Abstract
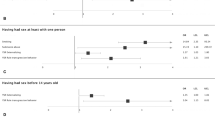
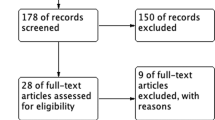
Transgender people and their next-of-kin may request information on sexual orientation and preferred partners during hormonal affirming process. Although previous research on sexual orientation in transgender people is extensive, this literature may already be outdated and/or the methodology of studies assessing sexual orientation may fall short. This prospective cohort study was part of the European Network for the Investigation of Gender Incongruence (ENIGI). Gender role and preferred partner in sexual fantasies, sexual orientation and gender of current sexual partner were assessed at baseline (initiation of HT) and every follow-up visit. Data from 469 transgender women (TW) and 433 transgender men (TM) were analyzed cross-sectionally and prospectively. At baseline, more than half reported having no partner (35% of TW, 47% of TM). After 12 months, more than half reported having a partner (59% of TW, 56% of TM), with no changes between one and three years of HT. The majority of TM preferred a female partner, TW preferred male and female partners. The sexual identity of their partner matched their sexual orientation in >80%. Sexual orientation did not change over time. We did not observe associations with serum levels of sex steroids or gender-affirming surgery (chest or genital surgery). Sexual orientation did not change during hormonal transition and was not associated with sex steroids or surgery. Also, preferences matched the partner’s sexual identity. We do not assume that changing serum levels of sex steroids is directly associated with changes in partner choice. The number of people with a current partner increased, possibly due to the indirect effects of gender-affirming care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Auer MK, Fuss J, Höhne N, Stalla GK, Sievers C. Transgender transitioning and change of self-reported sexual orientation. PLoS ONE. 2014;9:e110016.
Weyers S, Elaut E, De Sutter P, Gerris J, T’Sjoen G, Heylens G, et al. Long-term assessment of the physical, mental, and sexual health among transsexual women. J Sex Med. 2009;6:752–60.
Meier SC, Pardo ST, Labuski C, Babcock J. Measures of clinical health among female-to-male transgender persons as a function of sexual orientation. Arch Sex Behav. 2013;42:463–74.
Katz-Wise SL, Reisner SL, Hughto JW, Keo-Meier CL. Differences in sexual orientation diversity and sexual fluidity in attractions among gender minority adults in Massachusetts. J Sex Res. 2016;53:74–84.
Bockting W, Benner A, Coleman E. Gay and bisexual identity development among female-to-male transsexuals in North America: emergence of a transgender sexuality. Arch Sex Behav. 2009;38:688–701.
Lawrence AA. Sexuality before and after male-to-female sex reassignment surgery. Arch Sex Behav. 2005;34:147–66.
Gaither TW, Awad MA, Osterberg EC, Romero A, Bowers ML, Breyer BN. Impact of sexual orientation identity on medical morbidities in male-to-female transgender patients. LGBT Health. 2017;4:11–6.
Papadopulos NA, Lellé JD, Zavlin D, Herschbach P, Henrich G, Kovacs L, et al. Psychological pathologies and sexual orientation in transgender women undergoing gender confirming treatment. Ann Plast Surg. 2020;84:312–6.
De Vries ALC, Steensma TD, Doreleijers TAH, Cohen-Kettenis PT. Puberty suppression in adolescents with gender identity disorder: a prospective follow-up study. J Sex Med. 2011;8:2276–83.
Lawrence AA. Sexual orientation versus age of onset as bases for typologies (subtypes) for gender identity disorder in adolescents and adults. Arch Sex Behav. 2010;39:514–45.
Rachlin K. Factors which influence individual’s decisions when considering female-to-male genital reconstructive surgery. Int J Transgender Health. 1999;3:18–20.
Chivers ML, Bailey JM. Sexual orientation of female-to-male transsexuals: a comparison of homosexual and nonhomosexual types. Arch Sex Behav. 2000;29:259–78.
Reisner SL, White JM, Mayer KH, Mimiaga MJ. Sexual risk behaviors and psychosocial health concerns of female-to-male transgender men screening for STDs at an urban community health center. AIDS Care. 2014;26:857–64.
Kenagy GP, Hsieh CM, Kennedy G. The risk less known: female-to-male transgender persons’ vulnerability to HIV infection. AIDS Care - Psychol Socio-Med Asp AIDS/HIV. 2005;17:195–207.
Nieder TO, Herff M, Cerwenka S, Preuss WF, Cohen-Kettenis PT, De Cuypere G, et al. Age of onset and sexual orientation in transsexual males and females. J Sex Med. 2011;8:783–91.
Cerwenka S, Nieder TO, Cohen-Kettenis P, De Cuypere G, Haraldsen IRH, Kreukels BPC, et al. Sexual behavior of gender-dysphoric individuals before gender-confirming interventions: a European multicenter study. J Sex Marital Ther. 2014;40:457–71.
Cerwenka S, Nieder TO, Briken P, Cohen-Kettenis PT, De Cuypere G, Haraldsen IRH, et al. Intimate partnerships and sexual health in gender-dysphoric individuals before the start of medical treatment. Int J Sex Health. 2014;26:52–65.
Nieder TO, Elaut E, Richards C, Dekker A. Sexual orientation of trans adults is not linked to outcome of transition-related health care, but worth asking. Int Rev Psychiatry. 2016;28:103–11.
De Roo C, Tilleman K, T’Sjoen G, De Sutter P. Fertility options in transgender people. Int Rev Psychiatry. 2016;28:112–9.
Kreukels BPC, Haraldsen IR, De Cuypere G, Richter-Appelt H, Gijs L, Cohen-Kettenis PT. A European network for the investigation of gender incongruence: the ENIGI initiative. Eur Psychiatry. 2012;27:445–50.
