Abstract
Study design
Prospective cohort study.
Objectives
The aim of this study was to evaluate how time since spinal cord injury/disorder (SCI/D) and patients’ age influence risk constellation for hospital acquired pressure injuries (HAPI) in patients with a SCI/D.
Setting
Acute care and rehabilitation clinic specialized in SCI/D.
Methods
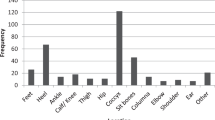
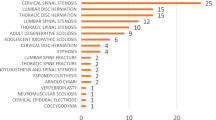
We collected patients’ characteristics and 85 risk factors for HAPI development in adults with SCI/D with at least one HAPI during their inpatient stay between August 2018 and December 2019. We analyzed patients’ characteristics and HAPI risk factors using descriptive statistics according to time since SCI/D ( < 1 year, 1–15 years, > 15 years) and patients’ age (18–35 years, 35–65 years, > 65 years).
Results
We identified 182 HAPI in 96 patients. Comparing patients with SCI/D < 1 year with the other groups, autonomic dysreflexia (p < 0.001), abnormal body temperature (p = 0.001), hypertensive episode (p = 0.005), and pneumonia (p < 0.001) occurred more frequently; mean hemoglobin (p < 0.001), albumin (p = 0.002) and vitamin D levels (p = 0.013) were significantly lower, and patients with time since SCI/D < 1 year scored fewer points (10–12) on the Braden Scale (p < 0.001). Comparing groups per patients’ age, only the SCIPUS score was higher in patients > 65 years compared to the other two groups (p = 0.002).
Conclusions
Different risk factor constellation seem to be underlying HAPI development with more differences in patients time since SCI/D than patients’ age. Awareness of these differences in risk factor constellation depending on time since SCI/D in these patients might lead to different HAPI prevention strategies.
Sponsorship
The study team didn't receive any additional sponsorship.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All data are stored by the corresponding author and can be requested individually from the corresponding author.
References
Brinkhof MWG, Al-Khodairy A, Eriks-Hoogland I, Fekete CH, Hinrichs T, Hund-Georgiadis M, et al. for the SwiSCI Study Group., Health conditions in people with spinal cord injury: Contemporary evidence from a population-based community survey in Switzerland. J Rehab Med. 2016;48:197–209.
Stillman MD, Barber J, Burns S, Williams S, Hoffman JM. Complications of Spinal Cord Injury Over the First Year After Discharge From Inpatient Rehabilitation. Arch Phys Med Rehabil. 2017;98:1800–5.
Sezer N, Akkuş S, Uğurlu FG. Chronic complications of spinal cord injury. World J Orthop. 2015;6:24–33.
Hagen EM. Acute complications of spinal cord injuries. World J Orthop. 2015;6:17–23.
Guidelines, C.f.S.C.M.C.P. Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care professionals. J spinal cord Med. 2001;24:S40.
Lupe L, Zambrana D, Cooper L. Prevention of hospital-acquired pressure ulcers in the operating room and beyond: a successful monitoring and intervention strategy program. Int Anesthesiol Clin. 2013;51:128–46.
Shiferaw WS, Akalu TY, Mulugeta H, Aynalem YA. The global burden of pressure ulcers among patients with spinal cord injury: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2020;21:334.
Padula WV, Mishra MK, Makic MB, Sullivan PW. Improving the quality of pressure ulcer care with prevention: a cost-effectiveness analysis. Med Care. 2011;49:385–92.
Kruger, EA, Pires M, Ngann Y, Sterling M, Rubayi S. Comprehensive management of pressure ulcers in spinal cord injury: Current concepts and future trends. 2013.
Scheel-Sailer A, Wyss A, Boldt C, Post MW, Lay V. Prevalence, location, grade of pressure ulcers and association with specific patient characteristics in adult spinal cord injury patients during the hospital stay: a prospective cohort study. Spinal Cord. 2013;51:828–33.
Verschueren JH, Post MW, de Groot S, van der Woude LH, van Asbeck FW, Rol M. Occurrence and predictors of pressure ulcers during primary in-patient spinal cord injury rehabilitation. Spinal Cord. 2011;49:106–12.
van der Wielen H, Post MW, Lay V, Gläsche K, Scheel-Sailer A. Hospital-acquired pressure ulcers in spinal cord injured patients: time to occur, time until closure and risk factors. Spinal Cord. 2016;54:726–31.
Bergstrom N, Braden BJ, Laguzza A, Holman V. The Braden scale for predicting pressure sore risk. Nurs Res. 1987;36:205–10.
Anthony D, Parboteeah S, Saleh M, Papanikolaou P. Norton, Waterlow and Braden scores: a review of the literature and a comparison between the scores and clinical judgement. J Clin Nurs. 2008;17:646–53.
Salzberg CA, Byrne DW, Cayten CG, van Niewerburgh P, Murphy JG, Viehbeck M. A new pressure ulcer risk assessment scale for individuals with spinal cord injury. Am J Phys Med Rehabil. 1996;75:96–104.
Mortenson WB, Miller WC. A review of scales for assessing the risk of developing a pressure ulcer in individuals with SCI. Spinal Cord. 2008;46:168–75.
Afridi A, Rathore FA. Are Risk Assessment Tools Effective for the Prevention of Pressure Ulcers Formation?: A Cochrane Review Summary With Commentary. Am J Phys Med Rehabil. 2020;99:357–8.
Marin J, Nixon J, Gorecki C. A systematic review of risk factors for the development and recurrence of pressure ulcers in people with spinal cord injuries. Spinal Cord. 2013;51:522–7.
