Abstract
Objectives
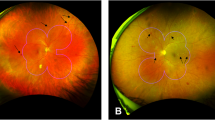
To investigate the association between peripheral non-perfusion index (NPI) on ultrawide-field fluorescein angiography (UWF-FA) and quantitative OCT-Angiography (OCT-A) metrics in the macula.
Methods
In total, 48 eyes with UWF-colour fundus photos (CFP), UWF-FA (California, Optos) and OCT-A (Spectralis, Heidelberg) were included. OCT-A (3 × 3 mm) was used to determine foveal avascular zone (FAZ) parameters and vessel density (VD), perfusion density (PD), fractal dimension (FD) on superficial capillary plexus (SCP). NPI’s extent and distribution was determined on UWF-FA within fovea centred concentric rings corresponding to posterior pole (<10 mm), mid-periphery (10–15 mm), and far-periphery (>15 mm) and within the total retinal area, the central macular field (6×6 mm), ETDRS fields and within each extended ETDRS field (P3-P7).
Results
Macular PD was correlated to NPI in total area of retina (Spearman ρ = 0.69, p < 0.05), posterior pole (ρ = 0.48, p < 0.05), mid-periphery (ρ = 0.65, p < 0.05), far-periphery (ρ = 0.59, p < 0.05), P3-P7 (ρ = 0,55 at least, p < 0.05 for each), central macula (ρ = 0.47, p < 0.05), total area in ETDRS (ρ = 0.55, p < 0.05). Macular VD and FD were correlated to NPI of total area of the retina (ρ = 0.60 and 0.61, p < 0.05), the mid-periphery (ρ = 0.56, p < 0.05) and far-periphery (ρ = 0.60 and ρ = 0.61, p < 0.05), and in P3-P7 (p < 0.05). FAZ perimeter was significantly corelated to NPI at posterior pole and central macular area (ρ = 0.37 and 0.36, p < 0.05), and FAZ area to NPI in central macular area (ρ = 0.36, p < 0.05).
Conclusions
Perfusion macular metrics on OCT-A correlated with UWF-FA’s non-perfusion (NP), particularly in the retina’s mid and far periphery, suggesting that OCT-A might be a useful non-invasive method to estimate peripheral retinal NP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data are not public, but are available from the corresponding author upon reasonable request.
References
Ting DSW, Cheung GCM, Wong TY. Diabetic retinopathy: global prevalence, major risk factors, screening practices and public health challenges: a review. Clin Exp Ophthalmol. 2016;44:260–77. https://doi.org/10.1111/ceo.12696
Niki T, Muraoka K, Shimizu K. Distribution of capillary nonperfusion in early-stage diabetic retinopathy. Ophthalmology. 1984;91:1431–9. https://doi.org/10.1016/S0161-6420(84)34126-4
Shimizu K, Kobayashi Y, Muraoka K. Midperipheral fundus involvement in diabetic retinopathy. Ophthalmology. 1981;88:601–12. https://doi.org/10.1016/S0161-6420(81)34983-5
Silva PS, Cavallerano JD, Sun JK, Soliman AZ, Aiello LM, Aiello LP. Peripheral lesions identified by mydriatic ultrawide field imaging: Distribution and potential impact on diabetic retinopathy severity. Ophthalmology. 2013;120:2587–95. https://doi.org/10.1016/j.ophtha.2013.05.004
Price LD, Au S, Chong NV. Optomap ultrawide field imaging identifies additional retinal abnormalities in patients with diabetic retinopathy. Clin Ophthalmol. 2015;9:527–31. https://doi.org/10.2147/OPTH.S79448
Silva PS, Cavallerano JD, Haddad NM, Kwak H, Dyer KH, Omar AF, et al. Peripheral lesions identified on ultrawide field imaging predict increased risk of diabetic retinopathy progression over 4 years. Ophthalmology. 2015;122:949–56. https://doi.org/10.1016/j.ophtha.2015.01.008
