Abstract
Over the past two decades, assessment and treatment of associated curvature has emerged as a major issue in treating patients with proximal hypospadias. However, the cut-off for defining a curvature as clinically significant is still unclear, as not all patients are bothered by the same degree of curvature and, although the need for a method to assess the curvature objectively has been emphasized, no standard method yet exists. Curvature is multifactorial. The same degree of curvature can be due to any possible combination of skin and/or subcutaneous dartos tethering, a short urethral plate and an intrinsic corpora disproportion. Different strategies can be used to treat curvature, depending on the underlying cause, surgeon preferences, and the goals of the repair. In the past 10 years, use of urethral plate transection and ventral lengthening procedures has increased, although the lack of long-term follow-up data on ventral lengthening procedures suggests that the use of such procedures should be selective. Furthermore, straightening manoeuvres are influenced by the technique used for subsequent urethroplasty and, in turn, may influence the success rate of the urethroplasty. This Review provides a comprehensive overview of the major developments from the past 10 years in the management of severe proximal hypospadias in children.
Key points
-
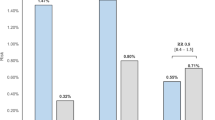
For clinical practice, 30° is a reasonable cut-off to define clinically significant curvature, but many patients with a curvature above this cut-off point might not be bothered by the curvature.
-
Objective measurement of curvature is important, but difficult to achieve consistently in patients with hypospadias preoperatively, intraoperatively and especially during follow-up.
-
The same degree of curvature can be caused by different factors and can require different treatments; therefore, a systematic step-wise approach is recommended for management.
-
In general, preserving the urethral plate does not contribute to straightening, is not advantageous for the urethroplasty, and can increase the risk of curvature recurrence and result in a shorter penis.
-
Ventral lengthening procedures can be important for straightening a penis without foreshortening it, but should be used judiciously in the absence of long-term follow-up data.
-
Similar outcomes can be achieved using different urethroplasty techniques and an important component of hypospadias repair is a skin reconfiguration with ventral transfer of healthy and well-vascularized skin.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Gong, E. M. & Cheng, E. Y. Current challenges with proximal hypospadias: we have a long way to go. J. Pediatr. Urol. 13, 457–467 (2017).
Pippi Salle, J. L. et al. Proximal hypospadias: a persistent challenge. Single institution outcome analysis of three surgical techniques over a 10-year period. J. Pediatr. Urol. 12, 28.e1–28.e7 (2016).
Snodgrass, W. & Bush, N. Staged tubularized autograft repair for primary proximal hypospadias with 30-degree or greater ventral curvature. J. Urol. 198, 680–686 (2017).
Spinoit, A. F. et al. Congenital penile pathology is associated with abnormal development of the dartos muscle: a prospective study of primary penile surgery at a tertiary referral center. J. Urol. 193, 1620–1624 (2015).
Atmoko, W. et al. Abnormal dartos fascia in buried penis and hypospadias: evidence from histopathology. J. Pediatr. Urol. 14, 536.e1–536.e7 (2018).
Snodgrass, W. A farewell to chordee. J. Urol. 178, 753–754 (2007).
Baskin, L. S., Duckett, J. W., Ueoka, K., Seibold, J. & Snyder, H. M. III Changing concepts of hypospadias curvature lead to more onlay flap procedures. J. Urol. 151, 191e6 (1994).
Snodgrass, W. & Bush, N. Tubularized incised plate proximal hypospadias repair: continued evolution and extended applications. J. Pediatr. Urol. 7, 2e9 (2011).
Castagnetti, M. & El-Ghoneimi, A. Surgical management of primary severe hypospadias in children: systematic 20-Year review. J. Urol. 184, 1469 (2010).
Snodgrass, W., Macedo, A., Hoebeke, P. & Mouriquand, P. D. Hypospadias dilemmas: a round table. J. Pediatr. Urol. 7, 145–157 (2011).
Bologna, R. A., Noah, T. A., Nasralla, P. F. & McMahon, D. R. Chordee: varied opinions and treatments as documented in a survey of the American Academy of Pediatrics, Section on Urology. Urology 53, 608e11 (1999).
Springer, A., Krois, W. & Horcher, E. Trends in hypospadias surgery: results of a worldwide survey. Eur. Urol. 60, 1184–1189 (2011).
Braga, L. H. P. et al. Ventral penile lengthening versus dorsal plication for severe ventral curvature in children with proximal hypospadias. J. Urol. 180, 1743e7 (2008).
