’Carroll et al, 1985; Snyder et al, 2000; Anderson et al, 1999; Arlt et al, 1999; Rabkin et al, 2000, 2006; Johannsson et al, 2002; Carani et al, 2005). These data suggest (albeit indirectly) that deficiencies of sex hormones could underlie a decrease in sexual function in both men and women. Second, some basal hormone studies have observed correlations between blood levels of sex steroids and sexual functioning, while other studies have observed lower sex hormone levels in subjects with decreased sexual function compared with asymptomatic control groups (Schiavi et al, 1991; Cawood and Bancroft, 1996; Santoro et al, 2005; Basar et al, 2005; Modelska et al, 2004; Travison et al, 2006; Beutel et al, 2005; Kennedy et al, 1997; Nyunt et al, 2005; Dennerstein et al, 1994, 2002; Slob et al, 1996; Adams et al, 1978; Bancroft et al, 1980; Meuwissen and Over, 1992; Doering et al, 1974). Finally, several longitudinal studies have demonstrated the reduction of sexual function under the following circumstances: after medical or surgical castration; after the development of hypogonadism secondary to a variety of medical illnesses; after the administration of medications that inhibit sex hormone production (Marberger et al, 2006); and during age-related reproductive senescence (Dennerstein et al, 2002; Koster and Garde, 1993).
Despite these findings, the role of gonadal steroids in the regulation of sexual function in humans remains controversial for several reasons. First, the results of therapeutic trials are difficult to interpret since hormone therapy may have effects independent of those on sexual function. For example, mood, energy, muscle mass, and strength improve with androgen therapy and might, therefore, contribute indirectly to the observed beneficial effects of androgens on sexual functioning (Grinspoon et al, 2000). Second, the results of basal hormone studies are inconsistent, since men and women with low sex hormone levels do not uniformly report low levels of sexual function (Travison et al, 2006; Santoro et al, 1996; Burger et al, 1995, 1999, 2000; Leiblum et al, 2006; Sternbach, 1998; Bachmann et al, 1985; Greendale et al, 1996; Davidson et al, 1983; Vermeulen, 2001). Finally, a substantial proportion of both men and women (30–50%) report no change in libido after medical or surgical castration despite obvious losses of reproductive endocrine function (Bagatell et al, 1994; Bremer, 1959; Dennerstein et al, 1977, 2002; Chakravarti et al, 1977; Tauber, 1940; Elit et al, 2001; Madalinska et al, 2005; Zussman et al, 1981).
Several characteristics could influence the impact of declining or suppressed gonadal steroid secretion on sexual functioning, including the magnitude of the decrease in sex hormone levels from baseline, the level of hormone during hypogonadism (ie below a threshold of hormone levels at which impaired sexual function occurs), sex, age, duration of hypogonadism, and baseline phenotype (eg level of sexual function), as well as the presence of concurrent symptoms such as depression (Isidori et al, 2005; Beutel et al, 2005; Cawood and Bancroft, 1996; Nilsson et al, 1995; Kratzik et al, 2004; Finkelstein et al, 1998; Schiavi and White, 1976; Schiavi et al, 1994). Indeed, in a preliminary study using an undimensional evaluation of libido, we observed that baseline levels of sexual functioning predicted the response to hypogonadism and hormone replacement in a group of men with GnRH agonist-induced hypogonadism (Schmidt et al, 2004). These observations are important clinically as they could predict those individuals in whom hormone therapy would improve sexual function.
In this study, we attempted to examine the role of gonadal steroids in human sexual functioning as follows: first, we assessed the impact of the acute short-term induction of hypogonadism on sexual functioning. Second, we evaluated potential sex differences in the response to induced hypogonadism. Finally, we examined the impact of several other variables that might predict a differential response to hypogonadism or hormone therapy in humans, including age, mood symptoms, and hormone levels. Our main hypothesis was that induced hypogonadism would impair sexual functioning across multiple domains in groups of men and women. A secondary hypothesis was that considerable variability would be demonstrated in the impact of hypogonadism on sexual functioning in men and women (Wallen, 1990, 2001; Herzog et al, 2005; Zehr et al, 1998).
METHODS
Subject Selection
Men (between age 18 and 45 years) and women (between age 18 and 55 years) were recruited through advertisements in local newspapers or referred from the NIH Normal Volunteer Office, and participated between November 1994 and March 2003. All were participants in a larger study examining the effects of GnRH agonist-induced hypogonadism and sex hormone replacement on measures of mood and brain function. Given the original focus of this study, in women we evaluated the effects of the two principal ovarian steroids, estradiol and progesterone, whereas the effects of testosterone were evaluated in men only. Estradiol, testosterone, and progesterone (or its neurosteroid metabolites) all have been implicated in the regulation of appetitive behaviors including sexual motivation in both animals and humans (Frye, 2007; Evans and Foltin, 2006; Dreher et al, 2007). All participants were medication free and free of significant medical illness (current or in the past 2 years) confirmed by history, physical examination, and routine laboratory tests.
None of the men and women reported problems with their mood, sleep, sexual function, or sexual relationships. Women reported regular menstrual cycle function (21–35 days). The absence of current or past psychiatric illness was confirmed by a structured psychiatric diagnostic interview (Spitzer et al, 1990). Additionally, all subjects completed daily visual analog scale self-ratings (sadness, anxiety, and irritability) for at least 2 months to exclude the presence of premenstrual mood symptoms in women or other mood disturbances.
The protocol was approved by the National Institute of Mental Health Intramural Research Board, and written informed consent was obtained from all subjects. Subjects were paid for their participation in this protocol according to the guidelines of the NIH Normal Volunteer Office.
Procedure
Hormonal manipulation protocol
All women received 3.75 mg of depot Lupron (leuprolide acetate, purchased from TAP Pharmaceuticals, Chicago, IL) by intramuscular injection every 4 weeks for 5 months (Figure 1). Lupron alone was administered for the first 8 weeks. All women then received, in addition to Lupron, 17 β estradiol (0.1 mg/day) (E) by skin patch (Alora, active and placebo patches were supplied by Watson Pharmaceuticals, Salt Lake City, UT) or progesterone suppositories (200 mg b.i.d.) (P) (NIH Pharmacy, Bethesda, MD) for 5 weeks each. The two replacement regimens were separated by a 2-week washout period.
