Abstract
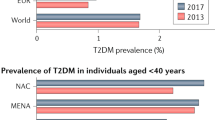
The incidence and prevalence of youth-onset type 2 diabetes mellitus (T2DM) and its complications are increasing worldwide. Youth-onset T2DM has been reported in all racial and ethnic groups, but Indigenous peoples and people of colour are disproportionately affected. People with youth-onset T2DM often have a more aggressive clinical course than those with adult-onset T2DM or those with type 1 diabetes mellitus. Moreover, the available treatment options for children and adolescents with T2DM are more limited than for adult patients. Intermediate complications of youth-onset T2DM, such as increased albuminuria, often develop in late childhood or early adulthood, and end-stage complications, including kidney failure, develop in mid-life. The increasing frequency, earlier onset and greater severity of childhood obesity in the past 50 years together with increasingly sedentary lifestyles and an increasing frequency of intrauterine exposure to diabetes are important drivers of the epidemic of youth-onset T2DM. The particularly high risk of the disease in historically disadvantaged populations suggests an important contribution of social and environmental factors, including limited access to high-quality health care, healthy food choices and opportunities for physical activity as well as exposure to stressors including systemic racism and environmental pollutants. Understanding the mechanisms that underlie the development and aggressive clinical course of youth-onset T2DM is key to identifying successful prevention and management strategies.
Key points
-
The incidence and prevalence of youth-onset type 2 diabetes mellitus (T2DM) are increasing worldwide; the disease has been reported in all racial and ethnic groups, but Indigenous peoples and people of colour are disproportionately affected.
-
Important drivers of the epidemic of youth-onset T2DM include the increasing frequency, severity and earlier onset of childhood obesity, the increasing frequency of intrauterine exposure to diabetes, sedentary lifestyles, structural racism and other psychosocial factors.
-
Individuals who develop T2DM during childhood or adolescence often have a more aggressive clinical course than those with type 1 diabetes mellitus or those who develop T2DM in adulthood.
-
Youth-onset T2DM has a more extreme metabolic phenotype than adult-onset T2DM, with greater insulin resistance and more rapid deterioration of β-cell function; intermediate complications often develop in late childhood or early adulthood, and end-stage complications, including kidney failure, develop in mid-life.
-
Owing to limited efficacy and safety data, several drugs that are available for the treatment of adults with T2DM have not been approved for the treatment of youth, which reduces the options that are available to normalize glycaemia in these patients.
-
Managing youth-onset T2DM and mitigating the risk of microvascular and macrovascular complications require the development of more effective interventions as well as strategies to overcome barriers to adherence that are not typically encountered in adult patients.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Fajans, S. S. & Conn, J. W. Tolbutamide-induced improvement in carbohydrate tolerance of young people with mild diabetes mellitus. Diabetes 9, 83–88 (1960).
Burkeholder, J. N., Pickens, J. M. & Womack, W. N. Oral glucose tolerance test in siblings of children with diabetes mellitus. Diabetes 16, 156–160 (1967).
Martin, M. M. & Martin, A. L. Obesity, hyperinsulinism, and diabetes mellitus in childhood. J. Pediatr. 82, 192–201 (1973).
Drash, A. Relationship between diabetes mellitus and obesity in the child. Metabolism 22, 337–344 (1973).
Deschamps, I., Giron, B. J. & Lestradet, H. Blood glucose, insulin, and free fatty acid levels during oral glucose tolerance tests in 158 obese children. Diabetes 26, 89–93 (1977).
Pinhas-Hamiel, O. et al. Increased incidence of non-insulin-dependent diabetes mellitus among adolescents. J. Pediatrics 128, 608–615 (1996).
Dean, H. J., Mundy, R. L. & Moffatt, M. Non-insulin-dependent diabetes mellitus in Indian children in Manitoba. Can. Med. Assoc. J. 147, 52–57 (1992).
Kitagawa, T., Owada, M., Urakami, T. & Yamauchi, K. Increased incidence of non-insulin dependent diabetes mellitus among Japanese schoolchildren correlates with an increased intake of animal protein and fat. Clin. Pediatr. 37, 111–115 (1998).
Pihoker, C., Scott, C. R., Lensing, S. Y., Cradock, M. M. & Smith, J. Non-insulin dependent diabetes mellitus in African-American youths of Arkansas. Clin. Pediatr. 37, 97–102 (1998).
Harris, S. B., Perkins, B. A. & Whalen-Brough, E. Non-insulin-dependent diabetes mellitus among First Nations children. New entity among First Nations people of north western Ontario. Can. Fam. Physician 42, 869–876 (1996).
Neufeld, N. D., Raffel, L. J., Landon, C., Chen, Y. D. & Vadheim, C. M. Early presentation of type 2 diabetes in Mexican-American youth. Diabetes Care 21, 80–86 (1998).
Savage, P. J., Bennett, P. H., Senter, R. G. & Miller, M. High prevalence of diabetes in young Pima Indians: evidence of phenotypic variation in a genetically isolated population. Diabetes 28, 937–942 (1979).
Kadiki, O. A., Reddy, M. R. & Marzouk, A. A. Incidence of insulin-dependent diabetes (IDDM) and non-insulin-dependent diabetes (NIDDM) (0–34 years at onset) in Benghazi, Libya. Diabetes Res. Clin. Pract. 32, 165–173 (1996).
Pinhas-Hamiel, O. & Zeitler, P. The global spread of type 2 diabetes mellitus in children and adolescents. J. Pediatr. 146, 693–700 (2005).
Telo, G. H., Cureau, F. V., Szklo, M., Bloch, K. V. & Schaan, B. D. Prevalence of type 2 diabetes among adolescents in Brazil: findings from study of cardiovascular risk in adolescents (ERICA). Pediatr. Diabetes 20, 389–396 (2019).
Fagot-Campagna, A. et al. Type 2 diabetes among North American children and adolescents: an epidemiologic review and a public health perspective. J. Pediatrics 136, 664–672 (2000).
American Diabetes Association. Type 2 diabetes in children and adolescents. Diabetes Care 23, 381–389 (2000).
Mayer-Davis, E. J. et al. Incidence trends of type 1 and type 2 diabetes among youths, 2002–2012. N. Engl. J. Med. 376, 1419–1429 (2017). The incidence of youth-onset T1DM and T2DM increased significantly between 2002 and 2012, particularly among minority racial and ethnic groups.
Lawrence, J. M. et al. Trends in prevalence of type 1 and type 2 diabetes in children and adolescents in the US, 2001–2017. JAMA 326, 717–727 (2021).
TODAY Study Group et al. Long-term complications in youth-onset type 2 diabetes. N. Engl. J. Med. 385, 416–426 (2021). This study reports a high burden of microvascular and macrovascular complications in youth with T2DM transitioning to adulthood.
Dabelea, D. et al. Association of type 1 diabetes vs type 2 diabetes diagnosed during childhood and adolescence with complications during teenage years and young adulthood. JAMA 317, 825–835 (2017).
Diabetes Canada Clinical Practice Guidelines Expert Committee et al. Type 2 diabetes and indigenous peoples. Can. J. Diabetes 42, S296–S306 (2018).
Nadeau, K. J. et al. Youth-onset type 2 diabetes consensus report: current status, challenges, and priorities. Diabetes Care 39, 1635–1642 (2016).
