Abstract
Background
Metabolic bone disease is a common manifestation of celiac disease (CD). We aimed to assess fracture risk among children and adolescents with CD compared with a matched group.
Methods
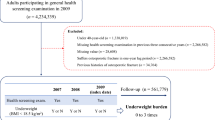
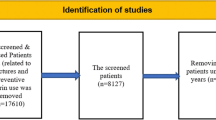
This registry-based cohort study included 2372 children with CD who were matched 1:5 to 11,860 children without CD. Demographic and clinical data were obtained from the electronic database of Meuhedet, a health maintenance organization. Fracture events at ages 1–18 years were identified by coded diagnoses.
Results
The overall fracture incidence rate was 256 per 10,000 patient-years (PY) in the CD group and 165 per 10,000 PY in the comparison group (p < 0.001). The hazard ratio (HR) to have a fracture was 1.57 (95% CI 1.43–1.73, p < 0.001) for the CD group compared to the matched group. The HR for multiple fractures was 1.67 (95% CI 1.38–2.01, p < 0.001). Analysis of the pre- and post-diagnosis periods separately showed that the HR for fractures in the pre-diagnosis period was 1.64 (95% CI 1.42–1.88, p < 0.001) for the CD group compared to the matched group, and 1.52 (95% CI 1.26–1.71, p < 0.001) in the period from diagnosis to the end of the follow-up period.
Conclusions
Children with CD had increased fracture risk both preceding and following the diagnosis of CD.
Impact
-
One manifestation of celiac disease (CD) is metabolic bone disease, including osteoporosis and impaired bone mineralization.
-
We found increased fracture risk among children with CD, both preceding the CD diagnosis and during the years following the diagnosis.
-
Recognition of the high risk of fractures in this population may help promote prevention.
-
Further studies are needed to evaluate changes in bone quantity and quality after initiation of a gluten-free diet, and to identify those at risk for persistent metabolic bone disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Lebwohl, B. & Rubio-Tapia, A. Epidemiology, presentation, and diagnosis of celiac disease. Gastroenterology 160, 63–75 (2021).
Caio, G. et al. Celiac disease: a comprehensive current review. BMC Med. 17, 142 (2019).
Gujral, N., Freeman, H. J. & Thomson, A. B. Celiac disease: prevalence, diagnosis, pathogenesis and treatment. World J. Gastroenterol. 18, 6036–6059 (2012).
King, J. A. et al. Incidence of celiac disease is increasing over time: a systematic review and meta-analysis. Am. J. Gastroenterol. 115, 507–525 (2020).
Andren Aronsson, C. et al. Association of gluten intake during the first 5 years of life with incidence of celiac disease autoimmunity and celiac disease among children at increased risk. JAMA 322, 514–523 (2019).
Collin, P., Vilppula, A., Luostarinen, L., Holmes, G. K. T. & Kaukinen, K. Review article: coeliac disease in later life must not be missed. Aliment Pharm. Ther. 47, 563–572 (2018).
Zanchetta, M. B., Longobardi, V. & Bai, J. C. Bone and celiac disease. Curr. Osteoporos. Rep. 14, 43–48 (2016).
Larussa, T. et al. Bone mineralization in celiac disease. Gastroenterol. Res. Pract. 2012, 198025 (2012).
Bianchi, M. L. & Bardella, M. T. Bone in celiac disease. Osteoporos. Int. 19, 1705–1716 (2008).
Xing, Y. & Morgan, S. L. Celiac disease and metabolic bone disease. J. Clin. Densitom. 16, 439–444 (2013).
Fedewa, M. V. et al. Celiac disease and bone health in children and adolescents: a systematic review and meta-analysis. J. Clin. Densitom. 23, 200–211 (2020).
Kondapalli, A. V. & Walker, M. D. Celiac disease and bone. Arch. Endocrinol. Metab. 66, 756–764 (2022).
Rubio-Tapia, A., Hill, I. D., Semrad, C., Kelly, C. P. & Lebwohl, B. American College of Gastroenterology Guidelines Update: diagnosis and management of celiac disease. Am. J. Gastroenterol. 118, 59–76 (2023).
Al-Toma, A. et al. European Society for the Study of Coeliac Disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. U. Eur. Gastroenterol. J. 7, 583–613 (2019).
Galindo-Zavala, R. et al. Expert panel consensus recommendations for diagnosis and treatment of secondary osteoporosis in children. Pediatr. Rheumatol. Online J. 18, 20 (2020).
Ciancia, S. et al. Osteoporosis in children and adolescents: how to treat and monitor? Eur. J. Pediatr. 182, 501–511 (2023).
Micic, D., Rao, V. L. & Semrad, C. E. Celiac disease and its role in the development of metabolic bone disease. J. Clin. Densitom. 23, 190–199 (2020).
Olmos, M. et al. Systematic review and meta-analysis of observational studies on the prevalence of fractures in coeliac disease. Dig. Liver Dis. 40, 46–53 (2008).
Heikkila, K., Pearce, J., Maki, M. & Kaukinen, K. Celiac disease and bone fractures: a systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 100, 25–34 (2015).
Hjelle, A. M. et al. Celiac disease and risk of fracture in adults—a review. Osteoporos. Int. 25, 1667–1676 (2014).
West, J., Logan, R. F., Card, T. R., Smith, C. & Hubbard, R. Fracture risk in people with celiac disease: a population-based cohort study. Gastroenterology 125, 429–436 (2003).
Ludvigsson, J. F., Michaelsson, K., Ekbom, A. & Montgomery, S. M. Coeliac disease and the risk of fractures – a general population-based cohort study. Aliment Pharm. Ther. 25, 273–285 (2007).