All women received 3.75 mg of depot Lupron (leuprolide acetate; TAP Pharmaceuticals, Chicago, IL) by intramuscular injection every 4 weeks for 5 months. The first injection of Lupron was administered during the follicular phase between days 2–6 after the onset of menses. Lupron alone was administered for the first 8 weeks. All women then received, in addition to Lupron, 17 β estradiol (0.1 mg/day) (E) by skin patch (Alora; Watson Pharmaceuticals, Salt Lake City, UT) or progesterone suppositories (200 mg b.i.d.) (P) (NIH Pharmacy, Bethesda, MD) for 5 weeks each. The two replacement regimens were separated by a 2-week washout period. Subjects were administered both patches and suppositories (active or placebo, depending upon the treatment phase) daily throughout the entire replacement period to ensure that the double blind was maintained. During the last week of E, all women received 1 week of active P suppositories in addition to E to precipitate menses. All women received prepackaged 1-week unit-dose supplies of suppositories that were formulated and coded (weeks 1–5) by the NIH Pharmacy Department. All men received 7.5 mg of depot Lupron by intramuscular injection every 4 weeks for 3 months. Lupron alone was administered for the first 4 weeks. Subjects then received, in addition to Lupron, testosterone enanthate (200 mg) or placebo (1 ml sesame oil) given by intramuscular injection every 2 weeks for 1 month. All men received 1 month each of testosterone replacement (T) and placebo. A placebo comparison was included in men to blind the timing of the addition of testosterone, whereas in women no placebo phase was included since the order of estradiol and progesterone addback was randomly assigned. In both men and women the order of receiving hormone replacement (ie, T vs placebo in men, and E vs P in women) was randomly assigned and counter-balanced.
All men received 7.5 mg of depot Lupron by intramuscular injection every 4 weeks for 3 months. Lupron alone was administered for the first 4 weeks. Subjects then received, in addition to Lupron, testosterone enanthate (200 mg) (T) or placebo (1 ml sesame oil) given by intramuscular injection every 2 weeks for 1 month. A placebo comparison was included in men to blind the timing of the addition of testosterone, whereas in women no placebo phase was included since the order of estradiol and progesterone addback was randomly assigned.
In both men and women, the order of receiving hormone replacement (ie, T vs placebo in men, and E vs P in women) was randomly assigned and counter-balanced.
Subjects were seen at the NIMH clinic at least every 2 weeks throughout the study, and blood samples were obtained and symptom rating scales were completed. Both subjects and raters (NH, PJS) were blinded to the order of replacement. Blood samples were employed solely to confirm hormone levels during each of the pharmacologically induced hormone conditions (see Table 2). Individuals came into the clinic at approximately the same time during the study, although the time of the day for each visit varied across individuals. Blood samples were centrifuged, aliquoted, and stored at −70°C until time of assay.
Outcome Measures
Sexual functioning was evaluated by a uniquely modified version of the Derogatis Interview of Sexual Functioning-Self Report (DISF-SR) (Derogatis, 1997), a multidimensional scale with separate forms designed for men and women. The DISF-SR scale was selected for this study because it sampled several domains of sexual function. Additionally, in contrast to the majority of other measures of sexual function, the DISF-SR was available in forms adapted for both men and women and, therefore, potential sex differences could be evaluated. Finally, the reliability and validity of DISF-SR (and other scales measuring sexual function) have been determined by comparing scores between symptomatic and asymptomatic samples; however, this study employed a repeated measure, self-as-own design; consequently, the capability of the scale to distinguish normal from abnormal sexual function was less of a concern. Questions focus on five domains (ie, subscales) of sexual functioning: (1) sexual cognition and fantasy (eg erotic thoughts and dreams), (2) sexual arousal (eg level of arousal during sexual behaviors), (3) sexual behavior and experience (eg masturbation, foreplay, and intercourse), (4) quality of orgasm, and (5) sexual drive and relationship (eg level of satisfaction with sexual relationships). We requested and were given permission to modify the DISF-SR specifically for this study by the author and copyright holder, Leonard R Derogatis, PhD. Such permission used by the authors (PJS, DRR) should in no way be construed as an endorsement of this approach to measurement. The DISF was modified from the original for this study as follows. First, the sampling interval within which sexual function is measured was reduced from a 30-day to a 7-day interval. Second, the scale was converted from a nine-point Likert-type scale (0–8) to a 100 mm visual analog scale (0–100) (range—not at all to very frequently). Finally, a seventh question was introduced in section IV (quality of orgasm) of the male version to examine feelings of closeness and togetherness with partner, an item that was present in the female scale and also relevant to male sexual function. The modified scale has both a total score and individual domain scores (subscale) as follows: maximum total scores of 2500 in women and 2600 in men, maximum scores for each domain of 500, except for quality of orgasm (no. 4—score of 600 in women and 700 in men), and sexual drive (no. 5—score of 400 in both men and women) (Figure 2).
In men, a significant interaction between baseline symptom group (high vs low) and hormone condition was identified by ANOVA-R (F2,20=9.7, p<0.003). Men with high baseline DISF scores (n=6) had a significant reduction in total DISF scores during hypogonadism compared with both baseline and T-replaced conditions, and a significant increase in DISF scores after T replacement compared with hypogonadism. Men with low baseline DISF scores (n=6) showed no significant differences in DISF scores across hormone conditions. Similarly, women with high baseline DISF scores (n=6) showed a significant reduction in DISF scores during hypogonadism (and during estrogen and progesterone conditions) compared with baseline scores, whereas women with low baseline DISF scores (n=6) showed no significant change across hormone conditions (ANOVA-R group × hormone condition, F3,30=9.8, p=0.001). In women, total DISF scores were significantly greater in the ‘high’ group at baseline only (t40=3.8, p<0.01; otherwise p=NS). Whereas, in men, total DISF scores were significantly higher in the ‘high’ compared to the ‘low’ baseline symptom group during both baseline and T (t30=3.4 and 4.7, respectively, p<0.01). No significant interactions between subscale scores and group or hormone condition were observed in either men or women.
The modified version maintained the same five domains as the original, and except for one question (mentioned above), the remaining 25 questions were the same (in both female and male interviews). The DISF was administered at baseline (start date of Lupron) in both men and women. In men, the DISF also was administered during the last weeks of placebo and T replacement; whereas in women, the DISF was administered at the end of Lupron alone (hypogonadism) and during the last week of each hormone replacement condition (E and P). Symptom rating data during the first month were not included in the analysis since steroid levels increase (or ‘flare’) transiently after the first injection of Lupron. Additionally, to evaluate coexisting mood symptoms all participants completed the Beck Depression Inventory (BDI) (Beck et al, 1961) at the same time that the DISF was completed.
Statistical Analysis
In both women and men, serum hormone levels, BDI, and total DISF scores at each time point were compared by analysis of variance with repeated measures (ANOVA-R; Systat, SPSS, Chicago, IL), with hormone condition (women [four levels]: baseline, hypogonadal, E, and P; men [three levels]: baseline, hypogonadal, and T) as the within-subjects variable. Additionally, in both men and women we examined the effects of hormone condition on individual domains of sexual functioning by performing separate ANOVA-Rs on each of the DISF subscales (ie nos. 1–5).
To examine possible sex differences in response to hypogonadism, Z-scores were calculated for baseline and hypogonadal DISF scores (ie, total and individual subscale scores) in the women and compared with those in men by ANOVA-R with sex as the between-subjects variable and hormone condition (baseline and hypogonadal) as the within-subjects variable. Z-scores were calculated using the average and standard deviations of the baseline DISF scores in each sex to permit comparisons across men and women despite differences in total maximum DISF scores. Additionally, we operationally defined a substantial decline in sexual function as a 50% or greater reduction in the total DISF score relative to baseline scores. This criterion was intended to serve as a proxy for a clinically significant decrease in sexual function (Alexander et al, 2004) and was based on a similar threshold employed in pharmacologic studies of depression, in which a 50% improvement in rating scores is considered to be clinically significant. We compared the number of men and women who experienced a 50% or greater reduction (relative to baseline) in their total DISF scores by χ2 analysis. We performed an identical analysis employing a less conservative 30% cutoff score as the threshold.