Fagot-Campagna, A. et al. Diabetes, impaired fasting glucose, and elevated HbA1c in U.S. adolescents: the Third National Health and Nutrition Examination Survey. Diabetes Care 24, 834–837 (2001).
Demmer, R. T., Zuk, A. M., Rosenbaum, M. & Desvarieux, M. Prevalence of diagnosed and undiagnosed type 2 diabetes mellitus among US adolescents: results from the continuous NHANES, 1999-2010. Am. J. Epidemiol. 178, 1106–1113 (2013).
Bullard, K. M. et al. Prevalence of diagnosed diabetes in adults by diabetes type-United States, 2016. Morb. Mortal. Wkly Rep. 67, 359–361 (2018).
Bennett, P. H., Burch, T. A. & Miller, M. Diabetes mellitus in American (Pima) Indians. Lancet 2, 125–128 (1971).
Katzeff, H. L., Savage, P. J., Barclay-White, B., Nagulesparan, M. & Bennett, P. H. C-peptide measurement in the differentiation of type 1 (insulin-dependent) and type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia 28, 264–268 (1985).
Knowler, W. C., Bennett, P. H., Bottazzo, G. F. & Doniach, D. Islet cell antibodies and diabetes mellitus in Pima Indians. Diabetologia 17, 161–164 (1979).
Dabelea, D., Palmer, J. P., Bennett, P. H., Pettitt, D. J. & Knowler, W. C. Absence of glutamic acid decarboxylase antibodies in Pima Indian children with diabetes mellitus. Diabetologia 42, 1265–1266 (1999).
Janssen, R. C., Bogardus, C., Takeda, J., Knowler, W. C. & Thompson, D. B. Linkage analysis of acute insulin secretion with GLUT2 and glucokinase in Pima Indians and the identification of a missense mutation in GLUT2. Diabetes 43, 558–563 (1994).
Muller, Y. L. et al. Variants in hepatocyte nuclear factor 4alpha are modestly associated with type 2 diabetes in Pima Indians. Diabetes 54, 3035–3039 (2005).
Dabelea, D. et al. Increasing prevalence of type II diabetes in American Indian children. Diabetologia 41, 904–910 (1998).
Pettitt, D. J., Baird, H. R., Aleck, K. A., Bennett, P. H. & Knowler, W. C. Excessive obesity in offspring of Pima Indian women with diabetes during pregnancy. N. Engl. J. Med. 308, 242–245 (1983).
Vijayakumar, P. et al. Secular changes in physical growth and obesity among southwestern American Indian children over four decades. Pediatr. Obes. 13, 94–102 (2018).
Tanamas, S. K. et al. Effect of severe obesity in childhood and adolescence on risk of type 2 diabetes in youth and early adulthood in an American Indian population. Pediatr. Diabetes 19, 622–629 (2018).
Amed, S. et al. Type 2 diabetes, medication-induced diabetes, and monogenic diabetes in Canadian children: a prospective national surveillance study. Diabetes Care 33, 786–791 (2010).
Young, T. K., McIntyre, L. L., Dooley, J. & Rodriguez, J. Epidemiologic features of diabetes mellitus among Indians in northwestern Ontario and northeastern Manitoba. Can. Med. Assoc. J. 132, 793–797 (1985).
Green, C., Blanchard, J. F., Young, T. K. & Griffith, J. The epidemiology of diabetes in the Manitoba-registered First Nation population: current patterns and comparative trends. Diabetes Care 26, 1993–1998 (2003).
Young, T. K., Reading, J., Elias, B. & O’Neil, J. D. Type 2 diabetes mellitus in Canada’s first nations: status of an epidemic in progress. CMAJ 163, 561–566 (2000).
Turin, T. C. et al. Lifetime risk of diabetes among First Nations and non-First Nations people. CMAJ 188, 1147–1153 (2016).
Albisser, A. M., Harris, R. I., Sakkal, S., Parson, I. D. & Chao, S. C. Diabetes intervention in the information age. Med. Inf. 21, 297–316 (1996).
Shulman, R. et al. Prevalence, incidence and outcomes of diabetes in Ontario First Nations children: a longitudinal population-based cohort study. CMAJ Open 8, E48–E55 (2020).
Dart, A. et al. Screening for kidney disease in Indigenous Canadian children: the FINISHED screen, triage and treat program. Paediatr. Child. Health 23, e134–e142 (2018).
Shulman, R., Miller, F. A., Stukel, T. A., Daneman, D. & Guttmann, A. Resources and population served: a description of the Ontario Paediatric Diabetes Network. CMAJ Open 4, E141–E146 (2016).
Lynch, J. L. et al. Country-specific prevalence and incidence of youth-onset type 2 diabetes: a narrative literature review. Ann. Nutr. Metab. 76, 289–296 (2020).
Haines, L., Wan, K. C., Lynn, R., Barrett, T. G. & Shield, J. P. Rising incidence of type 2 diabetes in children in the U.K. Diabetes Care 30, 1097–1101 (2007).
Candler, T. P. et al. Continuing rise of type 2 diabetes incidence in children and young people in the UK. Diabet. Med. 35, 737–744 (2018).
de Almeida-Pititto, B. et al. Type 2 diabetes in Brazil: epidemiology and management. Diabetes Metab. Syndr. Obes. 8, 17–28 (2015).
Singh, R., Shaw, J. & Zimmet, P. Epidemiology of childhood type 2 diabetes in the developing world. Pediatr. Diabetes 5, 154–168 (2004).
Muthuri, S. K. et al. Evidence of an overweight/obesity transition among school-aged children and youth in sub-Saharan Africa: a systematic review. PLoS ONE 9, e92846 (2014).
Kim, J. H. & Lim, J. S. Trends of diabetes and prediabetes prevalence among Korean Adolescents from 2007 to 2018. J. Korean Med. Sci. 36, e112 (2021).
Wang, Z. et al. Prevalence and risk factors of impaired fasting glucose and diabetes among Chinese children and adolescents: a national observational study. Br. J. Nutr. 120, 813–819 (2018).
Fu, J. F. et al. Status and trends of diabetes in Chinese children: analysis of data from 14 medical centers. World J. Pediatr. 9, 127–134 (2013).
Urakami, T. Screening of childhood type 2 diabetes in Japan. Diabetes Res. Clin. Pract. 120, https://doi.org/10.1016/s0168-8227(16)30891-9 (2016).
Wei, J. N. et al. National surveillance for type 2 diabetes mellitus in Taiwanese children. JAMA 290, 1345–1350 (2003).
Jensen, E. T. et al. Comparison of the incidence of diabetes in United States and Indian youth: an international harmonization of youth diabetes registries. Pediatr. Diabetes 22, 8–14 (2021).
Stone, M., Baker, A. & Maple Brown, L. Diabetes in young people in the Top End of the Northern Territory. J. Paediatr. Child. Health 49, 976–979 (2013).
Titmuss, A. et al. Youth-onset type 2 diabetes among First Nations young people in northern Australia: a retrospective, cross-sectional study. Lancet Diabetes Endocrinol. 10, 11–13 (2022).
Haynes, A., Kalic, R., Cooper, M., Hewitt, J. K. & Davis, E. A. Increasing incidence of type 2 diabetes in Indigenous and non-Indigenous children in Western Australia, 1990–2012. Med. J. Aust. 204, 303 (2016).
