Abstract
Background
Socioeconomic deprivation has been associated with lower breast cancer (BC) survival, but the influence of stage at diagnosis on this association merits further study. Our aim was to investigate this association using the Loire-Atlantique/Vendee Cancer Registry (France).
Methods
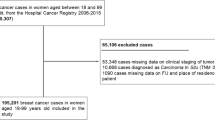
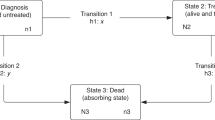
Twelve-thousand seven-hundred thirty-eight women living in the area covered by the registry and diagnosed with invasive breast carcinoma between 2008 and 2015 were included in the study. They were censored at maximal 6 years. Deprivation was measured by the French European Deprivation Index. Excess hazard and net survival were estimated for deprivation level, stage and age at diagnosis using a flexible excess mortality hazard model.
Results
After adjustment by stage, women living in the most deprived areas had a borderline non-significant higher excess mortality hazard (+25% (95% CI: −3%; +62%)) compared to those living in the least deprived areas. Stage-adjusted 5-year net survival differed significantly between these two subgroups (respectively, 88.2% (95% CI:85.2%-90.5%) and 92.5% (95% CI:90.6%-93.9%)).
Conclusion
BC survival remained lower in deprived areas in France, despite universal access to cancer care. Intensification of prevention measures could help to reduce advanced BC, responsible for the majority of deaths from BC. A better understanding of remaining social disparities is crucial to implement specific interventions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
French National Cancer Institute (INCa). Stratégie décennale de lutte contre les cancers 2021–2030 [in French] [Internet]. [cited 2021 Aug 31]. Available from: https://www.e-cancer.fr/Institut-national-du-cancer/Strategie-de-lutte-contre-les-cancers-en-France/La-strategie-decennale-de-lutte-contre-les-cancers-2021-2030
Plan Cancer 2014–2019. Guérir et prévenir les cancers: donnons les mêmes chances à tous, partout en France [in French] [Internet]. [cited 2021 Aug 30]. Available from: https://www.e-cancer.fr/Institut-national-du-cancer/Strategie-de-lutte-contre-les-cancers-en-France/Les-Plans-cancer/Le-Plan-cancer-2014-2019
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Defossez G, Le Guyader-Peyrou S, Uhry Z, Grosclaude P, Remontet L, Colonna M, et al. Estimations nationales de l’incidence et de la mortalité par cancer en France métropolitaine entre 1990 et 2018. Étude à partir des registres des cancers du réseau Francim. Résultats préliminaires. Rapport. [Internet]. Saint-Maurice (Fra): Santé Publique France; 2019 [cited 2021 Jul 21] p. 161. Available from: http://www.santepubliquefrance.fr/
Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–75.
Sant M, Chirlaque Lopez MD, Agresti R, Sánchez Pérez MJ, Holleczek B, Bielska-Lasota M, et al. Survival of women with cancers of breast and genital organs in Europe 1999-2007: results of the EUROCARE-5 study. Eur J Cancer. 2015;51:2191–205.
Molinié F, Trétarre B, Arveux P, Woronoff AS, Lecoffre C, Lafay L, et al. Survie des personnes atteintes de cancer en France métropolitaine 1989-2018—Sein [Internet]. Boulogne-Billancourt (Fra.): Institut national du cancer; 2020 Sept [cited 2021 Jul 21] p. 12. Available from: https://e-cancer.fr/
Bryere J, Tron L, Menvielle G, Launoy G, French Network of Cancer Registries (FRANCIM). The respective parts of incidence and lethality in socioeconomic differences in cancer mortality. An analysis of the French network Cancer registries (FRANCIM) data. Int J Equity Health. 2019;18:189.
Pollock AM, Vickers N. Breast, lung and colorectal cancer incidence and survival in South Thames Region, 1987-1992: the effect of social deprivation. J Public Health Med. 1997;19:288–94.
Walsh PM, Byrne J, Kelly M, McDevitt J, Comber H. Socioeconomic disparity in survival after breast cancer in ireland: observational study. PLoS ONE. 2014;9:e111729.