Saunders LL, Krause JS. Personality and Behavioral Predictors of Pressure Ulcer History. Top Spinal Cord Inj Rehabil. 2010;16:61–71.
Morita T, Yamada T, Watanabe T, Nagahori E. Lifestyle risk factors for pressure ulcers in community-based patients with spinal cord injuries in Japan. Spinal Cord. 2015;53:476–81.
Najmanova K, Neuhauser C, Krebs J, Baumberger M, Schaefer DJ, Sailer CO, et al. Risk factors for hospital acquired pressure injury in patients with spinal cord injury during first rehabilitation: prospective cohort study. Spinal Cord. 2022;60:45–52.
Scheel-Sailer A, Plattner CH, Flückiger B, Ling B, Schaefer DJ, Baumberger M, et al. Dekubitus – ein Update. Schweiz Med Forum. 2016;16:489–98.
Meier C, Boes S, Gemperli A, Gmünder HP, Koligi K, Metzger S, et al. Treatment and cost of pressure injury stage III or IV in four patients with spinal cord injury: the Basel Decubitus Concept. Spinal cord Ser cases. 2019;5:30.
Rigazzi J, Fähndrich C, Osinga R, Baumgartner S, Baumberger M, Krebs J, et al. Osteomyelitis and antibiotic treatment in patients with grade IV pressure injury and spinal cord lesion-a retrospective cohort study. Spinal Cord. 2022;60:540–7.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Hemkens LG, Moher D, et al. RECORD Working Committee., The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12:e1001885.
Krassioukov A, Biering-Sørensen F, Donovan W, Kennelly M, Kirshblum S, Krogh K, et al. Autonomic Standards Committee of the American Spinal Injury Association/International Spinal Cord Society., International standards to document remaining autonomic function after spinal cord injury. J spinal cord Med. 2012;35:201–10.
Chen Y, Devivo MJ, Jackson AB. Pressure ulcer prevalence in people with spinal cord injury: age-period-duration effects. Arch Phys Med Rehabil. 2005;86:1208–13.
Eslami V, Saadat S, Habibi Arejan R, Vaccaro AR, Ghodsi SM, Rahimi-Movaghar V. Factors associated with the development of pressure ulcers after spinal cord injury. Spinal Cord 2012;50:899–903. https://doi.org/10.1038/sc.2012.75.
R Core Team (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL. https://www.R-project.org/.
Liu X, Zhang Y, Wang Y, Qian T. Inflammatory Response to Spinal Cord Injury and Its Treatment. World Neurosurg. 2021;155:19–31.
Kessler TM, Traini LR, Welk B, Schneider MP, Thavaseelan J, Curt A. Early neurological care of patients with spinal cord injury. World J Urol. 2018;36:1529–36.
Kirshblum S, Snider B, Eren F, Guest J. Characterizing Natural Recovery after Traumatic Spinal Cord Injury. J Neurotrauma. 2021;38:1267–84.
Buchtler K, Carrard V, Jochum H, Ledermann K, Lude P, Scheel-Sailer A. Body experience during post-acute rehabilitation in individuals after a traumatic spinal cord injury: a qualitative interview-based pilot study. Spinal Cord Ser Cases. 2021;7:14.
Ma Y, de Groot S, Romviel S, Achterberg W, van Orsouw L, Janssen TWJ. Changes in body composition during and after inpatient rehabilitation in people with recent spinal cord injury. Spinal Cord Ser Cases. 2021;7:88.
Krassioukov A. Autonomic function following cervical spinal cord injury. Respir Physiol Neurobiol. 2009;169:157–64.
Wecht JM, Krassioukov AV, Alexander M, Handrakis JP, McKenna SL, Kennelly M, et al. AA, Previnaire JG, Rodriguez GM, Slocum C, Wilson JR., International Standards to document Autonomic Function following SCI (ISAFSCI): Second Edition. Top Spinal Cord Inj Rehabil. 2021;27:23–49.
Flueck JL, Perret C. Vitamin D deficiency in individuals with a spinal cord injury: a literature review. Spinal Cord. 2017;55:428–34.
Zanini, C, Brach M, Lustenberger N, Scheel-Sailer A, Koch HG, Stucki G, et al. Engaging in the prevention of pressure injuries in spinal cord injury: A qualitative study of community-dwelling individuals’ different styles of prevention in Switzerland. J Spinal Cord Med. 2020;43:247–56.
Acknowledgements
We thank the “Decu Care Team” (Jessica Decker, Eva Kissling, Rita Müller, Diana Sigrist-Nix, Ivonne Zamzow) for assistance with data collection and Karin Gläsche as the main supervising and responsible nurse. A special recognition goes to Stefanie Tesini for the composition of the database.
Author information
Authors and Affiliations
Contributions
CN: study design, data collection, data interpretation, manuscript preparation and revision. COS: study design, data analysis and interpretation, manuscript preparation and revision. KN: study design, data collection, manuscript revision. MB, DJS, RW: study design, manuscript revision. DP-G: data analysis and interpretation, manuscript revision. AS-S: study design, data collection, data interpretation, manuscript preparation and revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committees of Northwest and Central Switzerland on (protocol code EKNZ ID 2019-02179, date of approval 25th November 2019).
Informed consent
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Neuhauser, C., Sailer, C.O., Najmanova, K. et al. Risk constellation of hospital acquired pressure injuries in patients with a spinal cord injury/ disorder - focus on time since spinal cord injury/ disorder and patients’ age. Spinal Cord 61, 453–459 (2023). https://doi.org/10.1038/s41393-023-00910-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-023-00910-5