In a prior report (Schmidt et al, 2004) with a larger sample of men (ie n=31), 20 of whom participated in this study, men who received placebo first and, therefore, were exposed to two consecutive months of hypogonadism reported greater declines in sexual function during hypogonadism than those men receiving T replacement first (ie the first month of Lupron alone was followed by 1 month of T prior to the third month during which they received Lupron plus placebo). Thus, we repeated our analyses of sex differences in DISF scores after hypogonadism with only those men who were exposed to two consecutive months of hypogonadism to match (and control for differences in) the duration of hypogonadism in the women in this study.
In our earlier report, in which we employed a multi-symptom inventory in the male subjects of the current study, we also observed that baseline levels of sexual interest predicted subsequent behavioral response to both hypogonadism and T replacement (Schmidt et al, 2004). To replicate these observations with a more comprehensive measure of sexual function in men and to determine if these observations could be extended to women, we first assigned subjects to one of two categories defined by their baseline DISF total scores and then compared subjects in the lowest (n=6) and highest (n=6) tertile baseline scores. DISF scores (total and subscale) were re-analyzed within each sex by ANOVA-R, with baseline total DISF score (low vs high) as the between-subjects variable and hormonal condition as the within-subjects variable.
Finally, men and women were grouped for comparison as follows: (1) those with a 50% or greater reduction in the total DISF scores during hypogonadism compared with baseline and (2) those with the highest and lowest tertiles of baseline DISF scores (as described above). We examined whether these differences in sexual function were associated with specific characteristics at baseline, during hypogonadism, or that changed between baseline and hypogonadism. Two-tailed Student's t-tests (all t-tests had Bonferroni corrections for the number of comparisons made unless indicated) were performed comparing the following baseline measures: age; blood hormone levels (ie, men: total T, free T, E, and dihydrotestosterone [DHT]; women: total T, E, and P), including measures at baseline, during hypogonadism, and the difference (Δ) between measures at baseline and during hypogonadism; and BDI scores at baseline, during hypogonadism, and the change in BDI scores between baseline and hypogonadism. Pearson correlation coefficients were employed to investigate possible relationships between changes in DISF scores and changes in blood hormone levels.
RESULTS
Subject Characteristics
In total, 20 men ranging in age from 22 to 42 years (mean±SD, 28.5±6.2 years) and 20 women ranging in age from 19 to 47 years (mean±SD, 33.5±8.7 years) participated in the study. All participants were Caucasian except for two African-American women. Eleven men received placebo first and, therefore, were exposed to two consecutive months of hypogonadism as were all 20 women. All subjects were sexually active, and their marital status was as follows: men—single (n=12), married (n=6), and divorced (n=2); women—single (n=13), married (n=5), and divorced (n=2). In women, there were no significant effects of hormone condition on BDI scores (ANOVA-R F3,57=0.5, p=NS), whereas in men a significant effect of hormone condition on BDI scores was observed (ANOVA-R F2,38=3.7, p=0.04), which reflected a small but statistically significant increase in BDI scores during the hypogonadal state (Table 1). This increase in BDI score reflected the influence of two men who developed clinically significant mood symptoms and had BDI scores of 14 and 6, respectively, during hypogonadism (consistent with data in the larger group of subjects reported previously) (Schmidt et al, 2004).
DISF Symptom Ratings
Comparisons across hormone conditions in women and men
In women, induced hypogonadism significantly decreased DISF scores compared with those at baseline (Table 1). DISF scores during hypogonadism did not differ from those during either E or P. All DISF subscale scores also showed a reduction during hypogonadism, E, and P compared with baseline; however, the only decrease that met statistical significance after adjustment for five comparisons (ie, the five subscales) was subscale four (quality of orgasm). As observed with the total DISF scores, the subscale scores during hypogonadism, E, and P did not differ significantly.
In men, total DISF scores during hypogonadism were significantly decreased compared with scores during both baseline and T. All five subscale scores significantly decreased during hypogonadism compared with baseline conditions and during hypogonadism compared with T (see Table 1).
We observed identical patterns of results when we repeated these analyses after excluding those men (n=1) and women (n=5) over 40 years of age.
Comparisons between men and women during baseline and hypogonadism
Standardized total DISF scores (ie, Z-scores) were significantly higher in men compared with women during both baseline and hypogonadism and significantly decreased in both sexes during hypogonadism compared with baseline. Each of the individual DISF subscales demonstrated a similar significant effect of hormone condition (decreased during hypogonadism), and in scales nos. 2 and 4 (ie, arousal and orgasm), we observed significant effects of sex (higher in men) and a sex by hormone condition interaction, reflecting greater decline in men than women during hypogonadism. An identical pattern of effects was observed when the nine men who received T replacement before placebo were excluded from the analysis.
Eight men (40%) and seven women (35%) experienced a 50% or greater decline in total DISF scores during hypogonadism: (χ2=0.12, p=0.7); similarly, 12 men (60%) and 14 women (70%) experienced a 30% or greater decline in total DISF scores during hypogonadism. Five of the eight men who experienced a 50% or greater decline in total DISF received placebo first.
Comparisons between those with high and low baseline DISF scores
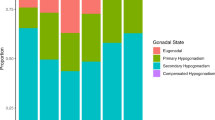
Women with low and high total DISF scores at baseline had significantly different responses to induced hypogonadism (Figure 1). No significant effects of hormone condition were observed in the low baseline symptom group (t30 (range)=1.0–1.4, p=NS), with no significant differences between hypogonadism, E, and P compared with baseline. In contrast, the women with high total DISF scores at baseline had significantly lower scores during hypogonadism, E, and P compared with baseline conditions, (t30 (range)=4.6–5.4, p<0.01).
In men, a similar pattern of effects was observed, with the absence of significant differences (between hypogonadism and baseline or T) in the low baseline symptom group (t20 (range)=0.1–1.6, p=NS), whereas in the high baseline symptom group significantly lower DISF scores were observed during hypogonadism compared with baseline and T conditions (t20=6.1 and 7.5, respectively, p<0.01).
As a caveat, when data were re-analyzed using baseline DISF scores as a covariate, the significance of the effect of hormone condition was reduced to marginally significant levels (p=0.05 and 0.01 (women and men, respectively)).
Mood and Hormonal Measures
Characteristics of those with and without a clinically significant response to hypogonadism
Women with and without a 50% or greater reduction in total DISF scores were not distinguished by any variables, including total T and P (Student's t-values ranged from 0.9 to 1.0), with the exception of significantly lower baseline plasma E levels (in those women with a 50% reduction in DISF scores) (Student's t17=2.8, p=0.013) and a significantly greater decline in plasma E levels from baseline to hypogonadism in those without a 50% decrease (Student's t17=15.9, p=0.02). These findings reflected the presence of outlier values in the women without a 50% decrease that spuriously elevated mean baseline E levels. When three women with luteal phase plasma levels of E (ie, >100 pg/ml) were eliminated from the analysis, there were no differences between the groups. There were also no differences in plasma E levels between groups of women during hypogonadism (Student's t17=1.3, p=NS).