Dekker MJHJ, Wierckx K, Van Caenegem E, Klaver M, Kreukels BP, Elaut E, et al. A European network for the investigation of gender incongruence: endocrine part. J Sex Med. 2016;13:994–9.
Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, De Cuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people. Int J Transgender Health. 2012;13:165–232.
Kinsey AC, Martin CE, Pomeroy WB. Kinsey Scale. WB Saunders; Philadelphia PA, USA; 1948.
Wiepjes CM, Vlot MC, Klaver M, Nota NM, de Blok CJM, de Jongh RT, et al. Bone mineral density increases in trans persons after 1 year of hormonal treatment: a multicenter prospective observational study. J Bone Miner Res. 2017;32:1252–60.
Defreyne J, Kreukels B, T’Sjoen G, Staphorsius A, Den Heijer M, Heylens G, et al. No correlation between serum testosterone levels and state-level anger intensity in transgender people: results from the European Network for the Investigation of Gender Incongruence. Hormones Behav. 2019;110:29–39.
Defreyne J, Elaut E, Kreukels B, Fisher AD, Castellini G, Staphorsius A, et al. Sexual desire changes in transgender individuals upon initiation of hormone treatment: results from the longitudinal European network for the investigation of gender incongruence. J Sex Med. 2020;17:812–25.
Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65–70.
Fein LA, Salgado CJ, Sputova K, Estes CM, Medina CA. Sexual preferences and partnerships of transgender persons mid- or post-transition. J Homosex. 2018;65:659–71.
Rowniak S, Chesla C. Coming out for a third time: transmen, sexual orientation, and identity. Arch Sex Behav. 2013;42:449–61.
Katz-Wise SL, Hyde JS. Sexual fluidity and related attitudes and beliefs among young adults with a same-gender orientation. Arch Sex Behav. 2015;44:1459–70.
Fundamental Rights Agency. Being trans in the EU—comparative analysis of the EU LGBT survey data. Luxembourg: Fundamental Rights Agency; 2014.
Statbel. Population by place of residence, nationality (Belgian/non-Belgian), marital status, age and gender. Statbel (Directorate-general Statistics - Statistics Belgium); Brussels, Belgium; 2020.
Fisher AD, Castellini G, Ristori J, Casale H, Cassioli E, Sensi C, et al. Cross-sex hormone treatment and psychobiological changes in transsexual persons: two-year follow-up data. J Clin Endocrinol Metab. 2016;101:4260–9.
Fisher AD, Castellini G, Bandini E, Casale H, Fanni E, Benni L, et al. Cross‐sex hormonal treatment and body uneasiness in individuals with gender dysphoria. J Sex Med. 2014;11:709–19.
van de Grift TC, Elaut E, Cerwenka SC, Cohen-Kettenis PT, De Cuypere G, Richter-Appelt H, et al. Effects of medical interventions on gender dysphoria and body image: a follow-up study. Psychosom Med. 2017;79:815.
Heylens G, Verroken C, De Cock S, T’Sjoen G, De Cuypere G. Effects of different steps in gender reassignment therapy on psychopathology: a prospective study of persons with a gender identity disorder. J Sex Med. 2014;11:119–26.
Fisher AD, Bandini E, Casale H, Ferruccio N, Meriggiola MC, Gualerzi A, et al. Sociodemographic and clinical features of gender identity disorder: an Italian multicentric evaluation. J Sex Med. 2013;10:408–19.
Kuper LE, Nussbaum R, Mustanski B. Exploring the diversity of gender and sexual orientation identities in an online sample of transgender individuals. J Sex Res. 2012;56:249–63.
Baker WB. The meaning of sexual and gender identities in transgender men. Montclair State University; 2017.
Wierckx K, Elaut E, Van Hoorde B, Heylens G, De Cuypere G, Monstrey S, et al. Sexual desire in trans persons: associations with sex reassignment treatment. J Sex Med. 2014;11:107–18.
Nuttbrock L, Hwahng S, Bockting W, Rosenblum A, Mason M, Macri M, et al. Lifetime risk factors for HIV/sexually transmitted infections among male-to-female transgender persons. J Acquired Immune Defic Syndr. 2009;52:417–21.
Acknowledgements
We would like to thank the people who contributed to the ENIGI study: Sarah Collet, Meltem Kiyar, Thomas Schreiner, Timo Nieder, Inga Becker, Yona Greenman, Chantal Wiepjes, Maartje Klaver, Christel De Blok, Nienke Nota, Carlotta Cocchetti, Koen Dreijerink, Daan Van Velzen, Dennis Van Dijk, Margot Morssinkhof, Elfi Conemans, Brand Coumou, and Iris de Nie. We also thank all endocrinology residents who made a valuable contribution to the ENIGI study: Greet Roef, Mirra Boer, Marijn Carpentier, Liesbeth Van Huffel, Sara Vandewalle, Loes Moernaut, Sabine Vermeersch, Gertjan Vereecke, Xavier-Philippe Aers, Charlotte Verroken, Emmanuelle Versele, Eva Van Caenegem, Katrien Wierckx, and Bram Vantomme for their outpatient care; Charlotte Bultynck, Charlotte Pas, Anne-Sophie De Maertelaere, and Kessewa Abosi-Appeadu for their help with the dataset; our study nurse Kaatje Toye for handling the extensive administration to the study, and all participants in the ENIGI study protocol.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Defreyne, J., Elaut, E., Den Heijer, M. et al. Sexual orientation in transgender individuals: results from the longitudinal ENIGI study. Int J Impot Res 33, 694–702 (2021). https://doi.org/10.1038/s41443-020-00402-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-020-00402-7
This article is cited by
-
The interrelations between resilience, distress, and transphobia among transgender individuals in Israel
Current Psychology (2024)