Snodgrass, W. & Bush, N. C. Persistent or recurrent ventral curvature after failed proximal hypospadias repair. J. Pediatr. Urol. 15, 344.e1–344.e6 (2019).
Snodgrass, W. & Bush, N. Recurrent ventral curvature after proximal TIP hypospadias repair. J. Pediatr. Urol. 17, 222.e1–222.e5 (2020).
Rynja, S. P., de Jong, T. P., Bosch, J. L. & de Kort, L. M. Functional, cosmetic and psychosexual results in adult men who underwent hypospadias correction in childhood. J. Pediatr. Urol. 7, 504–515 (2011).
Sullivan, K. J. et al. Assessing quality of life of patients with hypospadias: a systematic review of validated patient-reported outcome instruments. J. Pediatr. Urol. 13, 19–27 (2017).
Chertin, B. et al. Objective and subjective sexual outcomes in adult patients after hypospadias repair performed in childhood. J. Urol. 190, 1556–1560 (2013).
Örtqvist, L. et al. Long-term followup of men born with hypospadias: urological and cosmetic results. J. Urol. 193, 975–981 (2015).
Örtqvist, L. et al. Psychosocial outcome in adult men born with hypospadias. J. Pediatr. Urol. 13, 79.e1–79.e7 (2017).
Örtqvist, L. et al. Sexuality and fertility in men with hypospadias; improved outcome. Andrology 5, 286–293 (2017).
Andersson, M. et al. Psychosocial and sexual outcomes in adolescents following surgery for proximal hypospadias in childhood. J. Urol. 200, 1362–1370 (2018).
Andersson, M. et al. Urological results and patient satisfaction in adolescents after surgery for proximal hypospadias in childhood. J. Pediatr. Urol. 16, 660.e1–660.e8 (2020).
Tack, L. J. W. et al. Psychosexual outcome, sexual function, and long-term satisfaction of adolescent and young adult men after childhood hypospadias repair. J. Sex. Med. 17, 1665–1675 (2020).
Castagnetti, M. Childhood hypospadias repairs — do they stand the test of time? J. Urol. 193, 756–757 (2015).
Blanc, T. et al. Testicular function and physical outcome in young adult males diagnosed with idiopathic 46 XY disorders of sex development during childhood. Eur. J. Endocrinol. 165, 907–915 (2011).
Pasterski, V., Prentice, P. & Hughes, I. A. Consequences of the Chicago consensus on disorders of sex development (DSD): current practices in Europe. Arch. Dis. Child. 95, 618–623 (2010).
Bandini, M. et al. Prevalence, assessment and surgical correction of penile curvature in hypospadias patients treated at one European Referral Center: description of the technique and surgical outcomes. World J. Urol. 38, 2041–2048 (2020).
Menon, V. et al. Do adult men with untreated ventral penile curvature have adverse outcomes? J. Pediatr. Urol. 12, 31.e1–7 (2016).
Chung, E., Gillman, M., Rushton, D., Love, C. & Katz, D. Prevalence of penile curvature: a population-based cross-sectional study in metropolitan and rural cities in Australia. BJU Int. 122, 42–49 (2018).
Chen, J. Y., Hockenberry, M. S. & Lipshultz, L. I. Objective assessments of Peyronie’s disease. Sex. Med. Rev. 6, 438–445 (2018).
Villanueva, C. A. Ventral penile curvature estimation using an app. J. Pediatr. Urol. 16, 437.e1–437.e3 (2020).
Villanueva, C. A. Goniometer not better than unaided visual inspection at estimating ventral penile curvature on plastic models. J. Pediatr. Urol. 15, 628–633 (2019).
Nascimento, B. et al. Impact of camera deviation on penile curvature assessment using 2D pictures. J. Sex. Med. 15, 1638–1644 (2018).
Blanc, T. et al. Double-face preputial island flap revisited: is it a reliable one-stage repair for severe hypospadias?. World J. Urol. 39, 1613–1624 (2020).
Cimador, M. et al. Failed hypospadias in paediatric patients. Nat. Rev. Urol. 10, 657–666 (2013).
Cunha, G. R., Sinclair, A., Risbridger, G., Hutson, J. & Baskin, L. S. Current understanding of hypospadias: relevance of animal models. Nat. Rev. Urol. 12, 271–280 (2015).
Yuri, P. et al. The impact of COL1A1 and COL6A1 expression on hypospadias and penile curvature severity. BMC Urol. 20, 189 (2020).