Deborde T, Chatignoux E, Quintin C, Beltzer N, Hamers FF, Rogel A. Breast cancer screening programme participation and socioeconomic deprivation in France. Prev Med. 2018;115:53–60.
Menvielle G, Rey G, Jougla E, Luce D. Diverging trends in educational inequalities in cancer mortality between men and women in the 2000s in France. BMC Public Health. 2013;13:823.
Ouédraogo S, Dabakuyo-Yonli TS, Roussot A, Pornet C, Sarlin N, Lunaud P, et al. European transnational ecological deprivation index and participation in population-based breast cancer screening programmes in France. Prev Med. 2014;63:103–8.
Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol. 2019;30:1194–220.
Afshar N, English DR, Milne RL. Factors explaining socio-economic inequalities in cancer survival: a systematic review. Cancer Control. 2021;28:10732748211011956.
Booth CM, Li G, Zhang-Salomons J, Mackillop WJ. The impact of socioeconomic status on stage of cancer at diagnosis and survival: a population-based study in Ontario, Canada. Cancer. 2010;116:4160–7.
Kaffashian F, Godward S, Davies T, Solomon L, McCann J, Duffy SW. Socioeconomic effects on breast cancer survival: proportion attributable to stage and morphology. Br J Cancer. 2003;89:1693–6.
Haynes R, Pearce J, Barnett R. Cancer survival in New Zealand: ethnic, social and geographical inequalities. Soc Sci Med. 2008;67:928–37.
Jansen L, Eberle A, Emrich K, Gondos A, Holleczek B, Kajüter H, et al. Socioeconomic deprivation and cancer survival in Germany: an ecological analysis in 200 districts in Germany. Int J Cancer. 2014;134:2951–60.
Schrijvers CT, Mackenbach JP, Lutz JM, Quinn MJ, Coleman MP. Deprivation and survival from breast cancer. Br J Cancer. 1995;72:738–43.
Trewin CB, Johansson ALV, Hjerkind KV, Strand BH, Kiserud CE, Ursin G. Stage-specific survival has improved for young breast cancer patients since 2000: but not equally. Breast Cancer Res Treat. 2020;182:477–89.
Skyrud KD, Bray F, Eriksen MT, Nilssen Y, Møller B. Regional variations in cancer survival: Impact of tumour stage, socioeconomic status, comorbidity and type of treatment in Norway. Int J Cancer. 2016;138:2190–200.
Rutherford MJ, Hinchliffe SR, Abel GA, Lyratzopoulos G, Lambert PC, Greenberg DC. How much of the deprivation gap in cancer survival can be explained by variation in stage at diagnosis: an example from breast cancer in the East of England. Int J Cancer. 2013;133:2192–200.
Kumachev A, Trudeau ME, Chan KKW. Associations among socioeconomic status, patterns of care and outcomes in breast cancer patients in a universal health care system: Ontario’s experience. Cancer. 2016;122:893–8.
Allgood PC, Duffy SW, Kearins O, O’Sullivan E, Tappenden N, Wallis MG, et al. Explaining the difference in prognosis between screen-detected and symptomatic breast cancers. Br J Cancer. 2011;104:1680–5.
Li R, Daniel R, Rachet B. How much do tumor stage and treatment explain socioeconomic inequalities in breast cancer survival? Applying causal mediation analysis to population-based data. Eur J Epidemiol. 2016;31:603–11.
Finke I, Behrens G, Maier W, Schwettmann L, Pritzkuleit R, Holleczek B, et al. Small-area analysis on socioeconomic inequalities in cancer survival for 25 cancer sites in Germany. Int J Cancer. 2021;149:561–72.
Zadnik V, Žagar T, Tomšič S, Mihor A, Lokar K. Cancer Patients’ Survival According to Socioeconomic Environment in a High-Income Country with Universal Health Coverage. Cancers (Basel). 2022;14:1620.
Pornet C, Delpierre C, Dejardin O, Grosclaude P, Launay L, Guittet L, et al. Construction of an adaptable European transnational ecological deprivation index: the French version. J Epidemiol Community Health. 2012;66:982–9.