Te Whatu Ora. Virtual Diabetes Register and web tool. https://www.tewhatuora.govt.nz/our-health-system/digital-health/virtual-diabetes-tool/ (2020).
Assady S, R. R., Frishberg Y. in Brenner and Rector’s The Kidney (Tenth Edition). Vol. 78 (eds Rector Brenner, F. C. et al.) 2517–2545 (Elsevier, 2018).
Ali, B. A., Abdallah, S. T., Abdallah, A. M. & Hussein, M. M. The frequency of type 2 diabetes mellitus among diabetic children in El Minia Governorate, Egypt. Sultan Qaboos Univ. Med. J. 13, 399–403 (2013).
Moadab, M. H., Kelishadi, R., Hashemipour, M., Amini, M. & Poursafa, P. The prevalence of impaired fasting glucose and type 2 diabetes in a population-based sample of overweight/obese children in the Middle East. Pediatr. Diabetes 11, 101–106 (2010).
Mirbolouk, M. et al. Incidence and predictors of early adulthood pre-diabetes/type 2 diabetes, among Iranian adolescents: the Tehran Lipid and Glucose Study. Pediatr. Diabetes 17, 608–616 (2016).
Alsaffar, Y., Hussain, A. M. A. & Selman, N. A. Prevalence of type 2 diabetes in pediatrics and adolescents newly diagnosed with diabetes in Babylon Governorate, Iraq. AVFT 39, 839–845 (2020).
Zuckerman Levin, N. et al. Youth-onset type 2 diabetes in Israel: a national cohort. Pediatr. Diabetes 23, 649–659 (2022).
Meyerovitch, J., Zlotnik, M., Yackobovitch-Gavan, M., Phillip, M. & Shalitin, S. Real-life glycemic control in children with type 2 diabetes: a population-based study. J. Pediatr. 188, 173–180.e171 (2017).
Al-Kandari, H. et al. Incidence of type 2 diabetes in Kuwaiti children and adolescents: results from the childhood-onset diabetes electronic registry (CODeR). Front. Endocrinol. 10, 836 (2019).
Moussa, M. A. et al. Prevalence of type 2 diabetes mellitus among Kuwaiti children and adolescents. Med. Princ. Pract. 17, 270–275 (2008).
Salameh, P. & Barbour, B. Pattern of obesity and associated diabetes in Lebanese adolescents: a pilot study. East. Mediterr. Health J. 17, 226–230 (2011).
Agroiya, P. & Alrawahi, A. H. Pediatric diabetic retinopathy: experience of a tertiary hospital in Oman. Middle East. Afr. J. Ophthalmol. 26, 189–195 (2019).
Haris, B. et al. Epidemiology, genetic landscape and classification of childhood diabetes mellitus in the State of Qatar. J. Diabetes Investig. https://doi.org/10.1111/jdi.13610 (2021).
Alyafei, F. et al. Prevalence of beta-cell antibodies and associated autoimmune diseases in children and adolescents with type 1 diabetes (T1DM) versus type 2 diabetes (T2DM) in Qatar. Acta Biomed. 89, 32–39 (2018).
Al-Agha, A., Ocheltree, A. & Shata, N. Prevalence of hyperinsulinism, type 2 diabetes mellitus and metabolic syndrome among Saudi overweight and obese pediatric patients. Minerva Pediatr. 64, 623–631 (2012).
Al-Rubeaan, K. National surveillance for type 1, type 2 diabetes and prediabetes among children and adolescents: a population-based study (SAUDI-DM). J. Epidemiol. Community Health 69, 1045–1051 (2015).
Braham, R. et al. Double diabetes in Saudi Arabia: a new entity or an underestimated condition? World J. Diabetes 7, 621–626 (2016).
Haliloglu, B. et al. The distribution of different types of diabetes in childhood: a single center experience. J. Clin. Res. Pediatr. Endocrinol. 10, 125–130 (2018).
Hatun, S. et al. Characteristics of Turkish children with type 2 diabetes at onset: a multicentre, cross-sectional study. Diabet. Med. 36, 1243–1250 (2019).
Al Amiri, E. et al. The prevalence, risk factors, and screening measure for prediabetes and diabetes among Emirati overweight/obese children and adolescents. BMC Public Health 15, 1298–1298 (2015).
Punnose, J., Agarwal, M. M. & Bin-Uthman, S. Type 2 diabetes mellitus among children and adolescents in Al-Ain: a case series. East. Mediterr. Health J. 11, 788–797 (2005).
Atef, Z., Al-Ghazaly, J. & M, B. Prediabetes and type 2 diabetes among Yemeni adolescents. Eur. J. Biomed. Pharm. Sci. 5, 28–34 (2018).
International Diabetes Federation. IDF Diabetes Atlas 10th edn (International Diabetes Federation, 2021).
Elkum, N., Al-Arouj, M., Sharifi, M., Shaltout, A. & Bennakhi, A. Prevalence of childhood obesity in the state of Kuwait. Pediatr. Obes. 11, e30–e34 (2016).
AlBlooshi, A. et al. Increasing obesity rates in school children in United Arab Emirates. Obes. Sci. Pract. 2, 196–202 (2016).
Hamman, R. F. et al. The SEARCH for Diabetes in Youth study: rationale, findings, and future directions. Diabetes Care 37, 3336–3344 (2014).
SEARCH Study Group. SEARCH for Diabetes in Youth: a multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Control. Clin. Trials 25, 458–471 (2004).
Divers, J. et al. Trends in incidence of type 1 and type 2 diabetes among youths — selected counties and Indian reservations, United States, 2002–2015. MMWR Morb. Mortal. Wkly Rep. 69, 161–165 (2020).
Hales, C. M., Carroll, M. D., Fryer, C. D. & Ogden, C. L. Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS Data Brief, 1–8 (2017).
Ogden, C. L. et al. Trends in obesity prevalence by race and hispanic origin-1999–2000 to 2017–2018. JAMA 324, 1208–1210 (2020).
CDC. Prevalence of diagnosed diabetes. https://www.cdc.gov/diabetes/data/statistics-report/diagnosed-diabetes.html (2022).
Dabelea, D. et al. Association of intrauterine exposure to maternal diabetes and obesity with type 2 diabetes in youth: the SEARCH case-control study. Diabetes Care 31, 1422–1426 (2008).
Mayer-Davis, E. J. et al. Breast-feeding and type 2 diabetes in the youth of three ethnic groups: the SEARCH for Diabetes in Youth case-control study. Diabetes Care 31, 470–475 (2008).
Fernandez-Twinn, D. S., Hjort, L., Novakovic, B., Ozanne, S. E. & Saffery, R. Intrauterine programming of obesity and type 2 diabetes. Diabetologia 62, 1789–1801 (2019).
Navas-Acien, A., Silbergeld, E. K., Pastor-Barriuso, R. & Guallar, E. Arsenic exposure and prevalence of type 2 diabetes in US adults. JAMA 300, 814–822 (2008).
Maull, E. A. et al. Evaluation of the association between arsenic and diabetes: a National Toxicology Program workshop review. Environ. Health Perspect. 120, 1658–1670 (2012).
Liese, A. D. et al. Neighborhood characteristics, food deserts, rurality, and type 2 diabetes in youth: findings from a case-control study. Health Place. 50, 81–88 (2018).