Similarly, no significant differences were observed between those men with and without a 50% or greater reduction in total DISF scores during hypogonadism (relative to baseline) in the following measures: age; BDI scores (at baseline, during hypogonadism, or the change in BDI score from baseline to hypogonadism); and plasma hormone levels (total and free T, DHT, and E) at baseline or during hypogonadism as well as the difference in plasma hormone levels between baseline and hypogonadism (Δ). (Student's t-values ranged from 0.7 to 1.0).
Finally, no baseline differences were observed between the high and low baseline symptom groups in either men or women (Student's t-values ranging from 0.5 to 1.0).
Hormone measures of experimental condition
Blood hormone levels confirmed the creation of the intended hormone conditions (Table 2). As expected, blood levels of T in women remained suppressed relative to baseline for the duration of the study (ie, despite E or P addback).
Hormonal correlates of DISF scores
No significant correlations were seen between the changes in hormone levels across conditions and the corresponding change in total DISF scores in either men or women.
DISCUSSION
Our hypotheses were that induced hypogonadism would impair sexual functioning across multiple domains and that there would be considerable variability in the impact of hypogonadism on sexual functioning in both men and women. Both of these hypotheses were confirmed, albeit with sex differences in the domains of sexual functioning influenced by induced hypogonadism. The findings of this study have implications for clinicians’ expectations about the impact of hypogonadism on an individual's sexual function and, possibly, for the selection of men and women who would be appropriate candidates for hormone therapies targeted at improving sexual function. First, in women, short-term induced hypogonadism was associated principally with a significant decrease in the reported quality of orgasm, whereas in men, hypogonadism significantly reduced all domains of sexual function measured by the DISF. In men, testosterone replacement restored sexual function to that observed at baseline, whereas in women, neither estradiol nor progesterone replacement reversed the reduction in sexual functioning caused by hypogonadism. Despite the reduction in sexual function observed on a group basis, only 40% of men and 35% of women reported substantial decreases in sexual function during induced hypogonadism (ie, 50% or greater decline in total DISF scores relative to baseline). Second, we observed no sex differences in the proportion of participants who responded with a substantial decline in sexual function during hypogonadism. Third, those participants with and without a significant decline in DISF scores during hypogonadism were not distinguished by any measure, including baseline mood symptom ratings (ie, BDI scores) and both baseline and post GnRH agonist hormone measures. Finally, men and women with high baseline DISF scores responded differently to hypogonadism than those with lower baseline DISF scores. Thus, levels of sexual function at baseline (ie, total DISF score) in both men and women predicted the magnitude of the decline in sexual function during hypogonadism and, in men, the improvement in sexual function after testosterone replacement. This study was designed to evaluate the effects of hypogonadism and sex steroid replacement on measures of mood; sexual function was not a primary outcome measure. However, the hormone manipulations performed represented a unique opportunity to examine the effects of hypogonadism (albeit short term) on measures of sexual function in young healthy men and women. The absence of a T replacement arm in women and the relatively small sample sizes limit our conclusions about the source of the decline in libido in women. Nonetheless, short-term hypogonadism was associated with a decline in measures of sexual function in both men and women.
In men, the reduced sexual function during hypogonadism was restored to baseline levels by testosterone replacement. These data in men are consistent with previous reports of impaired sexual functioning in hypogonadal men and the restoration of sexual function with testosterone replacement (Bhasin, 2000; Guay et al, 1995; Anderson et al, 1999; Snyder et al, 2000; Seftel et al, 2004; Isidori et al, 2005; Steidle et al, 2003; Gray et al, 2005; O’Carroll et al, 1985; Wang et al, 2000; Davidson et al, 1979; Kwan et al, 1983). The observed changes in sexual function in men during induced hypogonadism occurred independent of significant changes in mood symptoms (an increase in negative mood was reported in only two men). The reduction in global sexual function could be related to loss of testosterone, its 5 α-reduced metabolite DHT, estradiol (synthesized from testosterone within the brain by aromatase), or one of testosterone's neurosteroid metabolites such as androsterone. Indeed, androsterone levels are implicated in the reduced libido observed in this trial. In a subsample of these men in whom lumbar punctures were performed, we observed that CSF androsterone levels but not CSF measures of T or DHT correlated with the symptom of decreased sexual function (Bloch et al, 2006).
In women, we observed a similar effect of hypogonadism on total DISF scores; however, in contrast to the effects of testosterone in men neither estradiol nor progesterone replacement restored sexual function to levels reported at baseline. The failure of estradiol to enhance sexual function is consistent with some (Nathorst-Boos et al, 1993a; Alexander et al, 2004; Lobo et al, 2003; Sherwin, 1985; Myers et al, 1990), but not all (Dennerstein et al, 1980, 2002; Finkelstein et al, 1998; Sarrel, 1990, 1998; Sarrel et al, 1998; Sherwin, 1991; Nathorst-Boos et al, 1993b; Wiklund et al, 1993), studies reporting an association between estradiol levels and sexual function. While we did observe sexual function to decline in association with hypogonadism-induced decreases in ovarian estradiol secretion (perhaps consistent with earlier studies), sexual function was not restored by estradiol replacement. Blood levels of both estradiol and progesterone increased during each of their respective replacement conditions, but only slight nonsignificant increases in DISF scores accompanied these changes. Nonetheless, it is possible that had we studied a larger sample of women with decreased libido, or had we employed higher doses or provided a longer duration of therapy of estradiol (or possibly progesterone), a larger impact on sexual function would have been observed. The doses employed in this study, however, were adequate to reduce hot flushes (estradiol and progesterone) and self-reports of vaginal dryness (estradiol only). While no statistically significant effects of estradiol on sexual functioning were observed, an improvement in sexual function after estradiol was observed and, therefore, a type II error cannot be ruled out. Blood levels of both testosterone and DHT remained suppressed in women throughout all three hormone conditions in which DISF scores were reduced relative to baseline. Blood testosterone levels were decreased by approximately 30% during Lupron-induced hypogonadism compared with baseline and, therefore, changes in testosterone (or one of its androgen or neurosteroid metabolites) could mediate the observed decline in sexual function and quality of orgasm in women (Simon et al, 2005; Sherwin et al, 1985; Lobo et al, 2003; Nathorst-Boos et al, 2006; Braunstein et al, 2005; Sherwin and Gelfand, 1987; Shifren et al, 2000; Floter et al, 2002; Davis et al, 2006; Leiblum et al, 2006; Santoro et al, 2005). However, since testosterone was not administered to women in this study, we only can speculate about this possible relationship.
