Abstract
Study design
A retrospective cohort study.
Objectives
To describe antibiotic prescribing and urine culture testing patterns for urinary tract infections (UTIs) in a primary care Spinal Cord Injury (SCI) cohort.
Setting
A primary care electronic medical records (EMR) database in Ontario.
Methods
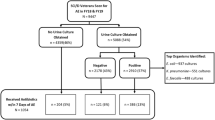
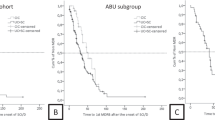
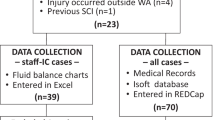
Using linked EMR health administrative databases to identify urine culture and antibiotic prescriptions ordered in primary care for 432 individuals with SCI from January 1, 2013 to December 31, 2015. Descriptive statistics were conducted to describe the SCI cohort, and physicians. Regression analyses were conducted to determine patient and physician factors associated with conducting a urine culture and class of antibiotic prescription.
Results
The average annual number of antibiotic prescriptions for UTI for the SCI cohort during study period was 1.9. Urine cultures were conducted for 58.1% of antibiotic prescriptions. Fluroquinolones and nitrofurantoin were the most frequently prescribed antibiotics. Male physicians and international medical graduates were more likely to prescribe fluroquinolones than nitrofurantoin for UTIs. Early-career physicians were more likely to order a urine culture when prescribing an antibiotic. No patient characteristics were associated with obtaining a urine culture or antibiotic class prescription.
Conclusion
Nearly 60% of antibiotic prescriptions for UTIs in the SCI population were associated with a urine culture. Only physician characteristics, not patient characteristics, were associated with whether or not a urine culture was conducted, and the class of antibiotic prescribed. Future research should aim to further understand physician factors with antibiotic prescribing and urine culture testing for UTIs in the SCI population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The dataset from this study is held securely in coded form at ICES. While legal data sharing agreements between ICES and data providers prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS (email: das@ices.on.ca). The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
References
Abbasi F, Korooni S. Infectious complications after spinal cord injury. In: Dionyssiotis Y (ed). Essentials of Spinal Cord Injury Medicine. InTech, 2018. https://doi.org/10.5772/intechopen.72783.
Siroky MB. Pathogenesis of bacteriuria and infection in the spinal cord injured patient. Am J Med. 2002;113:67–79.
Pannek J. Treatment of urinary tract infection in persons with spinal cord injury: guidelines, evidence, and clinical practice: a questionnaire-based survey and review of the literature. J Spinal Cord Med. 2011;34:11–5.
Bonkat G, Pickard R, Bartoletti R, Bruyère F, Geerlings SE, Wagenlehner F, et al. EAU guidelines on urological infections: In: EAU Guidelines, edition presented at the annual EAU Congress London 2017.
Milligan J, Goetz LL, Kennelly MJ. A primary care provider’s guide to management of neurogenic lower urinary tract dysfunction and urinary tract infection after spinal cord injury. Top Spinal Cord Inj Rehabilit. 2020;26:108–15.
Kavanagh A, Baverstock R, Campeau L, Carlson K, Cox A, Hickling D, et al. Canadian urological association guideline: diagnosis, management, and surveillance of neurogenic lower urinary tract dysfunction - Full text. CUAJ. 2019;13. https://doi.org/10.5489/cuaj.5912.
Craven BC, Alavinia SM, Gajewski JB, Parmar R, Disher S, Ethans K, et al. Conception and development of Urinary Tract Infection indicators to advance the quality of spinal cord injury rehabilitation: SCI-High Project. J Spinal Cord Med. 2019;42:205–14.
Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 international clinical practice guidelines from the infectious diseases society of America. Clin Infect Dis. 2010;50:625–63.
Everaert K, Lumen N, Kerckhaert W, Willaert P, van Driel M. Urinary tract infections in spinal cord injury: prevention and treatment guidelines. Acta Clin Belgica. 2009;64:335–40.
Garfield FB, Garfield JM. Clinical judgment and clinical practice guidelines. J Inter Tech Health Care. 2000;16:1050–60.
Garcia-Arguello LY, O’Horo JC, Farrell A, Blakney R, Sohail MR, Evans CT, et al. Infections in the spinal cord-injured population: a systematic review. Spinal Cord. 2017;55:526–34.
Nygaard Jensen J, Melander E, Hedin K, Bjerrum L, Kornfält Isberg H, Holm A, et al. Comparison of antibiotic prescribing and antimicrobial resistance in urinary tract infections at the municipal level among women in two Nordic regions. J Antimicrobial Chemother. 2018;73:2207–14.
Bruyndonckx R, Hens N, Aerts M, Goossens H, Cortiñas Abrahantes J, Coenen S. Exploring the association between resistance and outpatient antibiotic use expressed as DDDs or packages. J Antimicrobial Chemother. 2015;70:1241–4.
Senthinathan A. Outpatient antibiotic prescribing, dispensing and susceptibility testing in a primary care spinal cord injury cohort [dissertation]. Toronto (Canada): University of Toronto; 2022.