Findholt, N. E., Michael, Y. L., Davis, M. M. & Brogoitti, V. W. Environmental influences on children’s physical activity and diets in rural oregon: results of a youth photovoice project. Online J. Rural. Nurs. Health Care 10, 11–20 (2010).
Zhang, X. et al. Neighborhood commuting environment and obesity in the United States: an urban-rural stratified multilevel analysis. Prev. Med. 59, 31–36 (2014).
TODAY Study Group et al. A clinical trial to maintain glycemic control in youth with type 2 diabetes. N. Engl. J. Med. 366, 2247–2256 (2012). This trial shows high rates of glycaemic failure irrespective of treatment group (metformin versus metformin plus lifestyle changes versus metformin plus rosiglitazone).
Maahs, D. M. et al. Higher prevalence of elevated albumin excretion in youth with type 2 than type 1 diabetes: the SEARCH for Diabetes in Youth study. Diabetes care 30, 2593–2598 (2007).
Pavkov, M. E. et al. Effect of youth-onset type 2 diabetes mellitus on incidence of end-stage renal disease and mortality in young and middle-aged Pima Indians. JAMA 296, 421–426 (2006). This study reports a 5-fold greater risk of diabetic kidney failure and a 2-fold greater risk of death in mid-life (aged 25–54 years) among Pima Indians with youth-onset compared with older-onset T2DM.
Sellers, E. A. C. et al. Persistent albuminuria in children with type 2 diabetes: a Canadian Paediatric Surveillance Program study. J. Pediatr. 168, 112–117 (2016).
Cioana, M. et al. Prevalence of hypertension and albuminuria in pediatric type 2 diabetes: a systematic review and meta-analysis. JAMA Netw. Open. 4, e216069 (2021).
Dart, A. B., Sellers, E. A. & Dean, H. J. Kidney disease and youth onset type 2 diabetes: considerations for the general practitioner. Int. J. Pediatr. 2012, 237360 (2012).
Wang, Z. & Hoy, W. E. Remaining lifetime risk for developing end stage renal disease among Australian aboriginal people with diabetes. Diabetes Res. Clin. Pract. 103, e24–e26 (2014).
Krakoff, J. et al. Incidence of retinopathy and nephropathy in youth-onset compared with adult-onset type 2 diabetes. Diabetes Care 26, 76–81 (2003).
Looker, H. C. et al. Structural lesions on kidney biopsy in youth-onset and adult-onset type 2 diabetes. Diabetes Care 45, 436–443 (2022). More severe structural lesions are observed in kidney biopsy samples from Pima Indians with youth-onset T2DM than in those with adult-onset T2DM irrespective of age and diabetes duration.
Pavkov, M. E., Sievers, M. L., Knowler, W. C., Bennett, P. H. & Nelson, R. G. An explanation for the increase in heart disease mortality rates in diabetic Pima Indians: effect of renal replacement therapy. Diabetes Care 27, 1132–1136 (2004).
Nelson, R. G. et al. Pima Indian contributions to our understanding of diabetic kidney disease. Diabetes 70, 1603–1616 (2021).
Koye, D. N. et al. Trends in incidence of ESKD in people with type 1 and type 2 diabetes in Australia, 2002-2013. Am. J. Kidney Dis. 73, 300–308 (2019).
Middleton, T. L. et al. Young adult onset type 2 diabetes versus type 1 diabetes: progression to and survival on renal replacement therapy. J. Diabetes Complicat. 35, 108023 (2021).
Shah, A. S. et al. A cross sectional study to compare cardiac structure and diastolic function in adolescents and young adults with youth-onset type 1 and type 2 diabetes: the SEARCH for Diabetes in Youth Study. Cardiovasc. Diabetol. 20, 136 (2021).
Lawrence, J. M. et al. Demographic correlates of short-term mortality among youth and young adults with youth-onset diabetes diagnosed from 2002 to 2015: the SEARCH for Diabetes in Youth Study. Diabetes Care 44, 2691–2698 (2021).
Constantino, M. I. et al. Long-term complications and mortality in young-onset diabetes: type 2 diabetes is more hazardous and lethal than type 1 diabetes. Diabetes Care 36, 3863–3869 (2013).
Levitt Katz, L. et al. Alterations in left ventricular, left atrial, and right ventricular structure and function to cardiovascular risk factors in adolescents with type 2 diabetes participating in the TODAY clinical trial. Pediatr. Diabetes 16, 39–47 (2015).
Group, T. S. Longitudinal changes in cardiac structure and function from adolescence to young adulthood in participants with type 2 diabetes mellitus: the TODAY follow-up study. Circ. Heart Fail. 13, e006685 (2020).
Lynch, S. K. & Abramoff, M. D. Diabetic retinopathy is a neurodegenerative disorder. Vis. Res. 139, 101–107 (2017).
White, N. H. et al. Beneficial effects of intensive therapy of diabetes during adolescence: outcomes after the conclusion of the diabetes control and complications trial (DCCT). J. Pediatr. 139, 804–812 (2001).
Rajalakshmi, R. et al. Prevalence and risk factors for diabetic retinopathy in Asian Indians with young onset type 1 and type 2 diabetes. J. Diabetes Complicat. 28, 291–297 (2014).
Bai, P., Barkmeier, A. J., Hodge, D. O. & Mohney, B. G. Ocular sequelae in a population-based cohort of youth diagnosed with diabetes during a 50-year period. JAMA Ophthalmol. 140, 51–57 (2022).
Wang, S. Y., Andrews, C. A., Herman, W. H., Gardner, T. W. & Stein, J. D. Incidence and risk factors for developing diabetic retinopathy among youths with type 1 or type 2 diabetes throughout the United States. Ophthalmology 124, 424–430 (2017).
Mayer-Davis, E. J. et al. Diabetic retinopathy in the SEARCH for Diabetes in Youth cohort: a pilot study. Diabet. Med. 29, 1148–1152 (2012).
Unnikrishnan, R. et al. Younger-onset versus older-onset type 2 diabetes: clinical profile and complications. J. Diabetes Complicat. 31, 971–975 (2017).
Zhang, X. et al. Prevalence of diabetic retinopathy in the United States, 2005–2008. JAMA 304, 649–656 (2010).
Akinci, G., Savelieff, M. G., Gallagher, G., Callaghan, B. C. & Feldman, E. L. Diabetic neuropathy in children and youth: new and emerging risk factors. Pediatr. Diabetes 22, 132–147 (2021).
Dart, A. B. et al. Earlier onset of complications in youth with type 2 diabetes. Diabetes Care 37, 436–443 (2014).
He, J., Ryder, A. G., Li, S., Liu, W. & Zhu, X. Glycemic extremes are related to cognitive dysfunction in children with type 1 diabetes: a meta-analysis. J. Diabetes Investig. 9, 1342–1353 (2018).
Shapiro, A. L. B. et al. Cognitive function in adolescents and young adults with youth-onset type 1 versus type 2 diabetes: the SEARCH for Diabetes in Youth study. Diabetes Care 44, 1273–1280 (2021).
Nadeau, K. J., Klingensmith, G. & Zeitler, P. Type 2 diabetes in children is frequently associated with elevated alanine aminotransferase. J. Pediatr. Gastroenterol. Nutr. 41, 94–98 (2005).
Hudson, O. D., Nunez, M. & Shaibi, G. Q. Ethnicity and elevated liver transaminases among newly diagnosed children with type 2 diabetes. BMC Pediatr. 12, 174 (2012).
