Abstract
Background/Objectives
While dyslipidaemia has been suggested as a potential risk factor for diabetic retinopathy (DR), previous studies have reported conflicting findings. This study aimed to better characterize the relationship between abnormal serum levels of various lipid markers and the risk of the development and progression of DR.
Subjects/Methods
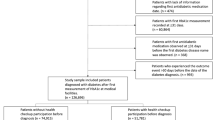
This retrospective cohort study utilized a United States national database of electronic medical records. Adults with a history of type 2 diabetes mellitus without type 1 diabetes mellitus were divided into cohorts based on the presence of abnormal serum levels of various lipid markers. Propensity score matching was performed to match cohorts with abnormal lipid levels to those with normal lipid levels on covariates. The cohorts were then compared to evaluate the hazard ratios (HR) of receiving a new DR diagnosis, pars plana vitrectomy, panretinal photocoagulation, vitreous haemorrhage, proliferative diabetic retinopathy, diabetic macular oedema (DMO), and traction retinal detachment.
Results
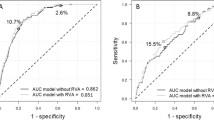
The database contained 1,126,231 eligible patients (mean age: 60.8 [14.2] years; 46.0% female). Among patients without prior DR, low HDL (HR = 0.94, CI = 0.90–0.98), total cholesterol (HR = 0.88, CI = 0.85–0.91), and high triglyceride (HR = 0.91, CI = 0.86–0.97) levels were associated with a decreased risk of receiving a DR diagnosis. Among patients with preexisting DR, high LDL levels was associated with an increased risk of DMO (HR = 1.42, CI = 1.15–1.75), whereas low HDL levels was associated with a marginally decreased risk (HR = 0.92, CI = 0.85–0.99).
Conclusions
Elevated levels of markers of dyslipidaemia are inversely associated with the risk of receiving a DR diagnosis, but this relationship is blunted after the onset of DR.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The de-identified data used in this research is available in the TriNetX research platform at https://live.trinetx.com, but a request may be necessary and costs may be incurred.
References
Kollias AN, Ulbig MW. Diabetic Retinopathy. Dtsch Arztebl Int. 2010;107:75–84.
Teo ZL, Tham YC, Yu M, Chee ML, Rim TH, Cheung N, et al. Global Prevalence of Diabetic Retinopathy and Projection of Burden through 2045: Systematic Review and Meta-analysis. Ophthalmology 2021;128:1580–91.
Lee R, Wong TY, Sabanayagam C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis (Lond). 2015;2:17.
Wong TY, Cheung CMG, Larsen M, Sharma S, Simó R. Diabetic retinopathy. Nat Rev Dis Prim. 2016;2:1–17.
Ulbig MRW, Hamilton AMP. Factors influencing the natural history of diabetic retinopathy. Eye. 1993;7:242–9.
Porta M, Sjoelie AK, Chaturvedi N, Stevens L, Rottiers R, Veglio M, et al. Risk factors for progression to proliferative diabetic retinopathy in the EURODIAB Prospective Complications Study. Diabetologia. 2001;44:2203–9.
Matthews DR, Stratton IM, Aldington SJ, Holman RR, Kohner EM, UK Prospective Diabetes Study Group. Risks of progression of retinopathy and vision loss related to tight blood pressure control in type 2 diabetes mellitus: UKPDS 69. Arch Ophthalmol. 2004;122:1631–40.
Chang YC, Wu WC. Dyslipidemia and Diabetic Retinopathy. Rev Diabet Stud. 2013;10:121–32.
Zhou Y, Wang C, Shi K, Yin X. Relationship between dyslipidemia and diabetic retinopathy: A systematic review and meta-analysis. Medicine. 2018;97:e12283.
Modjtahedi BS, Bose N, Papakostas TD, Morse L, Vavvas DG, Kishan AU. Lipids and Diabetic Retinopathy. Semin Ophthalmol. 2016;31:10–8.
Chou Y, Ma J, Su X, Zhong Y. Emerging insights into the relationship between hyperlipidemia and the risk of diabetic retinopathy. Lipids Health Dis. 2020;19:241.
van Leiden HA, Dekker JM, Moll AC, Nijpels G, Heine RJ, Bouter LM, et al. Risk Factors for Incident Retinopathy in a Diabetic and Nondiabetic Population: The Hoorn Study. Arch Ophthalmol. 2003;121:245–51.
Wang NK, Lai CC, Wang JP, Wu WC, Liu L, Yeh LK, et al. Risk factors associated with the development of retinopathy 10 yr after the diagnosis of juvenile-onset type 1 diabetes in Taiwan: a cohort study from the CGJDES. Pediatr Diabetes. 2016;17:407–16.
