Abstract
Study design
Retrospective comparative study.
Objective
This study aimed to determine whether the degree of preoperative gait disturbance remains following surgical resection in patients with intradural extramedullary spinal cord tumors (IDEMSCTs), and to investigate any factors that may influence poor improvement in postoperative gait disturbance.
Setting
The single institution in Japan.
Methods
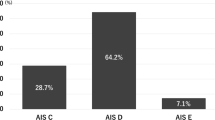
In total, 78 IDEMSCTs patients who required surgical excision between 2010 and 2019 were included. According to the degree of preoperative gait disturbance using modified McCormick scale (MMCS) grade, they were divided into the Mild and Severe groups. The mean postoperative follow-up period was 50.7 ± 17.9 months. Data on demographic and surgical characteristics were compared between the two groups.
Results
There was no significant difference in terms of age at surgery, sex, tumor size, surgical time, estimated blood loss, tumor histopathology, and postoperative follow-up period between the Mild and Severe groups. At the final follow-up, 84.6% of IDEMSCTs patients were able to walk without support. Gait disturbance improved after surgery in most of the patients with preoperative MMCS grades II–IV, but remained in approximately half of patients with preoperative MMCS grade V. Age at surgery was correlated with poor improvement in postoperative gait disturbance in the Severe group.
Conclusions
Regardless of the degree of preoperative gait disturbance, it improved after tumor resection in most of the IDEMSCTs patients. However, in the preoperative MMCS grade III–V cases, older age at surgery would be an important factor associated with poor improvement in postoperative gait disturbance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated and/or analyzed in this study are available from the corresponding author on request.
References
Özkan N, Jabbarli R, Wrede KH, Sariaslan Z, Stein KP, Dammann P, et al. Surgical management of intradural spinal cord tumors in children and young adults: a single-center experience with 50 patients. Surg Neurol Int. 2015;6:S661–7.
Abul-Kasim K, Thurnher MM, McKeever P, Sundgren PC. Intradural spinal tumors: current classification and MRI features. Neuroradiology. 2008;50:301–14.
Nambiar M, Kavar B. Clinical presentation and outcome of patients with intradural spinal cord tumours. J Clin Neurosci. 2012;19:262–6.
Bellut D, Mutter UM, Sutter M, Eggspuehler A, Mannion AF, Porchet F. Back pain in patients with degenerative spine disease and intradural spinal tumor: what to treat? when to treat? Eur Spine J. 2014;23:821–9.
Mehta AI, Adogwa O, Karikari IO, Thompson P, Verla T, Null UT, et al. Anatomical location dictating major surgical complications for intradural extramedullary spinal tumors: a 10-year single-institutional experience. J Neurosurg Spine. 2013;19:701–7.
Arora RK, Kumar R. Spinal tumors: trends from Northern India. Asian J Neurosurg. 2015;10:291–7.
Bhimani AD, Denyer S, Esfahani DR, Zakrzewski J, Aguilar TM, Mehta AI. Surgical complications in intradural extramedullary spinal sord tumors—an ACS-NSQIP analysis of spinal cord level and malignancy. World Neurosurg. 2018;117:e290–9.
Cofano F, Giambra C, Costa P, Zeppa P, Bianconi A, Mammi M, et al. Management of extramedullary intradural spinal tumors: the impact of clinical status, intraoperative neurophysiological monitoring and surgical approach on outcomes in a 12-year double-center experience. Front Neurol. 2020;11:598619.
Riad H, Knafo S, Segnarbieux F, Lonjon N. Spinal meningiomas: surgical outcome and literature review. Neurochirurgie. 2013;59:30–4.
Jenkinson MD, Simpson C, Nicholas RS, Miles J, Findlay GF, Pigott TJ. Outcome predictors and complications in the management of intradural spinal tumours. Eur Spine J. 2006;15:203–10.
Wach J, Banat M, Schuss P, Güresir E, Vatter H, Scorzin J. Age at diagnosis and baseline myelomalacia sign predict functional outcome after spinal meningioma surgery. Front Surg. 2021;8:682930.
Baro V, Moiraghi A, Carlucci V, Paun L, Anglani M, Ermani M, et al. Spinal meningiomas: influence of cord compression and radiological features on preoperative functional status and outcome. Cancers. 2021;13:4183.
Ando K, Kobayashi K, Nakashima H, Machino M, Ito S, Kanbara S, et al. Surgical outcomes and factors related to postoperative motor and sensory deficits in resection for 244 cases of spinal schwannoma. J Clin Neurosci. 2020;81:6–11.
Song KW, Shin SI, Lee JY, Kim GL, Hyun YS, Park DY. Surgical results of intradural extramedullary tumors. Clin Orthop Surg. 2009;1:74–80.