Weinstock, R. S. et al. Metabolic syndrome is common and persistent in youth-onset type 2 diabetes: results from the TODAY clinical trial. Obesity 23, 1357–1361 (2015).
Punthakee, Z. et al. Impact of rosiglitazone on body composition, hepatic fat, fatty acids, adipokines and glucose in persons with impaired fasting glucose or impaired glucose tolerance: a sub-study of the DREAM trial. Diabet. Med. 31, 1086–1092 (2014).
Virtanen, K. A. et al. Differential effects of rosiglitazone and metformin on adipose tissue distribution and glucose uptake in type 2 diabetic subjects. Diabetes 52, 283–290 (2003).
Iozzo, P. et al. Effects of metformin and rosiglitazone monotherapy on insulin-mediated hepatic glucose uptake and their relation to visceral fat in type 2 diabetes. Diabetes Care 26, 2069–2074 (2003).
Carey, D. G. et al. Effect of rosiglitazone on insulin sensitivity and body composition in type 2 diabetic patients [corrected]. Obes. Res. 10, 1008–1015 (2002).
Yokoyama, H. et al. High incidence of diabetic nephropathy in early-onset Japanese NIDDM patients. Risk analysis. Diabetes Care 21, 1080–1085 (1998).
Eppens, M. C. et al. Prevalence of diabetes complications in adolescents with type 2 compared with type 1 diabetes. Diabetes Care 29, 1300–1306 (2006).
Eppens, M. C. et al. Type 2 diabetes in youth from the Western Pacific region: glycaemic control, diabetes care and complications. Curr. Med. Res. Opin. 22, 1013–1020 (2006).
Dart, A. B. et al. A holistic approach to risk for early kidney injury in indigenous youth with type 2 diabetes: a proof of concept paper from the iCARE cohort. Can. J. Kidney Health Dis. 6, 2054358119838836 (2019).
Jaiswal, M. et al. Prevalence of and risk factors for diabetic peripheral neuropathy in youth with type 1 and type 2 diabetes: SEARCH for Diabetes in Youth study. Diabetes Care 40, 1226–1232 (2017).
Bjornstad, P. et al. Elevated serum uric acid is associated with greater risk for hypertension and diabetic kidney diseases in obese adolescents with type 2 diabetes: an observational analysis from the treatment options for type 2 diabetes in adolescents and youth (TODAY) study. Diabetes Care 42, 1120–1128 (2019).
Group, T. S. Retinopathy in youth with type 2 diabetes participating in the TODAY clinical trial. Diabetes Care 36, 1772–1774 (2013).
Carino, M. et al. Comparison of clinical and social characteristics of Canadian youth living with type 1 and type 2 diabetes. Can. J. diabetes 45, 428–435 (2021).
Kershnar, A. K. et al. Lipid abnormalities are prevalent in youth with type 1 and type 2 diabetes: the SEARCH for Diabetes in Youth study. J. Pediatr. 149, 314–319 (2006).
Rodriguez, B. L. et al. Prevalence of cardiovascular disease risk factors in U.S. children and adolescents with diabetes: the SEARCH for Diabetes in Youth study. Diabetes Care 29, 1891–1896 (2006).
Rodriguez, B. L. et al. Prevalence and correlates of elevated blood pressure in youth with diabetes mellitus: the SEARCH for Diabetes in Youth study. J. Pediatr. 157, 245–251.e241 (2010).
Albers, J. J. et al. Prevalence and determinants of elevated apolipoprotein B and dense low-density lipoprotein in youths with type 1 and type 2 diabetes. J. Clin. Endocrinol. Metab. 93, 735–742 (2008).
Jaiswal, M. et al. Cardiovascular autonomic neuropathy in adolescents and young adults with type 1 and type 2 diabetes: the SEARCH for Diabetes in Youth cohort study. Pediatr. Diabetes 19, 680–689 (2018).
Reynolds, K. et al. Prevalence of tobacco use and association between cardiometabolic risk factors and cigarette smoking in youth with type 1 or type 2 diabetes mellitus. J. Pediatr. 158, 594–601 e591 (2011).
Nanayakkara, N. et al. Age, age at diagnosis and diabetes duration are all associated with vascular complications in type 2 diabetes. J. Diabetes Complicat. 32, 279–290 (2018).
Zoungas, S. et al. Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes. Diabetologia 57, 2465–2474 (2014).
Huo, L. et al. Impact of age at diagnosis and duration of type 2 diabetes on mortality in Australia 1997-2011. Diabetologia 61, 1055–1063 (2018).
Yeap, B. B. et al. Diabetes, myocardial infarction and stroke are distinct and duration-dependent predictors of subsequent cardiovascular events and all-cause mortality in older men. J. Clin. Endocrinol. Metab. 100, 1038–1047 (2015).
Noh, M. et al. Impact of diabetes duration and degree of carotid artery stenosis on major adverse cardiovascular events: a single-center, retrospective, observational cohort study. Cardiovasc. Diabetol. 16, 74 (2017).
Al-Saeed, A. H. et al. An inverse relationship between age of type 2 diabetes onset and complication risk and mortality: the impact of youth-onset type 2 diabetes. Diabetes Care 39, 823–829 (2016).
Hu, C. et al. Association between age at diagnosis of type 2 diabetes and cardiovascular diseases: a nationwide, population-based, cohort study. Front. Endocrinol. 12, 717069 (2021).
Visaria, J. et al. Incidence and prevalence of microvascular and macrovascular diseases and all-cause mortality in type 2 diabetes mellitus: a 10-year study in a US commercially insured and Medicare Advantage population. Clin. Ther. 41, 1522–1536 e1521 (2019).
Hillier, T. A. & Pedula, K. L. Complications in young adults with early-onset type 2 diabetes: losing the relative protection of youth. Diabetes Care 26, 2999–3005 (2003).
Magliano, D. J. et al. Young-onset type 2 diabetes mellitus — implications for morbidity and mortality. Nat. Rev. Endocrinol. 16, 321–331 (2020).
Lascar, N. et al. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol. 6, 69–80 (2018).
Druet, C. et al. Characterization of insulin secretion and resistance in type 2 diabetes of adolescents. J. Clin. Endocrinol. Metab. 91, 401–404 (2006).
Mohan, V. et al. Associations of beta-cell function and insulin resistance with youth-onset type 2 diabetes and prediabetes among Asian Indians. Diabetes Technol. Ther. 15, 315–322 (2013).
Bacha, F. et al. Determinants of glycemic control in youth with type 2 diabetes at randomization in the TODAY study. Pediatr. Diabetes 13, 376–383 (2012).
Utzschneider, K. M. et al. Differential loss of beta-cell function in youth vs. adults following treatment withdrawal in the Restoring Insulin Secretion (RISE) study. Diabetes Res. Clin. Pract. 178, 108948 (2021).
RISE Consortium. Restoring Insulin Secretion (RISE): design of studies of beta-cell preservation in prediabetes and early type 2 diabetes across the life span Diabetes Care 37, 780–788 (2014).
Kahn, S. E. et al. Hyperglucagonemia does not explain the beta-cell hyperresponsiveness and insulin resistance in dysglycemic youth compared with adults: lessons from the RISE study. Diabetes Care 44, 1961–1969 (2021).