Poiseuil M, Tron L, Woronoff AS, Trétarre B, Dabakuyo-Yonli TS, Fauvernier M, et al. How do age and social environment affect the dynamics of death hazard and survival in patients with breast or gynecological cancer in France? Int J Cancer. 2021;68:1233–57.
Tron L, Belot A, Fauvernier M, Remontet L, Bossard N, Launay L, et al. Socioeconomic environment and disparities in cancer survival for 19 solid tumor sites: An analysis of the French Network of Cancer Registries (FRANCIM) data. Int J Cancer. 2019;144:1262–74.
Sobin LH, Gosporadowicz MK, Wittelkind C. TNM classification of malignant tumors. 7th ed. 2011. https://www.amazon.com/Classification-Malignant-Tumours-Leslie-Sobin/dp/1444332414
Guillaume E, Pornet C, Dejardin O, Launay L, Lillini R, Vercelli M, et al. Development of a cross-cultural deprivation index in five European countries. J Epidemiol Community Health. 2016;70:493–9.
Cancers & Preventions—UMR 1086 UCN.Caen. Plate-forme méthodologique nationale pour l’étude et la réduction des inégalités sociales en cancérologie (ERISC). [cited 2021 Dec 12]. Available from: http://cancerspreventions.fr/inegalites-sociales/plateforme-2/
Estève J, Benhamou E, Croasdale M, Raymond L. Relative survival and the estimation of net survival: elements for further discussion. Stat Med. 1990;9:529–38.
Fauvernier M, Roche L, Uhry Z, Tron L, Bossard N, Remontet L, et al. Multi‐dimensional penalized hazard model with continuous covariates: applications for studying trends and social inequalities in cancer survival. J R Stat Soc C. 2019;68:1233–57. https://onlinelibrary.wiley.com/doi/10.1111/rssc.12368
Remontet L, Uhry Z, Bossard N, Iwaz J, Belot A, Danieli C, et al. Flexible and structured survival model for a simultaneous estimation of non-linear and non-proportional effects and complex interactions between continuous variables: Performance of this multidimensional penalized spline approach in net survival trend analysis. Stat Methods Med Res. 2019;28:2368–84.
Fauvernier M, Remontet L, Uhry Z, Bossard N, Roche L. survPen: an R package for hazard and excess hazard modelling with multidimensional penalized splines. J Open Source Softw. 2019;4:1434 https://joss.theoj.org/papers/10.21105/joss.01434
ALD [Internet]. [cited 2022 Aug 11]. Available from: https://www.ameli.fr/assure/droits-demarches/maladie-accident-hospitalisation/affection-longue-duree-ald/affection-longue-duree-maladie-chronique
Sicsic J, Franc C. Obstacles to the uptake of breast, cervical, and colorectal cancer screenings: what remains to be achieved by French national programmes? BMC Health Serv Res. 2014;14:465.
Duport N. Characteristics of women using organized or opportunistic breast cancer screening in France. Analysis of the 2006 French Health, Health Care and Insurance Survey. Rev Epidemiol Sante Publique. 2012;60:421–30.
Ferrat E, Le Breton J, Djassibel M, Veerabudun K, Brixi Z, Attali C, et al. Understanding barriers to organized breast cancer screening in France: women’s perceptions, attitudes, and knowledge. Fam Pract. 2013;30:445–51.
Redig AJ, McAllister SS. Breast cancer as a systemic disease: a view of metastasis. J Intern Med. 2013;274:113–26.
Thomson CS, Hole DJ, Twelves CJ, Brewster DH, Black RJ, Scottish Cancer Therapy Network. Prognostic factors in women with breast cancer: distribution by socioeconomic status and effect on differences in survival. J Epidemiol Community Health. 2001;55:308–15.
Aarts MJ, Hamelinck VC, Bastiaannet E, Coebergh JWW, Liefers GJ, Voogd AC, et al. Small but significant socioeconomic inequalities in axillary staging and treatment of breast cancer in the Netherlands. Br J Cancer. 2012;107:12–7.