Baskin, L. et al. Androgen and estrogen receptor expression in the developing human penis and clitoris. Differentiation 111, 41–59 (2020).
Koff, S. A. & Jayanthi, V. R. Preoperative treatment with human chorionic gonadotropin in infancy decreases the severity of proximal hypospadias and chordee. J. Urol. 162, 1435–1439 (1999).
Bagnara, V., Giammusso, B., Castagnetti, M., Esposito, C. & Bianchi, A. Distal hypospadias repair using the needle point bipolar cutting-coagulation forceps. J. Pediatr. Urol. 16, 69.e1–69.e5 (2020).
Acimi, S. & Acimi, M. A. Can we preserve the urethral plate in proximal hypospadias repair? Ann. Plast. Surg. 79, 68–72 (2017).
Weber, B. A. et al. Impact of penile degloving and proximal ventral dissection on curvature correction in children with proximal hypospadias. Can. Urol. Assoc. J. 8, 424–427 (2014).
Thiry, S., Gorduza, D. & Mouriquand, P. Urethral advancement in hypospadias with a distal division of the corpus spongiosum: outcome in 158 cases. J. Pediatr. Urol. 10, 451–454 (2014).
Kuo, T. L., Venugopal, S., Inman, R. D. & Chapple, C. R. Surgical tips and tricks during urethroplasty for bulbar urethral strictures focusing on accurate localisation of the stricture: results from a tertiary centre. Eur. Urol. 67, 764–770 (2015).
Snodgrass, W. T., Granberg, C. & Bush, N. C. Urethral strictures following urethral plate and proximal urethral elevation during proximal TIP hypospadias repair. J. Pediatr. Urol. 9, 990–994 (2013).
Castagnetti, M., Zhapa, E. & Rigamonti, W. Primary severe hypospadias: comparison of reoperation rates and parental perception of urinary symptoms and cosmetic outcomes among 4 repairs. J. Urol. 189, 1508–1513 (2013).
McNamara, E. R. et al. Management of proximal hypospadias with 2-stage repair: 20-year experience. J. Urol. 194, 1080–1085 (2015).
Long, C. J. et al. Intermediate-term followup of proximal hypospadias repair reveals high complication rate. J. Urol. 197, 852–858 (2017).
Stanasel, I. et al. Complications following staged hypospadias repair using transposed preputial skin flaps. J. Urol. 194, 512–516 (2015).
Badawy, H. et al. Staged repair of proximal hypospadias: reporting outcome of staged tubularized autograft repair (STAG). J. Pediatr. Surg. 55, 2710–2716 (2020).
Pfistermüller, K. L., Manoharan, S., Desai, D. & Cuckow, P. M. Two-stage hypospadias repair with a free graft for severe primary and revision hypospadias: a single surgeon’s experience with long-term follow-up. J. Pediatr. Urol. 13, 35.e1–35.e7 (2017).
Baskin, L. S., Erol, A., Li, Y. W. & Liu, W. H. Anatomy of the neurovascular bundle: is safe mobilization possible? J. Urol. 164, 977–980 (2000).
Seveso, M. et al. Surgical correction of Peyronie’s disease via tunica albuginea plication: long-term follow-up. Andrology 6, 47–52 (2018).
Çayan, S. et al. Comparison of patient’s satisfaction and long-term results of 2 penile plication techniques: lessons learned from 387 patients with penile curvature. Urology 129, 106–112 (2019).
Bagnara, V. et al. Giammusso corporoplasty for the treatment of isolated congenital ventral penile curvature: results and long-term follow-up. Andrologia 53, e13934. (2020).
Abosena, W., Talab, S. S. & Hanna, M. K. Recurrent chordee in 59 adolescents and young adults following childhood hypospadias repair. J. Pediatr. Urol. 16, 162.e1–162.e5 (2020).
Rigamonti, W. & Castagnetti, M. Onlay on albuginea: modified onlay preputial island flap urethroplasty for single-stage repair of primary severe hypospadias requiring urethral plate division. Urology 77, 1498–1502 (2011).
Macedo, A., Liguori, R., Garrone, G. & Ottoni, S. One-stage complex primary hypospadia repair combining buccal mucosa graft, preputial flap and tunical vaginalis flap (the three-in-one technique). J. Pediatr. Urol. 7, 76.e1–2 (2011).
Yang, T. et al. Byars two-stage procedure for hypospadias after urethral plate transection. J. Pediatr. Urol. 10, 1133–1137 (2014).