Sam, S. et al. Baseline predictors of glycemic worsening in youth and adults with impaired glucose tolerance or recently diagnosed type 2 diabetes in the Restoring Insulin Secretion (RISE) study. Diabetes Care 44, 1938–1947 (2021).
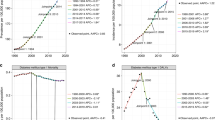
RISE Consortium. Metabolic contrasts between youth and adults with impaired glucose tolerance or recently diagnosed type 2 diabetes: I. Observations using the hyperglycemic clamp. Diabetes Care 41, 1696–1706 (2018). In comparison with adults with pre-diabetes and T2DM, youth with pre-diabetes and T2DM were more insulin resistant, had lower insulin clearance and, despite similar glycaemia, had much higher insulin secretion as assessed by hyperglycaemic clamp.
RISE Consortium. Metabolic contrasts between youth and adults with impaired glucose tolerance or recently diagnosed type 2 diabetes: II. Observations using the oral glucose tolerance test. Diabetes Care 41, 1707–1716 (2018).
Utzschneider, K. M. et al. β-Cells in youth with impaired glucose tolerance or early type 2 diabetes secrete more insulin and are more responsive than in adults. Pediatr. Diabetes 21, 1421–1429 (2020).
RISE Consortium. Effects of treatment of impaired glucose tolerance or recently diagnosed type 2 diabetes with metformin alone or in combination with insulin glargine on beta-cell function: comparison of responses in youth and adults. Diabetes 68, 1670–1680 (2019). More youth than adults had glycaemic worsening on treatment at month 12, and in adults, β-cell function improved during treatment whereas β-cell function deteriorated during treatment in youth.
Srinivasan, S. et al. The first genome-wide association study for type 2 diabetes in youth: the Progress in Diabetes Genetics in Youth (ProDiGY) consortium. Diabetes 70, 996–1005 (2021).
Jabar, F., Colatruglio, S., Sellers, E., Kroeker, K. & Wicklow, B. The next generation cohort: a description of a cohort at high risk for childhood onset type 2 diabetes. J. Dev. Orig. Health Dis. 10, 24–30 (2019).
Kriska, A. et al. Impact of lifestyle behavior change on glycemic control in youth with type 2 diabetes. Pediatr. Diabetes 19, 36–44 (2018).
Berkowitz, R. I. et al. Adherence to a lifestyle program for youth with type 2 diabetes and its association with treatment outcome in the TODAY clinical trial. Pediatr. Diabetes 19, 191–198 (2018).
Trief, P. M. et al. Medication adherence in young adults with youth-onset type 2 diabetes: iCount, an observational study. Diabetes Res. Clin. Pract. 184, 109216 (2022).
Anderson, B. J. et al. Depressive symptoms and quality of life in adolescents with type 2 diabetes: baseline data from the TODAY study. Diabetes Care 34, 2205–2207 (2011).
Copeland, K. C. et al. Characteristics of adolescents and youth with recent-onset type 2 diabetes: the TODAY cohort at baseline. J. Clin. Endocrinol. Metab. 96, 159–167 (2011).
Miller, J. L. & Silverstein, J. H. The treatment of type 2 diabetes mellitus in youth: which therapies? Treat. Endocrinol. 5, 201–210 (2006).
Yeung, R. O. et al. Metabolic profiles and treatment gaps in young-onset type 2 diabetes in Asia (the JADE programme): a cross-sectional study of a prospective cohort. Lancet Diabetes Endocrinol. 2, 935–943 (2014).
Ke, C. et al. Age at diagnosis, glycemic trajectories, and responses to oral glucose-lowering drugs in type 2 diabetes in Hong Kong: a population-based observational study. PLoS Med. 17, e1003316 (2020).
Group, T. S. Health care coverage and glycemic control in young adults with youth-onset type 2 diabetes: results from the TODAY2 study. Diabetes Care 43, 2469–2477 (2020).
Duke, N. N. Food insecurity and prediabetes among adolescents taking a school-based survey. Am. J. Health Behav. 45, 384–396 (2021).
Pulling Kuhn, A. et al. Home and neighborhood physical activity location availability among African American adolescent girls living in low-income, urban communities: associations with objectively measured physical activity. Int. J. Environ. Res. Public Health 18, 5003 (2021).
Kornides, M. L. et al. US adolescents at risk for not meeting physical activity recommendations by season. Pediatr. Res. 84, 50–56 (2018).
Kahn, J. A. et al. Patterns and determinants of physical activity in U.S. adolescents. J. Adolesc. Health 42, 369–377 (2008).
Gordon-Larsen, P., Adair, L. S. & Popkin, B. M. Ethnic differences in physical activity and inactivity patterns and overweight status. Obes. Res. 10, 141–149 (2002).
Hannon, J. C. Physical activity levels of overweight and nonoverweight high school students during physical education classes. J. Sch. Health 78, 425–431 (2008).
Simon, S. et al. Poor sleep is related to metabolic syndrome severity in adolescents with PCOS and obesity. J. Clin. Endocrinol. Metab. 105, e1827–e1834 (2020).
Simon, S. L., Higgins, J., Melanson, E., Wright, K. P. Jr & Nadeau, K. J. A model of adolescent sleep health and risk for type 2 diabetes. Curr. Diab Rep. 21, 4 (2021).
Simon, S. L. et al. Too late and not enough: school year sleep duration, timing, and circadian misalignment are associated with reduced insulin sensitivity in adolescents with overweight/obesity. J. Pediatr. 205, 257–264 e251 (2019).
Mokhlesi, B. et al. The association of sleep disturbances with glycemia and obesity in youth at risk for or with recently diagnosed type 2 diabetes. Pediatr. Diabetes 20, 1056–1063 (2019).
Grandner, M. A. et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep. Med. 11, 470–478 (2010).
Qureshi, F. et al. Childhood assets and cardiometabolic health in adolescence Pediatrics 143 e20182004 (2019).
Downs, C. A. & Faulkner, M. S. Toxic stress, inflammation and symptomatology of chronic complications in diabetes. World J. Diabetes 6, 554–565 (2015).
Shomaker, L. B. et al. Design of a randomized controlled trial to decrease depression and improve insulin sensitivity in adolescents: Mood and INsulin sensitivity to prevent Diabetes (MIND). Contemp. Clin. Trials 75, 19–28 (2018).
Brenner, B. M. & Chertow, G. M. Congenital oligonephropathy and the etiology of adult hypertension and progressive renal injury. Am. J. Kidney Dis. 23, 171–175 (1994).
Crume, T. L. et al. Association of exposure to diabetes in utero with adiposity and fat distribution in a multiethnic population of youth: the Exploring Perinatal Outcomes among Children (EPOCH) study. Diabetologia 54, 87–92 (2011).
Fetita, L. S., Sobngwi, E., Serradas, P., Calvo, F. & Gautier, J. F. Consequences of fetal exposure to maternal diabetes in offspring. J. Clin. Endocrinol. Metab. 91, 3718–3724 (2006).
Dong, M. Z. et al. Diabetic uterine environment leads to disorders in metabolism of offspring. Front. Cell Dev. Biol. 9, 706879 (2021).
Hockett, C. W. et al. Persistent effects of in utero overnutrition on offspring adiposity: the Exploring Perinatal Outcomes among Children (EPOCH) study. Diabetologia 62, 2017–2024 (2019).