Davis MD, Fisher MR, Gangnon RE, Barton F, Aiello LM, Chew EY, et al. Risk factors for high-risk proliferative diabetic retinopathy and severe visual loss: Early Treatment Diabetic Retinopathy Study Report #18. Invest Ophthalmol Vis Sci. 1998;39:233–52.
Klein R, Marino EK, Kuller LH, Polak JF, Tracy RP, Gottdiener JS, et al. The relation of atherosclerotic cardiovascular disease to retinopathy in people with diabetes in the Cardiovascular Health Study. Br J Ophthalmol. 2002;86:84–90.
Chung YR, Park SW, Choi SY, Kim SW, Moon KY, Kim JH, et al. Association of statin use and hypertriglyceridemia with diabetic macular edema in patients with type 2 diabetes and diabetic retinopathy. Cardiovasc Diabetol. 2017;16:4.
Wong TY, Cheung N, Tay WT, Wang JJ, Aung T, Saw SM, et al. Prevalence and risk factors for diabetic retinopathy: the Singapore Malay Eye Study. Ophthalmology 2008;115:1869–75.
Miljanovic B, Glynn RJ, Nathan DM, Manson JE, Schaumberg DA. A Prospective Study of Serum Lipids and Risk of Diabetic Macular Edema in Type 1 Diabetes. Diabetes 2004;53:2883–92.
Tan GS, Gan A, Sabanayagam C, Tham YC, Neelam K, Mitchell P, et al. Ethnic Differences in the Prevalence and Risk Factors of Diabetic Retinopathy: The Singapore Epidemiology of Eye Diseases Study. Ophthalmology 2018;125:529–36.
Keech AC, Mitchell P, Summanen PA, O’Day J, Davis TME, Moffitt MS, et al. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): a randomised controlled trial. Lancet. 2007;370:1687–97.
Klein BE, Moss SE, Klein R, Surawicz TS. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. XIII. Relationship of serum cholesterol to retinopathy and hard exudate. Ophthalmology. 1991;98:1261–5.
Ioannidou E, Tseriotis VS, Tziomalos K. Role of lipid-lowering agents in the management of diabetic retinopathy. World J Diabetes. 2017;8:1–6.
Kronenberg F. Lipoprotein(a). Handb Exp Pharm. 2022;270:201–32.
Kang EYC, Chen TH, Garg SJ, Sun CC, Kang JH, Wu WC, et al. Association of Statin Therapy With Prevention of Vision-Threatening Diabetic Retinopathy. JAMA Ophthalmol. 2019;137:363–71.
Vail D, Callaway NF, Ludwig CA, Saroj N, Moshfeghi DM. Lipid-Lowering Medications Are Associated with Lower Risk of Retinopathy and Ophthalmic Interventions among United States Patients with Diabetes. Am J Ophthalmol. 2019;207:378–84.
Kawasaki R, Konta T, Nishida K. Lipid-lowering medication is associated with decreased risk of diabetic retinopathy and the need for treatment in patients with type 2 diabetes: A real-world observational analysis of a health claims database. Diabetes, Obes Metab. 2018;20:2351–60.
Pranata R, Vania R, Victor AA. Statin reduces the incidence of diabetic retinopathy and its need for intervention: A systematic review and meta-analysis. Eur J Ophthalmol. 2021;31:1216–24.
Keech A, Simes RJ, Barter P, Best J, Scott R, Taskinen MR, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet 2005;366:1849–61.
ACCORD Study Group, ACCORD Eye Study Group, Chew EY, Ambrosius WT, Davis MD, Danis RP, et al. Effects of medical therapies on retinopathy progression in type 2 diabetes. N Engl J Med. 2010;363:233–44.
Schoenfeld D. Partial residuals for the proportional hazards regression model. Biometrika. 1982;69:239–41.
In J, Lee DK. Survival analysis: part II – applied clinical data analysis. Korean J Anesthesiol. 2019;72:441–57.
Kuitunen I, Ponkilainen VT, Uimonen MM, Eskelinen A, Reito A. Testing the proportional hazards assumption in cox regression and dealing with possible non-proportionality in total joint arthroplasty research: methodological perspectives and review. BMC Musculoskelet Disord. 2021;22:489.
Hancock MJ, Maher CG, Costa LdaCM, Williams CM. A guide to survival analysis for manual therapy clinicians and researchers. Man Ther. 2014;19:511–6.
Scott IU, Campochiaro PA, Newman NJ, Biousse V. Retinal Vascular Occlusions. Lancet. 2020;396:1927–40.
