Key Points
-
Details a real life clinical case demonstrating first-hand the healing of an area of mandible that has only been reported in literature.
-
Highlights new class of drugs that many readers may not be aware of.
-
Suggests knowing about this new class of drugs could be life changing for a patient.
-
Advises how to manage this condition should it arise.
Abstract
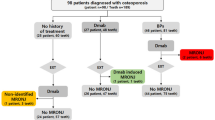
A patient was referred by a clinical oncologist regarding a non-healing area of bone in the lower jaw. The patient was taking denosumab (Prolia®, Xgeva®) when they had a tooth extracted and the area failed to heal. Following suspension of the drug, the area healed with mucosal coverage. This new class of drugs are being increasingly used as an alternative antiresorptive drug to bisphosphonates and are licenced in the UK for prevention of osteoporotic fractures and prevention of skeletal-related events (SREs) in patients with metastatic cancer.
Similar content being viewed by others
Introduction
Bisphosphonate related osteonecrosis of the jaws has been recognised since Marx in 2003.1 Initially, it was understood that osteonecrosis occurred in patients taking bisphosphonates, but there are now reports of osteonecrosis of the jaw (ONJ) with denosumab. This is a human monoclonal antibody that binds RANKL (Receptor Activator of Nuclear Factor Kappa-B Ligand), inhibiting osteoclast differentiation. It is administered via a subcutaneous injection, inhibiting osteoclast formation, function and survival, in turn decreasing bone turnover.2 This has broadened the list of drugs associated with ONJ, which has been renamed medication related osteonecrosis of the jaw – MRONJ, by the American Association of Oral and Maxillofacial Surgeons.
Denosumab was approved by the FDA in 2010 for:
-
Unresectable giant cell tumours
-
To increase bone mass in patients at high risk of fracture following prostate or breast cancer for prevention of skeletal related events (SREs)
-
Treatment of menopausal women with osteoporosis at high risk of fracture.3
The Medicines and Healthcare products Regulatory Agency (MHRA) launched a drug safety update in July 2015 warning healthcare professionals about how to further minimise risk.
The MRONJ classification in Table 1 is based on presence of exposed bone in the oral and maxillofacial region for more than eight weeks, in the absence of malignancy or radiation on a background of antiresorptive or anti-angiogenic drug use.4
Case report
A 68-year-old woman attended the dental department at Gartnavel General Hospital, following referral from a clinical oncologist within the hospital in October 2014, complaining of a non-healing area of the lower left jaw where a tooth had been removed. There was no associated pain, swelling or discharge reported. In July 2014 the patient had a tooth extracted in the lower left quadrant by her general dental practitioner (GDP). This was an atraumatic extraction of tooth 36 without any complication.
She had been diagnosed with ER+, HER2-breast cancer and underwent breast conserving surgery in October 2007. In December 2007 she was started on four cycles of chemotherapy (epirubicin, dexamethasone, granisetron) followed by four cycles of CMF (cyclophosphamide, methotrexate and 5-fluorouracil). She was then commenced on anastrozole (Arimidex). From July to August 2008 she had 25 fractions of radiotherapy to her right breast. Her co-morbidities included asthma and hypertension.
In June 2013 she presented with back pain and was found to have a solitary bone metastasis in her thoracic spine. In September 2013 she was started on monthly denosumab. Her medications other than denosumab included zopiclone, citalopram, amlodipine, calcichew and RD3. This patient was a non-smoker, however, she consumed 14 units of alcohol on a weekly basis.
She attended her GDP regularly. She suffered from dental anxiety regarding choking and had an upper partial denture. Although this patient was a regular attendee at her own GDP on a six monthly basis, her oral hygiene was poor.
Clinically, there was a 6mm x 2mm area of bone visible in the left mandible in November 2014 (Fig. 1). This represented Stage I MRONJ. The area was irrigated with chlorhexidine and she was provided with a chlorhexidine gluconate 0.2% mouthwash to be used twice daily.
A panoramic radiograph was taken in October 2014 (Fig. 2) which shows an evident socket with no bony infill. The radiograph also highlighted localised moderate-severe periodontitis in teeth 13, 21, 23 with generalised mild periodontitis in the remainder of the dentition. Secondary caries was present in 17 and 27. Caries was noted in 46 from which the patient reported a flare up at times with a 'dull ache when biting down.' To manage this, we liaised with her GDP who agreed to carry out a root canal treatment (RCT) and avoid further extractions due to the risk of further MRONJ.
Because of her diagnosis of MRONJ, her denosumab was suspended by the oncology team.
When she was seen again in December 2014, she was complaining of a tender lump in the area. Pus could be milked from the area. A diagnosis of Stage II MRONJ was made and she was prescribed amoxicillin 500mg and metronidazole 200mg, both to be taken three times daily for five days. In February 2015 the clinical picture had improved and stage I MRONJ was again diagnosed.