The robust decline in the reported quality of orgasm during hypogonadism contrasts with the results of many, but not all, studies examining the effects of testosterone therapy on domains of sexual function in women. Studies by Sherwin et al (1985) and Floter et al (2002) observed testosterone to enhance arousal and motivational aspects of sexual function in hypogonadal women, but neither quality of orgasm nor sexual behavior was increased. Although the Sherwin data (Sherwin et al, 1985) suggested that orgasm and sexual behavior were influenced less by androgens, more recent studies employing transdermal testosterone have observed improvements in all domains of sexual function, including orgasm and frequency of intercourse (Simon et al, 2005; Shifren et al, 2000; Braunstein et al, 2005; Nathorst-Boos et al, 2006).
Despite significant changes on a group basis, only 35% and 40% of women and men, respectively, experienced a substantial (50% or greater) decline in DISF scores during hypogonadism. At first glance, the proportion of participants in whom hypogonadism reduced sexual function seems remarkably small; however, these data are consistent with several prior studies in which rates of moderate to severe sexual dysfunction ranged from 20% to 50% in women postmenopause or post-oophorectomy (with studies of women post-oophorectomy reporting higher rates of clinically significant loss of libido compared with the natural menopause) (Leiblum et al, 2006; Bremer, 1959; Dennerstein et al, 1977, 2002; Chakravarti et al, 1977; Koster and Garde, 1993; Elit et al, 2001; Madalinska et al, 2005; Bachmann et al, 1985; Teplin et al, 2006). The rate of reduced sexual function in men (40%) is lower than the rates of post-castration loss of sexual function of 50% or greater reported by some case series (Bagatell et al, 1994; Bremer, 1959; Tauber, 1940; Basaria et al, 2002). Our data demonstrate that induced hypogonadism, at least short term, does not result in a clinically significant loss of sexual function in all men and women. Thus, as with many other non-reproductive behaviors, there is a differential response of sexual function to changes in reproductive function, with only a proportion of subjects experiencing a significant change in behavior despite a similar decrease in sex steroid hormone secretion. These data also could explain the findings of several treatment studies in which sex hormone therapy was not uniformly effective in enhancing libido (Seftel et al, 2004; Isidori et al, 2005; Davidson et al, 1979).
Several factors have been reported to modify the behavioral response to declining or loss of sex steroid secretion, including age, sex, extent of hormone suppression, quality of relationship with partner, coexisting stress or mood symptoms, or levels of adrenal hormones (Gray et al, 2005; Koster and Garde, 1993; Beutel et al, 2005; Cawood and Bancroft, 1996; Bachmann et al, 1985; Davidson et al, 1983; Basar et al, 2005; Nilsson et al, 1995; Kratzik et al, 2004; Finkelstein et al, 1998; Schiavi and White, 1976; Schiavi et al, 1994). However, with the exception of baseline DISF scores, no baseline characteristic was associated with the level of impaired libido during hypogonadism, including age (although all participants were of a similar young age), depression scores during hypogonadism, hormone levels during either baseline or hypogonadal conditions, and change in hormone levels across conditions. Men and women with higher baseline levels of sexual function (high group) experienced the greatest loss of sexual function during hypogonadism; however, these participants were not distinguished by any other characteristic measured in this study. These data are consistent with and extend our previous observations in men (Schmidt et al, 2004) as well as those in animals by Grunt and Young (1952, 1953), who reported that baseline levels of sexual activity predicted the response to castration and testosterone replacement in male guinea pigs. A floor effect may have prevented detection of a decline in DISF scores during hypogonadism in the low symptom group. Baseline DISF scores clearly contributed to the results we observed; nonetheless, the effect of hormone condition cannot solely be attributed to those with elevated baseline DISF scores. An important role for sex steroids in at least some men and women is suggested both by the loss of sexual function in men and women in the high baseline sexual function groups and by the restoration of normal sexual function by testosterone in the high baseline sexual function men (but not in the low symptom groups despite comparable changes in sex steroids). Thus, our data and those of others (Gray et al, 2005) suggest that a behavioral phenotype could predict a disparate response to changes (either decreases or increases) in sex steroid secretion. This phenotype could contribute to the heterogeneity of the changes in sexual function during reproductive aging in both men and women.
This study has several limitations: first, the duration of hypogonadism was relatively brief, and it is possible, therefore, that a longer duration of hypogonadism would have resulted in a larger proportion of men and women developing clinically significant losses of sexual function or different patterns of loss with respect to specific domains of sexual function. Indeed, in our earlier report (Schmidt et al, 2004), in a larger sample, those men exposed to two consecutive months of hypogonadism reported a greater decline in sexual function. Nonetheless, the relative proportion of women affected in this study is comparable to rates of significant loss of sexual function in previous studies in women after oophorectomy or natural menopause (Leiblum et al, 2006; Dennerstein et al, 1977, 2002; Chakravarti et al, 1977; Koster and Garde, 1993; Elit et al, 2001; Madalinska et al, 2005). Indeed, even in men, studies have reported that a loss of sexual function is not observed in 100% of hypogonadal men (Bagatell et al, 1994; Bremer, 1959). Second, although we controlled for several factors that could contribute to sexual function, including age, concurrent symptoms, and sex, we did not obtain detailed information about the quality of the relationships in participants (Bachmann et al, 1985). We also did not measure adrenal hormones (cortisol and dehydroepiandrosterone (DHEA)) (Basar et al, 2005), although neither baseline DHEA nor cortisol secretion would be predictably altered by GnRH agonist treatment. Finally, we studied young healthy men and women, and the rate of sexual dysfunction after hypogonadism could be higher in older subjects or in those with concurrent medical illnesses. Thus, our findings should not be generalized to older men and women.
Future studies should investigate other possible biological or environmental contributors to the difference in behavioral response to permit a better characterization of this hormonally vulnerable group of men and women.
References
Abraham GE (1973). Radioimmunoassay of plasma steroid hormones. In: Heftman E (ed). Modern Methods of Steroid Analysis. Academic Press: New York. pp 451–470.
Abraham GE, Buster JD, Lucas LA, Corrales PC, Teller RC (1972). Chromatographic separation of steroid hormones for use in radioimmunoassay. Anal Lett 5: 509–517.
Adams DB, Gold AR, Burt AD (1978). Rise in female-initiated sexual activity at ovulation and its suppression by oral contraceptives. N Engl J Med 299: 1145–1150.
Alexander JL, Kotz K, Dennerstein L, Kutner SJ, Wallen K, Notelovitz M (2004). The effects of postmenopausal hormone therapies on female sexual functioning: a review of double-blind, randomized controlled trials. Menopause 11: 749–765.
Anderson RA, Martin CW, Kung AW, Everington D, Pun TC, Tan KC et al (1999). 7α-Methyl-19-nortestosterone maintains sexual behavior and mood in hypogonadal men. J Clin Endocrinol Metab 84: 3556–3562.
Arlt W, Callies F, van Vlijmen JC, Koehler I, Reincke M, Bidlingmaier M et al (1999). Dehydroepiandrosterone replacement in women with adrenal insufficiency. N Engl J Med 341: 1013–1020.
Bachmann GA, Leiblum SR, Sandler B, Ainsley W, Narcessian R, Shelden R et al (1985). Correlates of sexual desire in post-menopausal women. Maturitas 7: 211–216.
Bagatell CJ, Heiman JR, Rivier JE, Bremner WJ (1994). Effects of endogenous testosterone and estradiol on sexual behavior in normal young men. J Clin Endocrinol Metab 78: 711–716.