Sauder, K. A., Hockett, C. W., Ringham, B. M., Glueck, D. H. & Dabelea, D. Fetal overnutrition and offspring insulin resistance and beta-cell function: the Exploring Perinatal Outcomes among Children (EPOCH) study. Diabet. Med. 34, 1392–1399 (2017).
Crume, T. L. et al. The influence of exposure to maternal diabetes in utero on the rate of decline in beta-cell function among youth with diabetes. J. Pediatr. Endocrinol. Metab. 26, 721–727 (2013).
Wicklow, B. A. et al. Association of gestational diabetes and type 2 diabetes exposure in utero with the development of type 2 diabetes in first nations and non-first nations offspring. JAMA Pediatr. 172, 724–731 (2018).
Agarwal, P. et al. Maternal obesity, diabetes during pregnancy and epigenetic mechanisms that influence the developmental origins of cardiometabolic disease in the offspring. Crit. Rev. Clin. Lab. Sci. 55, 71–101 (2018).
Wicklow, B. A. & Sellers, E. A. Maternal health issues and cardio-metabolic outcomes in the offspring: a focus on Indigenous populations. Best. Pract. Res. Clin. Obstet. Gynaecol. 29, 43–53 (2015).
Dabelea, D., Knowler, W. C. & Pettitt, D. J. Effect of diabetes in pregnancy on offspring: follow-up research in the Pima Indians. J. Matern. Fetal Med. 9, 83–88 (2000).
Freinkel, N. Banting Lecture 1980. Of pregnancy and progeny. Diabetes 29, 1023–1035 (1980).
Damm, P. et al. Gestational diabetes mellitus and long-term consequences for mother and offspring: a view from Denmark. Diabetologia 59, 1396–1399 (2016).
Nelson, R. G., Morgenstern, H. & Bennett, P. H. Intrauterine diabetes exposure and the risk of renal disease in diabetic Pima Indians. Diabetes 47, 1489–1493 (1998).
Cerqueira, D. M. et al. In utero exposure to maternal diabetes impairs nephron progenitor differentiation. Am. J. Physiol. Ren. Physiol. 317, F1318–F1330 (2019).
American Diabetes Association. 13. Children and adolescents: standards of medical care in diabetes-2021. Diabetes Care 44, S180–S199 (2021).
American Diabetes Association. 10. Cardiovascular disease and risk management: standards of medical care in diabetes-2021. Diabetes Care 44, S125–S150 (2021).
Arnett, D. K. et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 140, e596–e646 (2019).
Whelton, S. P., Chin, A., Xin, X. & He, J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann. Intern. Med. 136, 493–503 (2002).
Pierce, G. L., Eskurza, I., Walker, A. E., Fay, T. N. & Seals, D. R. Sex-specific effects of habitual aerobic exercise on brachial artery flow-mediated dilation in middle-aged and older adults. Clin. Sci. 120, 13–23 (2011).
DeSouza, C. A. et al. Regular aerobic exercise prevents and restores age-related declines in endothelium-dependent vasodilation in healthy men. Circulation 102, 1351–1357 (2000).
Look, A. R. G. Effect of a long-term behavioural weight loss intervention on nephropathy in overweight or obese adults with type 2 diabetes: a secondary analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2, 801–809 (2014).
Eskurza, I., Monahan, K. D., Robinson, J. A. & Seals, D. R. Effect of acute and chronic ascorbic acid on flow-mediated dilatation with sedentary and physically active human ageing. J. Physiol. 556, 315–324 (2004).
Martens, C. R., Kirkman, D. L. & Edwards, D. G. The vascular endothelium in chronic kidney disease: a novel target for aerobic exercise. Exerc. sport. Sci. Rev. 44, 12–19 (2016).
Slaght, J. L. et al. Physical activity and cardiometabolic health in adolescents with type 2 diabetes: a cross-sectional study. BMJ Open Diabetes Res. Care 9, e002134 (2021).
Stutts, W. C. Physical activity determinants in adults. Perceived benefits, barriers, and self efficacy. AAOHN J. 50, 499–507 (2002).
El Ansari, W. & Lovell, G. Barriers to exercise in younger and older non-exercising adult women: a cross sectional study in London, United Kingdom. Int. J. Env. Res. Public Health 6, 1443–1455 (2009).
Kelly, S. et al. Barriers and facilitators to the uptake and maintenance of healthy behaviours by people at mid-life: a rapid systematic review. PLoS ONE 11, e0145074 (2016).
Faulkner, M. S. & Michaliszyn, S. F. Exercise adherence in hispanic adolescents with obesity or type 2 diabetes. J. Pediatr. Nurs. 56, 7–12 (2021).
Egan, A. M. et al. Barriers to exercise in obese patients with type 2 diabetes. QJM 106, 635–638 (2013).
Thomas, N., Alder, E. & Leese, G. P. Barriers to physical activity in patients with diabetes. Postgrad. Med. J. 80, 287–291 (2004).
Siddiqi, Z., Tiro, J. A. & Shuval, K. Understanding impediments and enablers to physical activity among African American adults: a systematic review of qualitative studies. Health Educ. Res. 26, 1010–1024 (2011).
Yarwood, J., Carryer, J. & Gagan, M. J. Women maintaining physical activity at midlife: contextual complexities. Nurs. Prax. N. Z. 21, 24–37 (2005).
Babakus, W. S. & Thompson, J. L. Physical activity among South Asian women: a systematic, mixed-methods review. Int. J. Behav. Nutr. Phys. Act. 9, 150 (2012).
Jaser, S. S., Holl, M. G., Jefferson, V. & Grey, M. Correlates of depressive symptoms in urban youth at risk for type 2 diabetes mellitus. J. Sch. Health 79, 286–292 (2009).
Roshanravan, B., Gamboa, J. & Wilund, K. Exercise and CKD: skeletal muscle dysfunction and practical application of exercise to prevent and treat physical impairments in CKD. Am. J. Kidney Dis. 69, 837–852 (2017).
McGavock, J., Dart, A. & Wicklow, B. Lifestyle therapy for the treatment of youth with type 2 diabetes. Curr. Diab Rep. 15, 568 (2015).
Zeitler, P. et al. ISPAD clinical practice consensus guidelines 2018: type 2 diabetes mellitus in youth. Pediatr. Diabetes 19, 28–46 (2018).
Madiraju, A. K. et al. Metformin suppresses gluconeogenesis by inhibiting mitochondrial glycerophosphate dehydrogenase. Nature 510, 542–546 (2014).
Kelsey, M. M. et al. Presentation and effectiveness of early treatment of type 2 diabetes in youth: lessons from the TODAY study. Pediatr. Diabetes 17, 212–221 (2016).
RISE Consortium. Impact of insulin and metformin versus metformin alone on beta-cell function in youth with impaired glucose tolerance or recently diagnosed type 2 diabetes. Diabetes Care 41, 1717–1725 (2018).
Tamborlane, W. V. et al. Liraglutide in children and adolescents with type 2 diabetes. N. Engl. J. Med. 381, 637–646 (2019).
Arslanian, S. A. et al. Once-weekly dulaglutide for the treatment of youths with type 2 diabetes. N. Engl. J. Med. 387, 433–443 (2022).
Tamborlane, W. V. et al. Once-weekly exenatide in youth with type 2 diabetes. Diabetes Care 45, 1833–1840 (2022).