Lamy S, Molinié F, Daubisse-Marliac L, Cowppli-Bony A, Ayrault-Piault S, Fournier E, et al. Using ecological socioeconomic position (SEP) measures to deal with sample bias introduced by incomplete individual-level measures: inequalities in breast cancer stage at diagnosis as an example. BMC Public Health. 2019;19:857.
Bryere J, Pornet C, Copin N, Launay L, Gusto G, Grosclaude P, et al. Assessment of the ecological bias of seven aggregate social deprivation indices. BMC Public Health. 2017;17:86.
DeRouen MC, Schupp CW, Koo J, Yang J, Hertz A, Shariff-Marco S, et al. Impact of individual and neighborhood factors on disparities in prostate cancer survival. Cancer Epidemiol. 2018;53:1–11.
Hagedoorn P, Vandenheede H, Vanthomme K, Gadeyne S. Socioeconomic position, population density and site-specific cancer mortality: a multilevel analysis of Belgian adults, 2001-2011. Int J Cancer. 2018;142:23–35.
Diez Roux AV. A glossary for multilevel analysis. J Epidemiol Community Health. 2002;56:588–94.
Dalton SO, Olsen MH, Johansen C, Olsen JH, Andersen KK. Socioeconomic inequality in cancer survival—changes over time. A population-based study, Denmark, 1987-2013. Acta Oncol. 2019;58:737–44.
Acknowledgements
We would like to thank those who provided data to the registry: pathologists (CHD Vendée, CH Saint-Nazaire, CHU Nantes, IHP group, Kerlo-Morin laboratory, CRLCC Nantes-Angers, CHU Angers, laboratories from Ille-et-Vilaine and Nouvelle-Aquitaine), oncologists, public and private hospital medical data processing departments, and medical practitioners as well as the medical departments of the national health insurance programmes, the screening coordination centre and Cancer Regional Network. We would like to thank ERISC/MapInMed platform (French national methodological platform for the study and reduction of health social inequalities in oncology) for the attribution of F-EDI value.
Funding
This work was prepared within the framework of the SIRIC ILIAD programme supported by the French National Cancer Institute (INCa), the French Ministry of Health, and the Institute of Health and Medical Research (INSERM); SIRIC ILIAD INCa-DGOS-Inserm_12558 grant. The Loire-Atlantique/Vendee Cancer Registry is supported for the routine collection of data by the French National Cancer Institute (INCa), Santé Publique France, Direction Générale de l’Offre de Soins (DGOS), local institutions (Conseil Régional des Pays de la Loire, ARS des Pays de la Loire, CHU Nantes, CHD Vendée, Institut de Cancérologie de l’Ouest) and the League Against Cancer (comités de Loire-Atlantique et de Vendée).
Author information
Authors and Affiliations
Contributions
FM, ACB had the idea for the study. C Delacôte, SD, SAY, ACB, FM contributed to the conception and design of the analysis. ADT, GR, MV, SA collected the data. C Delacôte performed the analysis. C Delacôte, SD, SAY, C Delpierre, ACB, FM contributed to the interpretation. The first draft of the work was written by C Delacôte and all authors commented on previous versions of the manuscript. All authors revised the manuscript critically for important intellectual content and approved the final version for publication. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study is based on data from the Loire-Atlantique/Vendee Cancer Registry, a member of the French network of cancer registries (FRANCIM). It has received the approval of the French regulatory authorities for the collection and analysis of medical data: the Comité Consultatif sur le Traitement de l’Information en matière de Recherche dans le Domaine de la Santé (ethical approval) and the Commission Nationale Informatique et Libertés (legal framework and data protection). In conformity with French law, patients were informed individually of the nature of the information provided, the purpose of data processing, their right of access, rectification and objection. The ethics committee, in accordance with French law, did not request informed consent. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or a comparable ethical standard. All methods were performed in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Delacôte, C., Delacour-Billon, S., Ayrault-Piault, S. et al. Is survival rate lower after breast cancer in deprived women according to disease stage?. Br J Cancer 128, 63–70 (2023). https://doi.org/10.1038/s41416-022-02024-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-02024-w