Bancroft J, Davidson DW, Warner P, Tyrer G (1980). Androgens and sexual behaviour in women using oral contraceptives. Clin Endocrinol 12: 327–340.
Basar MM, Aydin G, Mert HC, Keles I, Caglayan O, Orkun S et al (2005). Relationship between serum sex steroids and aging male symptoms score and international index of erectile function. Urology 66: 597–601.
Basaria S, Lieb II J, Tang AM, DeWeese T, Carducci M, Eisenberger M et al (2002). Long-term effects of androgen deprivation therapy in prostate cancer patients. Clin Endocrinol 56: 779–786.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961). An inventory for measuring depression. Arch Gen Psychiatry 4: 561–571.
Beutel ME, Wiltink J, Hauck EW, Auch D, Behre HM, Brahler E et al (2005). Correlations between hormones, physical, and affective parameters in aging urologic outpatients. Eur Urol 47: 749–755.
Bhasin S (2000). The dose-dependent effects of testosterone on sexual function and on muscle mass and function. Mayo Clin Proc 75 (Suppl): S70–S76.
Bloch M, Rubinow DR, Berlin K, Kevala KR, Kim HY, Schmidt PJ (2006). Monoamines and neurosteroids in sexual function during induced hypogonadism in healthy men. Arch Gen Psychiatry 63: 450–456.
Braunstein GD, Sundwall DA, Katz M, Shifren JL, Buster JE, Simon JA et al (2005). Safety and efficacy of a testosterone patch for the treatment of hypoactive sexual desire disorder in surgically menopausal women: a randomized, placebo-controlled trial. Arch Intern Med 165: 1582–1589.
Bremer J (1959). Asexualization. A Follow-up Study of 244 Cases. Oslo University Press: Oslo, Norway, 366pp.
Burger HG, Dudley EC, Cui J, Dennerstein L, Hopper JL (2000). A prospective longitudinal study of serum testosterone, dehydroepiandrosterone sulfate, and sex hormone-binding globulin levels through the menopause transition. J Clin Endocrinol Metab 85: 2832–2838.
Burger HG, Dudley EC, Hopper JL, Groome N, Guthrie JR, Green A et al (1999). Prospectively measured levels of serum follicle-stimulating hormone, estradiol, and the dimeric inhibins during the menopausal transition in a population-based cohort of women. J Clin Endocrinol Metab 84: 4025–4030.
Burger HG, Dudley EC, Hopper JL, Shelley JM, Green A, Smith A et al (1995). The endocrinology of the menopausal transition: a cross-sectional study of a population-based sample. J Clin Endocrinol Metab 80: 3537–3545.
Carani C, Granata ARM, Rochira V, Caffagni G, Aranda C, Antunez P et al (2005). Sex steroids and sexual desire in a man with a novel mutation of aromatase gene and hypogonadism. Psychoneuroendocrinology 30: 413–417.
Cawood EH, Bancroft J (1996). Steroid hormones, the menopause, sexuality and well-being of women. Psychol Med 26: 925–936.
Chakravarti S, Collins WP, Newton JR, Oram DH, Studd JWW (1977). Endocrine changes and symptomatology after oophorectomy in premenopausal women. Br J Obstet Gynaecol 84: 769–775.
Davidson JM, Camargo CA, Smith ER (1979). Effects of androgen on sexual behavior in hypogonadal men. J Clin Endocrinol Metab 48: 955–958.
Davidson JM, Chen JJ, Crapo L, Gray GD, Greenleaf WJ, Catania JA (1983). Hormonal changes and sexual function in aging men. J Clin Endocrinol Metab 57: 71–77.
Davis SR, Goldstat R, Papalia MA, Shah S, Kulkarni J, Donath S et al (2006). Effects of aromatase inhibition on sexual function and well-being in postmenopausal women treated with testosterone: a randomized, placebo-controlled trial. Menopause 13: 37–45.
Dennerstein L, Burrows GD, Wood C, Hyman G (1980). Hormones and sexuality: effect of estrogen and progestogen. Obstet Gynecol 56: 316–322.
Dennerstein L, Gotts G, Brown JB, Morse CA, Farley TMM, Pinol A (1994). The relationship between the menstrual cycle and female sexual interest in women with PMS complaints and volunteers. Psychoneuroendocrinology 19: 293–304.
Dennerstein L, Randolph J, Taffe J, Dudley E, Burger H (2002). Hormones, mood, sexuality, and the menopausal transition. Fertil Steril 77 (Suppl 4): 42–48.
Dennerstein L, Wood C, Burrows GD (1977). Sexual response following hysterectomy and oophorectomy. Obstet Gynecol 49: 92–96.
Derogatis LR (1997). The Derogatis interview for sexual functioning (DISF/DISF-SR): an introductory report. J Sex Marital Ther 23: 291–304.
Doering CH, Brodie HKH, Kraemer H, Becker H, Hamburg DA (1974). Plasma testosterone levels and psychologic measures in men over a 2-month period. In: Friedman RC, Reichart RM, Vande Wiele RL (eds). Sex Differences in Behavior. Wiley: New York. pp 413–431.
Dreher J, Schmidt PJ, Kohn P, Furman D, Rubinow D, Berman KF (2007). Menstrual cycle phase modulates reward-related neural function in women. Proc Natl Acad Sci USA 104: 2465–2470.
Elit L, Esplen MJ, Butler K, Narod S (2001). Quality of life and psychosexual adjustment after prophylactic oophorectomy for a family history of ovarian cancer. Fam Cancer 1: 149–156.
Evans SM, Foltin RW (2006). Exogenous progesterone attenuates the subjective effects of smoked cocaine in women, but not in men. Neuropsychopharmacology 31: 659–674.
Finkelstein JW, Susman EJ, Chinchilli VM, D’Arcangelo MR, Kunselman SJ, Schwab J et al (1998). Effects of estrogen or testosterone on self-reported sexual responses and behaviors in hypogonadal adolescents. J Clin Endocrinol Metab 83: 2281–2285.
Floter A, Nathorst-Boos J, Carlstrom K, Von Schoultz B (2002). Addition of testosterone to estrogen replacement therapy in oophorectomized women: effects on sexuality and well-being. Climacteric 5: 357–365.
Frye CA (2007). Progestins influence motivation, reward, conditioning, stress, and/or response to drugs of abuse. Pharmacol Biochem Behav 86: 209–219.
Furuyama S, Mayes DM, Nugent CA (1970). A radioimmunoassay for plasma testosterone. Steroids 16: 415–428.
Gray PB, Singh AB, Woodhouse LJ, Storer TW, Casaburi R, Dzekov J et al (2005). Dose-dependent effects of testosterone on sexual function, mood, and visuospatial cognition in older men. J Clin Endocrinol Metab 90: 3838–3846.
Greendale GA, Hogan P, Shumaker S (1996). Sexual functioning in postmenopausal women: the postmenopausal estrogen/progestin interventions (PEPI) trial. J Womens Health 5: 445–458.