Nauck, M. A., Quast, D. R., Wefers, J. & Meier, J. J. GLP-1 receptor agonists in the treatment of type 2 diabetes - state-of-the-art. Mol. Metab. 46, 101102 (2021).
Lebovitz, H. E. Thiazolidinediones: the forgotten diabetes medications. Curr. Diab. Rep. 19, 151 (2019).
DeFronzo, R. A., Eldor, R. & Abdul-Ghani, M. Pathophysiologic approach to therapy in patients with newly diagnosed type 2 diabetes. Diabetes Care 36, S127–S138 (2013).
Singh, S., Loke, Y. K. & Furberg, C. D. Thiazolidinediones and heart failure: a teleo-analysis. Diabetes Care 30, 2148–2153 (2007).
Gottschalk, M., Danne, T., Vlajnic, A. & Cara, J. F. Glimepiride versus metformin as monotherapy in pediatric patients with type 2 diabetes: a randomized, single-blind comparative study. Diabetes Care 30, 790–794 (2007).
Tamborlane, W. V. et al. Efficacy and safety of dapagliflozin in children and young adults with type 2 diabetes: a prospective, multicentre, randomised, parallel group, phase 3 study. Lancet Diabetes Endocrinol. 10, 341–350 (2022).
Bjornstad, P. et al. Acute effect of empagliflozin on fractional excretion of sodium and eGFR in youth with type 2 diabetes. Diabetes Care 41, e129–e130 (2018).
Schauer, P. R. et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N. Engl. J. Med. 366, 1567–1576 (2012).
Sjostrom, L. Review of the key results from the Swedish Obese Subjects (SOS) trial-a prospective controlled intervention study of bariatric surgery. J. Intern. Med. 273, 219–234 (2013).
Sjostrom, L. et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA 311, 2297–2304 (2014).
Schauer, P. R. et al. Bariatric surgery versus intensive medical therapy for diabetes–5-year outcomes. N. Engl. J. Med. 376, 641–651 (2017).
Schauer, P. R. et al. Bariatric surgery versus intensive medical therapy for diabetes–3–year outcomes. N. Engl. J. Med. 370, 2002–2013 (2014).
Inge, T. H. et al. Weight loss and health status 3 years after bariatric surgery in adolescents. N. Engl. J. Med. 374, 113–123 (2016).
Inge, T. H. et al. Comparison of surgical and medical therapy for type 2 diabetes in severely obese adolescents. JAMA Pediatr. 172, 452–460 (2018).
Ryder, J. R. et al. Effect of surgical versus medical therapy on estimated cardiovascular event risk among adolescents with type 2 diabetes and severe obesity. Surg. Obes. Relat. Dis. 17, 23–33 (2021).
Bjornstad, P. et al. Effect of surgical versus medical therapy on diabetic kidney disease over 5 years in severely obese adolescents with type 2 diabetes. Diabetes Care 43, 187–195 (2020).
Shah, A. S. et al. Study protocol: a prospective controlled clinical trial to assess surgical or medical treatment for paediatric type 2 diabetes (ST(2)OMP). BMJ Open. 11, e047766 (2021).
Shah, A. S. et al. Metabolic outcomes of surgery in youth with type 2 diabetes. Semin. Pediatr. Surg. 29, 150893 (2020).
Dabelea, D. et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 311, 1778–1786 (2014). Among teenagers and young adults who were diagnosed with diabetes during childhood or adolescence, the prevalence of complications and comorbidities was higher in those with T2DM than those with T1DM.
WHO. Obesity, https://www.who.int/health-topics/obesity (2022).
Tönnies, T. et al. 156-OR: Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2060. Diabetes 70 (Suppl. 1), Abstr. 156-OR (2021).
TODAY Study Group. Rapid rise in hypertension and nephropathy in youth with type 2 diabetes: the TODAY clinical trial. Diabetes Care 36, 1735–1741 (2013).
RISE Consortium. Lack of durable improvements in beta-cell function following withdrawal of pharmacological interventions in adults with impaired glucose tolerance or recently diagnosed type 2 diabetes. Diabetes Care 42, 1742–1751 (2019).
Bhatt, D. L. et al. Sotagliflozin in patients with diabetes and chronic kidney disease. N. Engl. J. Med. 384, 129–139 (2020).
Perkovic, V. et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N. Engl. J. Med. 380, 2295–2306 (2019).
Mann, J. F. E. et al. Liraglutide and renal outcomes in type 2 diabetes. N. Engl. J. Med. 377, 839–848 (2017).
Wanner, C. et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N. Engl. J. Med. 375, 323–334 (2016).
Acknowledgements
The authors’ work was supported in part by the Intramural Research Program of the NIDDK. P.B. receives salary and research support from NIDDK (R01 DK129211, R01 DK132399, R21 DK129720, K23 DK116720, UC DK114886 and P30 DK116073), NHLBI (R01 HL165433), JDRF (3-SRA-2022-1097-M-B, 3-SRA-2022-1243-M-B, 2-SRA-2019-845-S-B), Boettcher Foundation, AHA (20IPA35260142), Center for Women’s Health Research at University of Colorado, the Department of Paediatrics, Section of Endocrinology and Barbara Davis Center for Diabetes at University of Colorado School of Medicine. D.H.v.R. is supported by a senior fellowship of the Dutch Diabetes Foundation. K.J.N. receives salary and research support from NIDDK (R01 DK119450) and NHLBI (K24 HL145076, R01 HL165433). A.S.S. receives salary and research support from NIDDK (R01 DK119450), NHLBI (R01 HL157260) and NINDS (R01 NS125316). The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, made substantial contributions to discussions of the content, wrote, reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
P.B. has acted as a consultant for AstraZeneca, Bayer, Bristol-Myers Squibb, Boehringer Ingelheim, Eli Lilly, LG Chem, Sanofi, Novo Nordisk, Horizon Pharma, XORTX. P.B. serves on the advisory boards of AstraZeneca, Bayer, Boehringer Ingelheim, Novo Nordisk and XORTX. D.H.v.R. has acted as a consultant and received honoraria from AstraZeneca, Boehringer Ingelheim, Eli Lilly, Merck and Sanofi, and received research operating funding from AstraZeneca, Boehringer Ingelheim–Eli Lilly Diabetes Alliance and Merck. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Nephrology thanks Amy Mottl, Angela Titmuss and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
DiCAYA: https://www.dicaya.org
Glossary
- Standardized mortality ratio
-
The ratio of the number of deaths observed in a population over a given period to the number that would be expected over the same period in the general population.
Rights and permissions
About this article
Cite this article
Bjornstad, P., Chao, L.C., Cree-Green, M. et al. Youth-onset type 2 diabetes mellitus: an urgent challenge. Nat Rev Nephrol 19, 168–184 (2023). https://doi.org/10.1038/s41581-022-00645-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-022-00645-1
This article is cited by
-
Sirtuins in kidney diseases: potential mechanism and therapeutic targets
Cell Communication and Signaling (2024)
-
Non-invasive diagnostic potential of salivary miR-25-3p for periodontal disease and osteoporosis among a cohort of elderly patients with type 2 diabetes mellitus
BMC Oral Health (2023)
-
Zunahme der Typ-2-Diabetes-Inzidenz unter Jugendlichen
Info Diabetologie (2023)