Wessel MM, Aaker GD, Parlitsis G, Cho M, D’Amico DJ, Kiss S. Ultra-wide-field angiography improves the detection and classification of diabetic retinopathy. Retina. 2012;32:785–91. https://doi.org/10.1097/IAE.0b013e3182278b64
Wessel MM, Nair N, Aaker GD, Ehrlich JR, D’Amico DJ, Kiss S. Peripheral retinal ischaemia, as evaluated by ultra-widefield fluorescein angiography, is associated with diabetic macular oedema. Br J Ophthalmol. 2012;96:694–8. https://doi.org/10.1136/bjophthalmol-2011-300774
Fan W, Wang K, Ghasemi Falavarjani K, Sagong M, Uji A, Ip M, et al. Distribution of Nonperfusion Area on Ultra-widefield Fluorescein Angiography in Eyes With Diabetic Macular Edema: DAVE Study. Am J Ophthalmol. 2017;180:110–6. https://doi.org/10.1016/j.ajo.2017.05.024
Patel RD, Messner LV, Teitelbaum B, Michel KA, Hariprasad SM. Characterization of ischemic index using ultra-widefield fluorescein angiography in patients with focal and diffuse recalcitrant diabetic macular edema. Am J Ophthalmol. 2013;155:1038–.e2. https://doi.org/10.1016/j.ajo.2013.01.007
Silva PS, Dela Cruz AJ, Ledesma MG, van Hemert J, Radwan A, Cavallerano JD, et al. Diabetic retinopathy severity and peripheral lesions are associated with nonperfusion on ultrawide field angiography. Ophthalmology. 2015;122:2465–72. https://doi.org/10.1016/j.ophtha.2015.07.034
Silva PS, Liu D, Glassman AR, Aiello LP, Grover S, Kingsley RM, et al. Assessment of fluorescein angiography nonperfusion in eyes with diabetic retinopathy using ultrawide field retinal imaging. Retina. 2022;42:1302–10. https://doi.org/10.1097/IAE.0000000000003479
Ehlers JP, Jiang AC, Boss JD, Hu M, Figueiredo N, Babiuch A, et al. Quantitative ultra-widefield angiography and diabetic retinopathy severity. Ophthalmology. 2019;126:1527–32. https://doi.org/10.1016/j.ophtha.2019.05.034
Silva PS, Marcus DM, Liu D, Aiello LP, Antoszyk A, Elman M, et al. Association of ultra-widefield fluorescein angiography-identified retinal nonperfusion and the risk of diabetic retinopathy worsening over time. JAMA Ophthalmol. 2022;140:936–45. https://doi.org/10.1001/jamaophthalmol.2022.3130
Kwiterovich KA, Maguire MG, Murphy RP, Schachat AP, Bressler NM, Bressler SB, et al. Frequency of adverse systemic reactions after fluorescein angiography. Ophthalmology. 1991;98:1139–42. https://doi.org/10.1016/S0161-6420(91)32165-1
Fineschi V, Monasterolo G, Rosi R, Turillazzi E. Fatal anaphylactic shock during a fluorescein angiography. Forensic Sci Int. 1999;100:137–42. https://doi.org/10.1016/S0379-0738(98)00205-9
Spaide RF, Fujimoto JG, Waheed NK, Sadda SR, Staurenghi G. Optical coherence tomography angiography. Prog Retin Eye Res. 2018;64:1–55. https://doi.org/10.1016/j.preteyeres.2017.11.003
Soares M, Neves C, Marques IP, Pires I, Schwartz C, Costa MÂ, et al. Comparison of diabetic retinopathy classification using fluorescein angiography and optical coherence tomography angiography. Br J Ophthalmol. 2017;101:62–8. https://doi.org/10.1136/bjophthalmol-2016-309424
Rabiolo A, Cicinelli MV, Corbelli E, Baldin G, Carnevali A, Lattanzio R, et al. Correlation analysis between foveal avascular zone and peripheral ischemic index in diabetic retinopathy: a pilot study. Ophthalmol Retin. 2018;2:46–52. https://doi.org/10.1016/j.oret.2017.05.007
Hajdu D, Sedova A, Datlinger F, Hafner J, Steiner I, Kriechbaum K, et al. Association of macular perfusion status with microvascular parameters up to the far periphery in diabetic retinopathy using multimodal imaging. Int J Retin Vitr. 2020;6:1–8. https://doi.org/10.1186/s40942-020-00253-w