Grinspoon S, Corcoran C, Stanley T, Baaj A, Basgoz N, Klibanski A (2000). Effects of hypogonadism and testosterone administration on depression indices in HIV-infected men. J Clin Endocrinol Metab 85: 60–65.
Grunt JA, Young WC (1952). Differential reactivity of individuals and the response of the male guinea pig to testosterone propionate. Endocrinology 51: 237–248.
Grunt JA, Young WC (1953). Consistency of sexual behavior patterns in individual male guinea pigs following castration and androgen therapy. J Comp Physiol Psychol 46: 138–144.
Guay AT, Bansal S, Heatley GJ (1995). Effect of raising endogenous testosterone levels in impotent men with secondary hypogonadism: double blind placebo-controlled trial with clomiphene citrate. J Clin Endocrinol Metab 80: 3546–3552.
Herzog AG, Drislane FW, Schomer DL, Pennell PB, Bromfield EB, Dworetzky BA et al (2005). Differential effects of antiepileptic drugs on sexual function and hormones in men with epilepsy. Neurology 65: 1016–1020.
Isidori AM, Giannetta E, Gianfrilli D, Greco EA, Bonifacio V, Aversa A et al (2005). Effects of testosterone on sexual function in men: results of a meta-analysis. Clin Endocrinol 63: 381–394.
Ito T, Horton R (1970). Dihydrotestosterone in human peripheral plasma. J Clin Endocr 31: 362–368.
Jiang N-S, Ryan PJ (1969). Radioimmunoassay for estrogens: a preliminary communication. Mayo Clin Proc 44: 461–465.
Johannsson G, Burman P, Wiren L, Engstrom BE, Nilsson AG, Ottosson M et al (2002). Low dose dehydroepiandrosterone affects behavior in hypopituitary androgen-deficient women: a placebo-controlled trial. J Clin Endocrinol Metab 87: 2046–2052.
Kennedy RG, Davies T, Al-Azzawi F (1997). Sexual interest in postmenopausal women is related to 5α-reductase activity. Hum Reprod 12: 209–213.
Koster A, Garde K (1993). Sexual desire and menopausal development. A prospective study of Danish women born in 1936. Maturitas 16: 49–60.
Kratzik CW, Reiter WJ, Riedl AM, Lunglmayr G, Brandstatter N, Rucklinger E et al (2004). Hormone profiles, body mass index and aging male symptoms: results of the Androx Vienna Municipality study. Aging Male 7: 188–196.
Kwan M, Greenleaf WJ, Mann J, Crapo L, Davidson JM (1983). The nature of androgen action on male sexuality: a combined laboratory-self-report study on hypogonadal men. J Clin Endocrinol Metab 57: 557–562.
Leiblum SR, Koochaki PE, Rodenberg CA, Barton IP, Rosen RC (2006). Hypoactive sexual desire disorder in postmenopausal women: US results from the Women's International Study of Health and Sexuality (WISHeS). Menopause 13: 46–56.
Lobo RA, Rosen RC, Yang HM, Block B, Van Der Hoop RG (2003). Comparative effects of oral esterified estrogens with and without methyltestosterone on endocrine profiles and dimensions of sexual function in postmenopausal women with hypoactive sexual desire. Fertil Steril 79: 1341–1352.
Madalinska JB, Hollenstein J, Bleiker E, van Beurden M, Valdimarsdottir HB, Massuger LF et al (2005). Quality-of-life effects of prophylactic salpingo-oophorectomy vs gynecologic screening among women at increased risk of hereditary ovarian cancer. J Clin Oncol 23: 6890–6898.
Marberger M, Roehrborn CG, Marks LS, Wislon T, Rittmaster RS (2006). Relationship among serum testosterone, sexual function, and response to treatment in men receiving dutasteride for benign prostatic hyperplasia. J Clin Endocrinol Metab 91: 1323–1328.
Meuwissen I, Over R (1992). Sexual arousal across phases of the human menstrual cycle. Arch Sex Behav 21: 101–119.
Modelska K, Litwack S, Ewing SK, Yaffe K (2004). Endogenous estrogen levels affect sexual function in elderly post-menopausal women. Maturitas 49: 124–133.
Myers LS, Dixen J, Morrissette D, Carmichael M, Davidson JM (1990). Effects of estrogen, androgen, and progestin on sexual psychophysiology and behavior in postmenopausal women. J Clin Endocrinol Metab 70: 1124–1131.
Nathorst-Boos J, Floter A, Jarkander-Rolff M, Carlstrom K, Von Schoultz B (2006). Treatment with percutaneous testosterone gel in postmenopausal women with decreased libido—effects on sexuality and psychological general well-being. Maturitas 53: 11–18.
Nathorst-Boos J, Von Schoultz B, Carlstrom K (1993a). Elective ovarian removal and estrogen replacement therapy—effects on sexual life, psychological well-being and androgen status. J Psychosom Obstet Gyn 14: 283–293.
Nathorst-Boos J, Wiklund I, Mattsson LA, Sandin K, Von Schoultz B (1993b). Is sexual life influenced by transdermal estrogen therapy? A double blind placebo controlled study in postmenopausal women. Acta Obstet Gynecol Scand 72: 656–660.
Nilsson PM, Moller L, Solstad K (1995). Adverse effects of psychosocial stress on gonadal function and insulin levels in middle-aged males. J Intern Med 237: 479–486.
Nyunt A, Stephen G, Gibbin J, Durgan L, Fielding AM, Wheeler M et al (2005). Androgen status in healthy premenopausal women with loss of libido. J Sex Marital Ther 31: 73–80.
O’Carroll R, Shapiro C, Bancroft J (1985). Androgens, behaviour and nocturnal erection in hypogonadal men: the effects of varying the replacement dose. Clin Endocrinol (Oxf) 23: 527–538.
Rabkin JG, Ferrando SJ, Wagner GJ, Rabkin R (2000). DHEA treatment for HIV+ patients: effects on mood, androgenic and anabolic parameters. Psychoneuroendocrinology 25: 53–68.
Rabkin JG, McElhiney MC, Rabkin R, McGrath PJ, Ferrando SJ (2006). Placebo-controlled trial of dehydroepiandrosterone (DHEA) for treatment of nonmajor depression in patients with HIV/AIDS. Am J Psychiatry 163: 59–66.
Rosner W, Auchus RJ, Azziz R, Sluss PM, Raff H (2007). Utility, limitations, and pitfalls in measuring testosterone: an endocrine society position statement. J Clin Endocrinol Metab 92: 405–413.
Santoro N, Brown JR, Adel T, Skurnick JH (1996). Characterization of reproductive hormonal dynamics in the perimenopause. J Clin Endocrinol Metab 81: 1495–1501.
Santoro N, Torrens J, Crawford S, Allsworth JE, Finkelstein JS, Gold EB et al (2005). Correlates of circulating androgens in mid-life women: the study of women's health across the nation. J Clin Endocrinol Metab 90: 4836–4845.
Sarrel P, Dobay B, Wiita B (1998). Estrogen and estrogen–androgen replacement in postmenopausal women dissatisfied with estrogen-only therapy. Sexual behavior and neuroendocrine responses. J Reprod Med 43: 847–856.