Conti P, Pansini G, Mouchaty H, Capuano C, Conti R. Spinal neurinomas: retrospective analysis and long-term outcome of 179 consecutively operated cases and review of the literature. Surg Neurol. 2004;61:34–44.
Safavi-Abbasi S, Senoglu M, Theodore N, Workman RK, Gharabaghi A, Feiz-Erfan I, et al. Microsurgical management of spinal schwannomas: evaluation of 128 cases. J Neurosurg Spine. 2008;9:40–7.
Yang C, Li G, Fang J, Wu L, Yang T, Deng X, et al. Clinical characteristics and surgical outcomes of primary spinal paragangliomas. Neurooncology. 2015;122:539–47.
Tuleasca C, Al-Risi AS, David P, Adam C, Aghakhani N, Parker F, et al. Paragangliomas of the spine: a retrospective case series in a national reference French center. Acta Neurochir. 2020;162:831–7.
Imagama S, Ito Z, Ando K, Kobayashi K, Hida T, Ito K. Optimal timing of surgery for intramedullary cavernous hemangioma of the spinal cord in relation to preoperative motor paresis, disease duration, and tumor volume and location. Glob Spine J. 2017;7:246–53.
McCormick JD, Werner BC, Shimer AL. Patient-reported outcome measures in spine surgery. J Am Acad Orthop Surg. 2013;21:99–107.
Kucia EJ, Maughan PH, Kakarla UK, Bambakidis NC, Spetzler RF. Surgical technique and outcomes in the treatment of spinal cord ependymomas: part II: myxopapillary ependymoma. Neurosurgery. 2011;68:90–4.
Okubo T, Nagoshi N, Tsuji O, Tachibana A, Kono H, Suzuki S, et al. Imaging characteristics and surgical outcomes in patients with intraspinal solitary fibrous tumor/hemangiopericytoma: a retrospective cohort study. Glob Spine J. 2021;11:2192568221994799.
Corell A, Cerbach C, Hoefling N, Björkman-Burtscher IM, Jakola AS. Spinal cord compression in relation to clinical symptoms in patients with spinal meningiomas. Clin Neurol Neurosurg. 2021;211:107018.
Mohme M, Mende KC, Krätzig T, Plaetke R, Beseoglu K, Hagedorn J, et al. Impact of spinal cord compression from intradural and epidural spinal tumors on perioperative symptoms-implications for surgical decision making. Neurosurg Rev. 2017;40:377–87.
Nagoshi N, Tsuji O, Suzuki S, Nori S, Yagi M, Okada E, et al. Clinical outcomes and a therapeutic indication of intramedullary spinal cord astrocytoma. Spinal Cord. 2022;60:216–22.
Zuckerman SL, Chotai S, Devin CJ, Parker SL, Stonko DP, Wick JB, et al. Surgical resection of intradural extramedullary spinal tumors: patient reported outcomes and minimum clinically important difference. Spine. 2016;41:1925–32.
Newman WC, Berry-Candelario J, Villavieja J, Reiner AS, Bilsky MH, Laufer I, et al. Improvement in quality of life following surgical resection of benign intradural extramedullary tumors: a prospective evaluation of patient-reported outcomes. Neurosurgery. 2021;15:989–95.
Mannion AF, Porchet F, Kleinstück FS, Lattig F, Jeszenszky D, Bartanusz V, et al. The quality of spine surgery from the patient’s perspective. Part 1: the Core Outcome Measures Index in clinical practice. Eur Spine J. 2009;18:367–73.
Guirado VM, Taricco MA, Nobre MR, Couto EB Jr, Ribas ES, Meluzzi A, et al. Quality of life in adult intradural primary spinal tumors: 36-item short form health survey correlation with McCormick and Aminoff-Logue scales. J Neurosurg Spine. 2013;19:721–35.
Bellut D, Burkhardt JK, Mannion AF, Porchet F. Assessment of outcome in patients undergoing surgery for intradural spinaltumor using the multidimensional patient-rated core outcome measures index and the modified McCormick scale. Neurosurg Focus. 2015;39:E2.
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for the English language review.
Author information
Authors and Affiliations
Contributions
TO collected and interpreted the data, and wrote the initial draft of this manuscript. KF, YK, and KM assisted in the preparation of the manuscript. TO designed the study, and TK, MF, TA, and YY critically reviewed the manuscript. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work to ensure that questions associated with the accuracy or integrity of any part of the work were appropriately evaluated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
We certify that all applicable governmental and institutional regulations concerning the ethical use of human volunteers were followed during the course of this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Okubo, T., Fujiyoshi, K., Kobayashi, Y. et al. Does the degree of preoperative gait disturbance remain after tumor resection in patients with intradural extramedullary spinal cord tumors?. Spinal Cord 61, 637–643 (2023). https://doi.org/10.1038/s41393-023-00931-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-023-00931-0