Shepherd J. Identifying cases of spinal cord injury/disorder in an Ontario primary care electronic medical record database [thesis]. Toronto (Canada): University of Toronto; 2020.
Shepherd J, Tu K, Young J, Chishtie J, Craven BC, Moineddin R, et al. Identifying cases of spinal cord injury or disease in a primary care electronic medical record database. J Spinal Cord Med. 2021;44:S28–39.
Senthinathan A .Using clinical vignettes and a modified expert delphi panel to determine parameters for identifying non-traumatic spinal cord injury in health administrative and electronic medical record databases. https://doi.org/10.1016/j.apmr.2022.08.002.
Schull MJ, Azimaee M, Marra M, Cartagena R, Vermulen M, Ho M, et al. ICES: data, discovery. Better Health. Int J Popul Data Sci. 2020;4:1–9.
Lucas G, Bielska IA, Fong R, Johnson AP. Rural–urban differences in use of health care resources among patients with ankle sprains in Ontario. Can J Rural Med. 2018;23:7–14.
Schwartz KL, Wilton AS, Langford BJ, Brown KA, Daneman N, Garber G, et al. Comparing prescribing and dispensing databases to study antibiotic use: a validation study of the Electronic Medical Record Administrative data Linked Database (EMRALD). J Antimicrob Chemother. 2019;74:2091–7.
Fernandez-Lazaro CI, Brown KA, Langford BJ, Daneman N, Garber G, Schwartz KL. Late-career physicians prescribe longer courses of antibiotics. Clin Infect Dis. 2019;69:1467–75.
Ruz AED, Leoni EG, Cabrera RH. Epidemiology and risk factors for urinary tract infection in patients with spinal cord injury. J Urol. 2000;164:1285–9.
Haldrup S, Thomsen RW, Bro F, Skov R, Bjerrum L, Søgaard M. Microbiological point of care testing before antibiotic prescribing in primary care: considerable variations between practices. BMC Fam Pr. 2017;18:9.
Lee J, Varghese J, Brooks R, Turpen BJ. A primary care provider’s guide to accessibility after spinal cord injury. Top Spinal Cord Inj Rehabilit. 2020;26:79–84.
Milligan J, Lee J, Smith M, Donaldson L, Athanasopoulos P, Bassett-Spiers K, et al. Advancing primary and community care for persons with spinal cord injury: Key findings from a Canadian summit. J Spinal Cord Med. 2020;43:223–33.
McColl MA, Aiken A, McColl A, Sakakibara B, Smith K. Primary care of people with spinal cord injury: scoping review. Can Fam Physician. 2012;58:1207–16.
Daneman N, Campitelli MA, Giannakeas V, Morris AM, Bell CM, Maxwell CJ, et al. Influences on the start, selection and duration of treatment with antibiotics in long-term care facilities. CMAJ. 2017;189:E851–60.
Safaeian L, Salami S, Pakmehr F, Mahdanian A-R, Mansourian M. Seasonality and physician-related factors associated with antibiotic prescribing: a cross-sectional study in Isfahan, Iran. Int J Prev Med. 2015;6:1.
Harris JM, Novalis-Marine C, Harris RB. Women physicians are early adopters of on-line continuing medical education. J Continuing Educ Health Prof. 2003;23:221–8.
Evans CT, Rogers TJ, Weaver FM, Burns SP. Providers’ beliefs and behaviors regarding antibiotic prescribing and antibiotic resistance in persons with spinal cord injury or disorder. J Spinal Cord Med. 2011;34:16–21.
Acknowledgements
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). This document used data adapted from the Statistics Canada Postal CodeOM Conversion File, which is based on data licensed from Canada Post Corporation, and/or data adapted from the Ontario Ministry of Health Postal Code Conversion File, which contains data copied under license from ©Canada Post Corporation and Statistics Canada. Parts of this material are based on data and/or information compiled and provided by CIHI and the Ontario Ministry of Health. The analyses, conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred. Thank you to Jun Guan, Zhiyin Li, and staff at ICES for their contributions to this paper.
Author information
Authors and Affiliations
Contributions
All authors contributed to the development of this paper, its study design and interpretation of results. AS conceptualized the study, analyzed the data, interpreted results, and wrote the manuscript. SBJ guided the data analyses and development of manuscript. SBJ, KT, MP, AMM, and BCC helped with the overall interpretation of findings, and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The use of data in this project was authorized under section 45 of Ontario’s Personal Health Information Protection Act, which does not require further review by a Research Ethics Board. The use of the data in this project is authorized under section 45 and approved by ICES’ Privacy and Legal Office.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Senthinathan, A., Craven, B.C., Morris, A.M. et al. Examining antibiotic prescribing and urine culture testing for urinary tract infections (UTIs) in a primary care spinal cord injury (SCI) cohort. Spinal Cord 61, 345–351 (2023). https://doi.org/10.1038/s41393-023-00899-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-023-00899-x
This article is cited by
-
Identifying prescribers of antibiotics in a primary care spinal cord injury cohort
Spinal Cord Series and Cases (2024)