Tiryaki, S. et al. Unexpected outcome of a modification of Bracka repair for proximal hypospadias: high incidence of diverticula with flaps. J. Pediatr. Urol. 12, 395.e1–395.e6 (2016).
Faure, A., Bouty, A., Nyo, Y. L., O’Brien, M. & Heloury, Y. Two-stage graft urethroplasty for proximal and complicated hypospadias in children: a retrospective study. J. Pediatr. Urol. 12, 286.e1–286.e7 (2016).
Altarac, S., Papeš, D. & Bracka, A. Two-stage hypospadias repair with inner preputial layer Wolfe graft (Aivar Bracka repair). BJU Int. 110, 460–473 (2012).
Huang, Y. et al. One-stage repair of proximal hypospadias with severe chordee by in situ tubularization of the transverse preputial island flap. J. Pediatr. Urol. 13, 296–299 (2017).
Daboos, M., Helal, A. A. & Salama, A. Five years’ experience of double faced tubularized preputial flap for penoscrotal hypospadias repair in pediatrics. J. Pediatr. Urol. 16, 673.e1–673.e7 (2020).
Cui, X. et al. Clinical efficacy of transverse preputial island flap urethroplasty for single-stage correction of proximal hypospadias: a single-centre experience in Chinese patients. BMC Urol. 20, 118 (2020).
Badawy, H., Orabi, S., Hanno, A. & Abdelhamid, H. Posterior hypospadias: evaluation of a paradigm shift from single to staged repair. J. Pediatr. Urol. 14, 28.e1–28.e8 (2018).
Castagnetti, M. & El-Ghoneimi, A. The influence of perioperative factors on primary severe hypospadias repair. Nat. Rev. Urol. 8, 198–206 (2011).
Rynja, S. P., de Jong, T. P. V. M., Bosch, J. L. H. R. & de Kort, L. M. O. Proximal hypospadias treated with a transverse preputial island tube: long-term functional, sexual, and cosmetic outcomes. BJU Int. 122, 463–471 (2018).
Hueber, P. A. et al. Long-term functional outcomes after penoscrotal hypospadias repair: a retrospective comparative study of proximal TIP, Onlay, and Duckett. J. Pediatr. Urol. 12, 198.e1–6 (2016).
Snodgrass, W. T. Flap versus graft 2-stage repair of severe hypospadias with chordee. J. Urol. 193, 760–761 (2015).
Haxhirexha, K. N., Castagnetti, M., Rigamonti, W. & Manzoni, G. A. Two-stage repair in hypospadias. Indian. J. Urol. 24, 226–232 (2008).
Morlacco, A., Gobbi, D., Esposito, C. & Castagnetti, M. Edges-on-dartos: an easy way to improve graft performance in staged hypospadias repair. Urology 144, 245–248 (2020).
Badawy, H. & Fahmy, A. Single- vs. multi-stage repair of proximal hypospadias: the dilemma continues. Arab. J. Urol. 11, 174–181 (2013).
Dason, S., Wong, N. & Braga, L. H. The contemporary role of 1 vs. 2-stage repair for proximal hypospadias. Transl. Androl. Urol. 3, 347–358 (2014).
Author information
Authors and Affiliations
Contributions
M.C. researched data for the article. Both authors made substantial contributions to discussion of content, wrote the article, and reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer reviewer information
Nature Reviews Urology thanks Agneta Nordenskjold and Anne-Francoise Spinoit for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Andle Meter 360: https://apps.apple.com/us/app/angle-metre-360/id1393860479
Angles in Photo: https://apps.apple.com/sg/app/angles-in-photo/id974550003
Bonesetter Angle: https://apps.apple.com/us/app/drgoniometer/id362356791
DrGoniometer: https://apps.apple.com/ge/app/bonesetter-angle/id1517018787
Photoblend Pro: https://apps.apple.com/us/app/photoblend-pro-blend-your-pics/id734258457
Rights and permissions
About this article
Cite this article
Castagnetti, M., El-Ghoneimi, A. Surgical management of primary severe hypospadias in children: an update focusing on penile curvature. Nat Rev Urol 19, 147–160 (2022). https://doi.org/10.1038/s41585-021-00555-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-021-00555-0
This article is cited by
-
Unaided visual assessment of ventral curvature during hypospadias repair is inferior to objective measurement using app goniometry
Pediatric Surgery International (2023)
-
Glans dehiscence after severe hypospadias repair. Is it a real complication? Clues from a study in post-pubertal patients
Pediatric Surgery International (2023)