Stroke - Causes and Risk Factors | NHLBI, NIH [Internet]. [cited 2023 Jun 19]. Available from: https://www.nhlbi.nih.gov/health/stroke/causes (2022).
Wilson PW. Established risk factors and coronary artery disease: the Framingham Study. Am J Hypertens. 1994;7:7S–12S.
Cheung N, Wang JJ, Klein R, Couper DJ, Sharrett AR, Wong TY. Diabetic Retinopathy and the Risk of Coronary Heart Disease: The Atherosclerosis Risk in Communities Study. Diabetes Care. 2007;30:1742–6.
Miksenas H, Januzzi JL Jr, Natarajan P. Lipoprotein(a) and Cardiovascular Diseases. JAMA 2021;326:352–3.
Reyes-Soffer G, Ginsberg HN, Berglund L, Duell PB, Heffron SP, Kamstrup PR, et al. Lipoprotein(a): A Genetically Determined, Causal, and Prevalent Risk Factor for Atherosclerotic Cardiovascular Disease: A Scientific Statement From the American Heart Association. Arteriosclerosis, Thrombosis, Vasc Biol. 2022;42:e48–60.
Lu M, Lu Q, Zhang Y, Tian G. ApoB/apoA1 is an effective predictor of coronary heart disease risk in overweight and obesity. J Biomed Res. 2011;25:266–73.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082–143.
Davidson MH, Ballantyne CM, Jacobson TA, Bittner VA, Braun LT, Brown AS, et al. Clinical utility of inflammatory markers and advanced lipoprotein testing: Advice from an expert panel of lipid specialists. J Clin Lipidol. 2011;5:338–67.
Mozetic V, Pacheco RL, Latorraca C, de Oliveira Cruz Latorraca C, Riera R. Statins and/or fibrates for diabetic retinopathy: a systematic review and meta-analysis. Diabetol Metab Syndr. 2019;11:92.
Narang S, Sood S, Kaur B, Singh R, Mallik A, Kaur J. Atorvastatin in clinically-significant macular edema in diabetics with a normal lipid profile. Nepal J Ophthalmol. 2012;4:23–8.
Zhang J, McGwin G. Association of statin use with the risk of developing diabetic retinopathy. Arch Ophthalmol. 2007;125:1096–9.
Dodson PM. Management of diabetic retinopathy: could lipid-lowering be a worthwhile treatment modality? Eye. 2009;23:997–1003.
Staels B, Dallongeville J, Auwerx J, Schoonjans K, Leitersdorf E, Fruchart JC. Mechanism of Action of Fibrates on Lipid and Lipoprotein Metabolism. Circulation. 1998;98:2088–93.
Bradford RH, Goldberg AC, Schonfeld G, Knopp RH. Double-blind comparison of bezafibrate versus placebo in male volunteers with hyperlipoproteinemia. Atherosclerosis 1992;92:31–40.
Trudeau K, Roy S, Guo W, Hernández C, Villarroel M, Simó R, et al. Fenofibric Acid Reduces Fibronectin and Collagen Type IV Overexpression in Human Retinal Pigment Epithelial Cells Grown in Conditions Mimicking the Diabetic Milieu: Functional Implications in Retinal Permeability. Invest Ophthalmol Vis Sci. 2011;52:6348–54.
Hsu YJ, Lin CW, Cho SL, Yang WS, Yang CM, Yang CH. Protective Effect of Fenofibrate on Oxidative Stress-Induced Apoptosis in Retinal–Choroidal Vascular Endothelial Cells: Implication for Diabetic Retinopathy Treatment. Antioxid (Basel). 2020;9:712.
Ding L, Cheng R, Hu Y, Takahashi Y, Jenkins AJ, Keech AC, et al. Peroxisome Proliferator–Activated Receptor α Protects Capillary Pericytes in the Retina. Am J Pathol. 2014;184:2709–20.
Huang L, Liang W, Zhou K, Wassel RA, Ridge ZD, Ma JX, et al. Therapeutic Effects of Fenofibrate Nano-Emulsion Eye Drops on Retinal Vascular Leakage and Neovascularization. Biol (Basel). 2021;10:1328.
Noonan JE, Jenkins AJ, Ma JX, Keech AC, Wang JJ, Lamoureux EL. An Update on the Molecular Actions of Fenofibrate and Its Clinical Effects on Diabetic Retinopathy and Other Microvascular End Points in Patients With Diabetes. Diabetes. 2013;62:3968–75.
Wang F, Wang X, Ye P, Cao R, Zhang Y, Qi Y, et al. High-density lipoprotein 3 cholesterol is a predictive factor for arterial stiffness: a community-based 4.8-year prospective study. Lipids Health Dis. 2018;17:5.