Decker NL, Duffy BV, Boughanem GO, Fukuyama H, Castellanos Canales D, Nesper PL, et al. Macular perfusion deficits on OCTA correlate with non-perfusion on ultrawide-field FA in diabetic retinopathy. Ophthalmol Retin. 2023;(Current Opinion in Green and Sustainable Chemistry):100788. https://doi.org/10.1016/j.oret.2023.04.003
Wilkinson CP, Ferris FL 3rd, Klein RE, Lee PP, Agardh CD, Davis M, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110:1677–82. https://doi.org/10.1016/S0161-6420(03)00475-5
Zahid S, Dolz-Marco R, Freund KB, Balaratnasingam C, Dansingani K, Gilani F, et al. Fractal dimensional analysis of optical coherence tomography angiography in eyes with diabetic retinopathy. Invest Ophthalmol Vis Sci. 2016;57:4940–7. https://doi.org/10.1167/IOVS.16-19656
Sim DA, Keane PA, Rajendram R, Karampelas M, Selvam S, Powner MB, et al. Patterns of peripheral retinal and central macula ischemia in diabetic retinopathy as evaluated by ultra-widefield fluorescein angiography. Am J Ophthalmol. 2014;158:144–.e1. https://doi.org/10.1016/j.ajo.2014.03.009
Krawitz BD, Mo S, Geyman LS, Agemy SA, Scripsema NK, Garcia PM, et al. Acircularity index and axis ratio of the foveal avascular zone in diabetic eyes and healthy controls measured by optical coherence tomography angiography. Vis Res. 2017;139:177–86. https://doi.org/10.1016/j.visres.2016.09.019
Spaide RF, Klancnik JM, Cooney MJ. Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol. 2015;133:45–50. https://doi.org/10.1001/jamaophthalmol.2014.3616
Sun Z, Yang D, Tang Z, Ng DS, Cheung CY. Optical coherence tomography angiography in diabetic retinopathy: an updated review. Eye. 2021;35:149–61. https://doi.org/10.1038/s41433-020-01233-y
Or C, Das R, Despotovic I, Alibhai AY, Moult E, Waheed NK, et al. Combined multimodal analysis of peripheral retinal and macular circulation in diabetic retinopathy (COPRA Study). Ophthalmol Retin. 2019;3:580–8. https://doi.org/10.1016/j.oret.2019.03.001
Chen S, Moult EM, Zangwill LM, Weinreb RN, Fujimoto JG. Geometric perfusion deficits: a novel OCT angiography biomarker for diabetic retinopathy based on oxygen diffusion. Am J Ophthalmol. 2021;222:256–70. https://doi.org/10.1016/j.ajo.2020.09.007
Nesper PL, Ong JX, Fawzi AA. Deep capillary geometric perfusion deficits on OCT angiography detect clinically referable eyes with diabetic retinopathy. Ophthalmol Retin. 2022;6:1194–205. https://doi.org/10.1016/j.oret.2022.05.028
Acknowledgements
This work has been supported by the Italian Ministry of Health—Ricerca Corrente—IRCCS MultiMedica.
Author information
Authors and Affiliations
Contributions
SV, RS, PS, TP, FF and PN were responsible for designing the study and interpretation of results. SV and TP contributed to UWF-CF grading; PS was responsible for UWF-FA imaging analysis; ET conducted OCT-A analysis; MB conducted statistical analysis; FF contributed to data extraction and image analysis. All authors contributed to the drafting and reviewing of the manuscript ensuring accuracy and integrity of every part of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vujosevic, S., Fantaguzzi, F., Silva, P.S. et al. Macula vs periphery in diabetic retinopathy: OCT-angiography and ultrawide field fluorescein angiography imaging of retinal non perfusion. Eye (2024). https://doi.org/10.1038/s41433-024-02989-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41433-024-02989-3