The ongoing management plan for this patient was twice daily use of chlorhexidine gluconate 0.2% mouthwash, four to six weekly review appointments with irrigation with chlorhexidine gluconate mouthwash. Hygiene appointments were made in which the patient learnt how to manage interdental cleaning and the importance of having a plaque free mouth.
The patient continued to be regularly reviewed with no changes in the size of the exposed bone. In July 2015, the patient presented to Gartnavel with a piece of bone from her mandible that had come loose (Fig. 3) and there appeared to be complete resolution of this patient's ONJ (Fig. 4). If this healing remains, extractions may be considered in the future if necessary.
Later that month, plans were made to restart her denosumab therapy. During the period of suspension of her denosumab, there was some progression of her spinal metastases. At her review in September 2015, she had no oral complaints. There was no breach in the mandibular alveolar mucosa. She was discharged to her GDP with advice on prevention and avoidance of extractions where possible.
Discussion
Bisphosphonates have a high affinity for calcium and bind to bone mineral surfaces, which ensures a long half-life within bone. They selectively localise to the sites of osteoclast activity and active bone remodelling.5 Unlike bisphosphonates, denosumab does not bind to bone and influence bone remodelling. It may therefore be reversible six months post therapy.6,7,8 Comparisons of monthly denosumab and IV bisphosphonates have shown that denosumab is similarly responsible for the occurrence of ONJ lesions.5
Current studies indicate that denosumab combined with other risk factors such as dental extractions, poor oral hygiene, use of removable prosthesis and chemotherapy may favour the development of osteonecrosis of the jaw (ONJ).
Regarding management of these patients, optimal oral hygiene is essential with regular preventative dental care.5 Patients must always be advised on the risks and benefits of antiresorptive therapy and the relation to dental therapy. Before commencing on this class of drugs it is advisable to undergo a thorough dental assessment as it has been shown that dento-alveolar trauma is the most prevalent risk factor for MRONJ.
Conclusion
This woman's complex case is one that needs a multidisciplinary approach involving a clinical oncologist, GDP, and special care dentist alongside the breast cancer care team. There continues to be an ongoing review of this case of MRONJ with prevention and restorative care with her GDP.
Dental care professionals should be aware of the importance of taking a thorough medical history from a patient and understanding the associated risks of antiresorptive agents related to oral healthcare, the timing of risk and the emphasis on prevention. There is potential for these lesions to heal and liaising with a medical practitioner would be advisable. The potential risk of further metastatic spread if the antiresorptive drug is withheld in order to allow resolution of the osteonecrotic lesion should be carefully considered.
There is currently no specific guidance for general dental or oral surgical management of these patients, but the MHRA weblink provides a useful source of information: https://www.gov.uk/drug-safety-update/denosumab-xgeva-prolia-intravenous-bisphosphonates-osteonecrosis-of-the-jaw-further-measures-to-minimise-risk.
In addition, the Scottish Dental Clinical Effectiveness Programme9 are in the process of updating their guidance on the oral health management of patients prescribed bisphosphonates, and it is to be expected that they will also consider other antiresorptive drugs.
References
Marx R . Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg 2003; 61: 1115–1117.
Pazianas M, Miller P, Blumentals W A, Bernal M, Kothawala P . A review of the literature on osteonecrosis of the jaw in patients with osteoporosis treated with oral bisphosphonates: prevalence, risk factors, and clinical characteristics. Clin Ther 2007: 29; 1548–1558.
Sivolella, S et al. Denosumab and anti-angiogenetic drug-related osteonecrosis of the jaw: an uncommon but potentially severe disease. Anticancer Res 2013; 33: 1793–1797.
Katsarelis H, Shah N P, Dhariwal D K, Pazianas M . Infection and medication-related osteonecrosis of the jaw. J Dent Res 2015; 94: 534–539.
Ruggiero S . Osteonecrosis of the jaw: BRONJ and ARONJ. Faculty Dent J 2014; 5: 90–93.
Dubois et al. Denosumab. Br J Clin Pharmacol 2011; 71: 804–806.
Kaur Sidhu H . Denosumab, an alternative to bisphosphonates but also associated with osteonecrosis of the jaw – what is the risk? Dent Update 2015; 42: 436.
Troeltzsch M, Woodlock T, Kriegelstein S et al. Physiology and pharmacology of nonbisphosphonate drusg implicated in osteonecrosis of the jaw. J Can Dent Assoc 2012; 78: c85.
Scottish Dental Clinical Effectiveness Programme. Oral Health Management of Patients Prescribed Bisphosphonates. 2011. Available online at http://www.sdcep.org.uk/published-guidance/bisphosphonates/ (accessed June 2016).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Lyttle, C., Paterson, H. Denosumab: a case of MRONJ with resolution. Br Dent J 220, 623–625 (2016). https://doi.org/10.1038/sj.bdj.2016.443
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2016.443
This article is cited by
-
Emerging therapies with potential risks of medicine-related osteonecrosis of the jaw: a review of the literature
British Dental Journal (2020)
-
Erratum: Corrigendum
British Dental Journal (2016)