Sarrel PM (1990). Sexuality and menopause. Obstet Gynecol 75: 26S–35S.
Sarrel PM (1998). Ovarian hormones and vaginal blood flow: using laser Doppler velocimetry to measure effects in a clinical trial of post-menopausal women. Int J Impot Res 10 (Suppl 2): S91–S93.
Schiavi RC, Mandeli J, Schreiner-Engel P (1994). Sexual satisfaction in healthy aging men. J Sex Marital Ther 20: 3–13.
Schiavi RC, Schreiner-Engel P, White D, Mandeli J (1991). The relationship between pituitary–gonadal function and sexual behavior in healthy aging men. Psychosom Med 53: 363–374.
Schiavi RC, White D (1976). Androgens and male sexual function: a review of human studies. J Sex Marital Ther 2: 214–228.
Schmidt PJ, Berlin KL, Danaceau MA, Neeren A, Haq NA, Roca CA et al (2004). The effects of pharmacologically induced hypogonadism on mood in healthy men. Arch Gen Psychiatry 61: 997–1004.
Seftel AD, Mack RJ, Secrest AR, Smith TM (2004). Restorative increases in serum testosterone levels are significantly correlated to improvements in sexual functioning. J Androl 25: 963–972.
Sherwin BB (1985). Changes in sexual behavior as a function of plasma sex steroid levels in post-menopausal women. Maturitas 7: 225–233.
Sherwin BB (1991). The impact of different doses of estrogen and progestin on mood and sexual behavior in postmenopausal women. J Clin Endocrinol Metab 72: 336–343.
Sherwin BB, Gelfand MM (1987). The role of androgen in the maintenance of sexual functioning in oophorectomized women. Psychosom Med 49: 397–409.
Sherwin BB, Gelfand MM, Brender W (1985). Androgen enhances sexual motivation in females: a prospective, crossover study of sex steroid administration in the surgical menopause. Psychosom Med 47: 339–351.
Shifren JL, Braunstein GD, Simon JA, Casson PR, Buster JE, Redmond GP et al (2000). Transdermal testosterone treatment in women with impaired sexual function after oophorectomy. N Engl J Med 343: 682–688.
Simon J, Braunstein G, Nachtigall L, Utian W, Katz M, Miller S et al (2005). Testosterone patch increases sexual activity and desire in surgically menopausal women with hypoactive sexual desire disorder. J Clin Endocrinol Metab 90: 5226–5233.
Slob AK, Bax CM, Hop WCJ, Rowland DL, van der Werff ten Bosch JJ (1996). Sexual arousability and the menstrual cycle. Psychoneuroendocrinology 21: 545–558.
Snyder PJ, Peachey H, Berlin JA, Hannoush P, Haddad G, Dlewati A et al (2000). Effects of testosterone replacement in hypogonadal men. J Clin Endocrinol Metab 85: 2670–2677.
Spitzer RL, Williams JB, Gibbon M, First MB (1990). Structured Clinical Interview for DSM-III-R, patient edition. Biometrics Research Department, New York State Psychiatric Institute: New York, NY.
Steidle C, Schwartz S, Jacoby K, Sebree T, Smith T, Bachand R et al (2003). AA2500 testosterone gel normalizes androgen levels in aging males with improvements in body composition and sexual function. J Clin Endocrinol Metab 88: 2673–2681.
Sternbach H (1998). Age-associated testosterone decline in men: clinical issues for psychiatry. Am J Psychiatry 155: 1310–1318.
Tauber ES (1940). Effects of castration upon the sexuality of the adult male. Psychosom Med 11: 74–87.
Teplin V, Vittinghoff E, Learman LA, Kuppermann M (2006). Sexual functioning and quality of life after oophorectomy in premenopausal women. Obstet Gynecol 107: 18S–19S.
Travison TG, Morley JE, Araujo AB, O’Donnell AB, McKinlay JB (2006). The relationship between libido and testosterone levels in aging men. J Clin Endocrinol Metab 91: 2509–2513.
Vermeulen A (2001). Androgen replacement therapy in the aging male—a critical evaluation. J Clin Endocrinol Metab 86: 2380–2390.
Vermeulen A, Stoica T, Verdonck L (1971). The apparent free testosterone concentration, an index of androgenicity. J Clin Endocr 33: 759–767.
Wallen K (1990). Desire and ability: hormones and the regulation of female sexual behavior. Neurosci Biobehav Rev 14: 233–241.
Wallen K (2001). Sex and context: hormones and primate sexual motivation. Horm Behav 40: 339–357.
Wang C, Swerdloff RS, Iranmanesh A, Dobs A, Snyder PJ, Cunningham G et al (2000). Transdermal testosterone gel improves sexual function, mood, muscle strength, and body composition parameters in hypogonadal men. J Clin Endocrinol Metab 85: 2839–2853.
Wiklund I, Karlberg J, Mattsson LA (1993). Quality of life of postmenopausal women on a regimen of transdermal estradiol therapy: a double-blind placebo-controlled study. Am J Obstet Gynecol 168: 824–830.
Wu CH, Lundy LE (1971). Radioimmunoassay of plasma estrogens. Steroids 18: 91–111.
Zehr JL, Maestripieri D, Wallen K (1998). Estradiol increases female sexual initiation independent of male responsiveness in rhesus monkeys. Horm Behav 33: 95–103.
Zussman L, Zussman S, Sunley R, Bjornson E (1981). Sexual response after hysterectomy–oophorectomy: recent studies and reconsideration of psychogenesis. Am J Obstet Gynecol 140: 725–729.
Acknowledgements
We acknowledge the important contributions to this paper of Lynnette Nieman, MD, for her clinical and research consultation, Robert Hamer, PhD (Department of Psychiatry, University of North Carolina, Chapel Hill, NC), for his statistical consultation, Linda Schenkel for her assistance with data management, and Merry Danaceau, RN, for her assistance in the clinic. We gratefully acknowledge the material support (estradiol and placebo skin patches) for this research provided by Watson Pharmaceuticals. This paper was written as part of Peter J Schmidt's official duties as a Government employee. The views expressed in this article do not necessarily represent the views of the NIMH, NIH, HHS, or the United States Government.
Author information
Authors and Affiliations
Corresponding author
Additional information
DISCLOSURE
This work was supported by the National Institute of Mental Health's Intramural Research Program. Dr Schmidt had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Other authors have nothing to disclose.
Rights and permissions
About this article
Cite this article
Schmidt, P., Steinberg, E., Negro, P. et al. Pharmacologically Induced Hypogonadism and Sexual Function in Healthy Young Women and Men. Neuropsychopharmacol 34, 565–576 (2009). https://doi.org/10.1038/npp.2008.24
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2008.24
Keywords
This article is cited by
-
Gonadotropin-releasing hormone (GnRH) deficiency under treatment: psychological and sexual functioning impacts
Hormones (2018)
-
The Effect of Targeted Therapy for Genitourinary Malignancies on Sexual Function and Fertility
Current Urology Reports (2017)
-
Perspective: Sex Matters: Gonadal Steroids and the Brain
Neuropsychopharmacology (2009)