Salonen JT, Salonen R, Seppänen K, Rauramaa R, Tuomilehto J. HDL, HDL2, and HDL3 subfractions, and the risk of acute myocardial infarction. A prospective population study in eastern Finnish men. Circulation. 1991;84:129–39.
Williams PT, Feldman DE. Prospective study of coronary heart disease vs HDL2, HDL3, and other lipoproteins in Gofman’s Livermore Cohort. Atherosclerosis 2011;214:196–202.
Hoogeveen RC, Gaubatz JW, Sun W, Dodge RC, Crosby JR, Jiang J, et al. Small Dense LDL Cholesterol Concentrations Predict Risk for Coronary Heart Disease: the Atherosclerosis Risk in Communities (ARIC) Study. Arterioscler Thromb Vasc Biol. 2014;34:1069–77.
Johansson J, Carlson LA, Landou C, Hamsten A. High density lipoproteins and coronary atherosclerosis. A strong inverse relation with the largest particles is confined to normotriglyceridemic patients. Arterioscler Thromb. 1991;11:174–82.
Pirillo A, Norata GD, Catapano AL. High-Density Lipoprotein Subfractions - What the Clinicians Need to Know. Cardiology. 2013;124:116–25.
Fu D, Yu JY, Wu M, Du M, Chen Y, Abdelsamie SA, et al. Immune complex formation in human diabetic retina enhances toxicity of oxidized LDL towards retinal capillary pericytes1. J Lipid Res. 2014;55:860–9.
Lyons TJ, Jenkins AJ. Glycation, oxidation, and lipoxidation in the development of the complications of diabetes: a carbonyl stress hypothesis. Diabetes Rev (Alex). 1997;5:365–91.
Du M, Wu M, Fu D, Yang S, Chen J, Wilson K, et al. Effects of modified LDL and HDL on retinal pigment epithelial cells: a role in diabetic retinopathy? Diabetologia 2013;56:2318–28.
Yu JY, Du M, Elliott MH, Wu M, Fu D, Yang S, et al. Extravascular modified lipoproteins: a role in the propagation of diabetic retinopathy in a mouse model of type 1 diabetes. Diabetologia. 2016;59:2026–35.
Norata GD, Pirillo A, Catapano AL. Modified HDL: Biological and physiopathological consequences. Nutr, Metab Cardiovasc Dis. 2006;16:371–86.
Bonizzi A, Piuri G, Corsi F, Cazzola R, Mazzucchelli S. HDL Dysfunctionality: Clinical Relevance of Quality Rather Than Quantity. Biomedicines. 2021;9:729.
Madsen CM, Varbo A, Nordestgaard BG. Extreme high high-density lipoprotein cholesterol is paradoxically associated with high mortality in men and women: two prospective cohort studies. Eur Heart J. 2017;38:2478–86.
Márquez AB, Nazir S, van der Vorst EPC. High-Density Lipoprotein Modifications: A Pathological Consequence or Cause of Disease Progression? Biomedicines 2020;8:549.
Farbstein D, Levy AP. HDL dysfunction in diabetes: causes and possible treatments. Expert Rev Cardiovasc Ther. 2012;10:353–61.
Kohner EM. The evolution and natural history of diabetic retinopathy. Int Ophthalmol Clin. 1978;18:1–16.
Acknowledgements
We would like to thank Dr. David Kaelber and the MetroHealth Medical Center in Cleveland for providing access to the TriNetX database.
Funding
This study was supported by the Clinical and Translational Science Collaborative (CTSC) of Cleveland which is funded by the National Institutes of Health (NIH), National Center for Advancing Translational Science (NCATS), Clinical and Translational Science Award (CTSA) grant, UL1TR002548. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Additional support was provided by P30EY025585(BA-A), the Research to Prevent Blindness (RPB) Challenge Grant, Cleveland Eye Bank Foundation Grant.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study, revised the manuscript, and reviewed the final manuscript. Data collection and statistical analysis were performed by HJ and CMM. Interpretation of the data, writing of the manuscript, and revision of the study design were performed by HJ.
Corresponding author
Ethics declarations
Competing interests
RPS reports personal fees from Genentech/Roche, personal fees from Alcon/Novartis, grants from Apellis and Graybug, personal fees from Zeiss, personal fees from Bausch + Lomb, personal fees from Regeneron Pharmaceuticals, Inc. Inc. All other authors report no disclosures.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jeong, H., Maatouk, C.M., Russell, M.W. et al. Associations between lipid abnormalities and diabetic retinopathy across a large United States national database. Eye (2024). https://doi.org/10.1038/s41433-024-03022-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41433-024-03022-3