Abstract
Background
Use of inpatient palliative care (IPC) in advanced cancer patients represents a well-established guideline recommendation. A recent analysis demonstrated that genitourinary (GU) cancer patients benefited of IPC at the second lowest rate within the four examined primaries, namely lung, breast, colorectal, and GU. Based on this observation, we examined temporal trends and predictors of IPC use in metastatic prostate cancer patients receiving critical care therapies (CCT).
Materials and methods
We identified mPCa patients receiving CCT within the Nationwide Inpatient Sample database (2004–2015). IPC use rates were evaluated using univariable estimated annual percentage changes analyses. Multivariable logistic regression (MLR) models were used after adjustment for clustering at hospital level.
Results
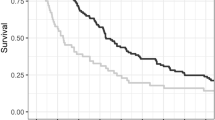
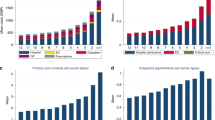
Of 4168 mPCa patients receiving CCT, 449 (11.3%) received IPC. IPC use increased from 1.2 to 22.3% (EAPC: +19.6%, p < 0.001). After stratification according to regions, race, and teaching status, the highest increase of IPC use was recorded in the South (from 0 to 25.4 %, EAPC: +27.6%), in Caucasians (from 1.5 to 24.4 %, EAPC: +19.8%; p < 0.001) and in teaching hospitals (from 0.9 to 26.2 %, EAPC: +19.6%; p < 0.001). In MLR models, teaching status (Odds ratio [OR]: 1.74, p < 0.001) and contemporary year interval (OR: 4.63, p < 0.001) were associated with higher IPC rates. Conversely, African American race (OR: 0.66, p < 0.001) and primary diagnosis of GU disorders (OR: 0.49, p < 0.001) and gastrointestinal (GI) disorders at admission (OR: 0.61, p = 0.02) were associated with lower IPC rates.
Conclusions
IPC use rate in mPCa patients receiving CCT sharply increased between 2004 and 2015. The highest increase of IPC use across time was recorded in the South, in Caucasian race, and in teaching hospitals. African-American race and nonteaching status were identified as independent predictors of lower IPC use and represent targets for efforts aimed at improving IPC delivery in mPCa patients receiving CCT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others

References
Morrison RS, Meier DE, Heart Y. Palliative Care - NCCN Guidelines. 2016:2582–90. https://doi.org/10.1056/NEJMc1511946.
Smith TJ, Temin S, Alesi ER, Abernethy AP, Balboni TA, Basch EM, et al. American Society of Clinical Oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol. 2012;30:880–7.
Ferrell BR, Temel JS, Temin S, Alesi ER, Balboni TA, Basch EM, et al. Integration of palliative care into standard oncology care: American society of clinical oncology clinical practice guideline update. J Clin Oncol. 2017;35:96–112.
Connors AF. A controlled trial to improve care for seriously iii hospitalized patients. J Am Med Assoc. 1995;274:1591.
Malin JL. Bridging the divide: integrating cancer-directed therapy and palliative care. J Clin Oncol. 2004;22:3438–40.
Greer J, Jackson V, Meier D.Early integration of palliative care services with standard oncology care for patients with advanced cancer. CA Cancer J Clin. 2001;63:137–52. https://doi.org/10.3322/caac.21192.
Meyers FJ, Linder J. Simultaneous care: disease treatment and palliative care throughout illness. J Clin Oncol. 2003;21:1412–5.
Davis MP, Bruera E, Morganstern D. Early integration of palliative and supportive care in the cancer continuum: challenges and opportunities. Am Soc Clin Oncol Educ Book. 2013:144–50.
Abrahm JL. Integrating palliative care into comprehensive cancer care. J Natl Compr Canc Netw. 2012;10:1192–8.
Temel JS, Greer JA, El-Jawahri A, Pirl WF, Park ER, Jackson VA, et al. Effects of early integrated palliative care in patients with lung and gi cancer: a randomized clinical trial. J Clin Oncol. 2017;35:834–41.
Temel JS, Greer JA, Muzikansky A, Gallagher E, Admane S, Jackson V, et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2010;363:733–42.
Loh KP, Bao M, Abdallah M, Shieh M. Use of inpatient palliative care services in patients with advanced cancer receiving critical care therapies. J Natl Compr Canc Netw. 2018;16:1055–64.
HCUP-US. NIS Overview. HCUP-US. Accessed 20 Jul 2018.
Loh KP, Kansagra A, Shieh M-S, Pekow P, Lindenauer P, Stefan M, et al. Predictors of in-hospital mortality in patients with metastatic cancer receiving specific critical care therapies. J Natl Compr Cancer Netw. 2016;14:979–87.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9.
Preisser F, Mazzone E, Nazzani S, Bandini M, Tian Z, Marchioni M, et al. Comparison of perioperative outcomes between cytoreductive radical prostatectomy and radical prostatectomy for nonmetastatic prostate cancer. Eur Urol. 2018;49:6–9.
Wadhwa V, Mehta D, Jobanputra Y, Lopez R, Thota PN, Sanaka MR. Healthcare utilization and costs associated with Gastroparesis. World J Gastroenterol. 2017;23:4428–36.
Feder S, Tate J, Womack J, Redeker N, Akgün K. Validation of the diagnostic code for palliative care in patients hospitalized with heart failure within the department of veterans affairs (S752). J Pain Symptom Manag. 2017;53:438–9.
Hua M, Li G, Clancy C, Morrison RS, Wunsch H. Validation of the V66.7 code for palliative care consultation in a single academic medical center. J Palliat Med. 2017;20:372–7.
Mulvey CL, Smith TJ, Gourin CG. Use of inpatient palliative care services in patients with metastatic incurable head and neck cancer. Head Neck. 2016;38:355–63.
Mazzone E, Nazzani S, Preisser F, Tian Z, Marchioni M, Bandini M, et al. Partial nephrectomy seems to confer a survival benefit relative to radical nephrectomy in metastatic renal cell carcinoma. Cancer Epidemiol. 2018;56:118–25.
Khandelwal N, Kross EK, Engelberg RA, Coe NB, Long AC, Curtis JR. Estimating the effect of palliative care interventions and advance care planning on icu utilization: a systematic review. Crit Care Med. 2016;43:1102–11.
May P, Garrido MM, Cassel JB, Kelley AS, Meier DE, Normand C, et al. Prospective cohort study of hospital palliative care teams for inpatients with advanced cancer: Earlier consultation is associated with larger cost-saving effect. J Clin Oncol. 2015;33:2745–52.
Abdollah F, Sammon JD, Majumder K, Reznor G, Gandaglia G, Sood A, et al. Racial disparities in end-of-life care among patients with prostate cancer: a population-based study. J Natl Compr Canc Netw. 2015;13:1131–8.
Author information
Authors and Affiliations
Contributions
Elio Mazzone had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mazzone, E., Mistretta, F.A., Knipper, S. et al. Temporal trends and social barriers for inpatient palliative care delivery in metastatic prostate cancer patients receiving critical care therapies. Prostate Cancer Prostatic Dis 23, 260–268 (2020). https://doi.org/10.1038/s41391-019-0183-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-019-0183-9
This article is cited by
-
Resource use in the last year of life of prostate cancer patients—A register-based analysis
Prostate Cancer and Prostatic Diseases (2023)
-
Palliative care and healthcare utilization among metastatic breast cancer patients in U.S. Hospitals
Scientific Reports (2023)