Jafri, M. R. et al. Long-term fracture risk in patients with celiac disease: a population-based study in Olmsted County, Minnesota. Dig. Dis. Sci. 53, 964–971 (2008).
Canova, C. et al. Risk of fractures in youths with celiac disease-a population-based study. J. Pediatr. 198, 117–120 (2018).
Husby, S. et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J. Pediatr. Gastroenterol. Nutr. 54, 136–160 (2012).
Lau, W. S., Heaton, P. A. & Paul, S. P. Improved adherence to the ESPGHAN Guidelines is necessary for diagnosing celiac disease in children: a single-center experience. Arq. Gastroenterol. 58, 164–167 (2021).
Tashtoush, L. B., Broad, S. R. & Paul, S. P. Pediatric celiac disease diagnosis and adherence to the ESPGHAN 2012 and 2020 Guidelines: a single centre experience. Arq. Gastroenterol. 59, 150–151 (2022).
Paul, S. P., Chan, Y. J. & Bailey, J. R. Diagnosing childhood celiac disease using ESPGHAN 2012 and 2020 guidelines: tighter adherence is required! Indian J. Gastroenterol. 39, 621–623 (2020).
Guz-Mark, A. et al. High rates of serology testing for coeliac disease, and low rates of endoscopy in serologically positive children and adults in Israel: lessons from a large real-world database. Eur. J. Gastroenterol. Hepatol. 32, 329–334 (2020).
Husby, S. et al. European Society Paediatric Gastroenterology, Hepatology and Nutrition Guidelines for Diagnosing Coeliac Disease 2020. J. Pediatr. Gastroenterol. Nutr. 70, 141–156 (2020).
Zacay, G., Dubnov-Raz, G., Modan-Moses, D., Tripto-Shkolnik, L. & Levy-Shraga, Y. Epidemiology of childhood fractures in Israel during 2000–2019. Bone 154, 116174 (2022).
Sanchez, M. I. et al. Risk of fracture in celiac disease: gender, dietary compliance, or both? World J. Gastroenterol. 17, 3035–3042 (2011).
Makharia, G. K. Current and emerging therapy for celiac disease. Front. Med. (Lausanne) 1, 6 (2014).
Grace-Farfaglia, P. Bones of contention: bone mineral density recovery in celiac disease-a systematic review. Nutrients 7, 3347–3369 (2015).
Verma, A. et al. Study of effect of gluten-free diet on vitamin D levels and bone mineral density in celiac disease patients. J. Fam. Med Prim. Care 11, 603–607 (2022).
Mora, S. et al. A prospective, longitudinal study of the long-term effect of treatment on bone density in children with celiac disease. J. Pediatr. 139, 516–521 (2001).
Bjorck, S., Brundin, C., Karlsson, M. & Agardh, D. Reduced bone mineral density in children with screening-detected celiac disease. J. Pediatr. Gastroenterol. Nutr. 65, 526–532 (2017).
Zanchetta, M. B. et al. Impaired bone microarchitecture improves after one year on gluten-free diet: a prospective longitudinal HRpQCT study in women with celiac disease. J. Bone Min. Res. 32, 135–142 (2017).
Zanchetta, M. B. et al. Improved bone microarchitecture in patients with celiac disease after 3 years on a gluten-free diet. Clin. Gastroenterol. Hepatol. 16, 774–775 (2018).
Lebwohl, B., Michaelsson, K., Green, P. H. & Ludvigsson, J. F. Persistent mucosal damage and risk of fracture in celiac disease. J. Clin. Endocrinol. Metab. 99, 609–616 (2014).
Mehta, P. et al. Gluten-free diet adherence in children with screening-detected celiac disease using a prospective birth cohort study. PLoS One 18, e0275123 (2023).
Barone, M. V. et al. Pivotal role of inflammation in celiac disease. Int. J. Mol. Sci. 23, 7177 (2022).
Mandile, R. et al. Mucosal healing in celiac disease: villous architecture and immunohistochemical features in children on a long-term gluten free diet. Nutrients 14, 3696 (2022).
Vici, G., Belli, L., Biondi, M. & Polzonetti, V. Gluten free diet and nutrient deficiencies: a review. Clin. Nutr. 35, 1236–1241 (2016).
McGrogan, L. et al. Micronutrient deficiencies in children with coeliac disease; a double-edged sword of both untreated disease and treatment with gluten-free diet. Clin. Nutr. 40, 2784–2790 (2021).
Jivraj, A. et al. Micronutrient deficiencies are frequent in adult patients with and without celiac disease on a gluten-free diet, regardless of duration and adherence to the diet. Nutrition 103–104, 111809 (2022).
Patwari, A. K. et al. Catch-up growth in children with late-diagnosed coeliac disease. Br. J. Nutr. 94, 437–442 (2005).
Assa, A. et al. Anthropometric measures and prevalence trends in adolescents with coeliac disease: a population based study. Arch. Dis. Child 102, 139–144 (2017).
Modan-Moses, D. et al. High prevalence of vitamin D deficiency and insufficiency in adolescent inpatients diagnosed with eating disorders. Int. J. Eat. Disord. 48, 607–614 (2015).
Oren, Y. et al. Vitamin D insufficiency in a sunny environment: a demographic and seasonal analysis. Isr. Med. Assoc. J. 12, 751–756 (2010).
Saliba, W., Rennert, H. S., Kershenbaum, A. & Rennert, G. Serum 25(OH)D concentrations in sunny Israel. Osteoporos. Int. 23, 687–694 (2012).
Aydemir, Y., Erdogan, B. & Turkeli, A. Vitamin D deficiency negatively affects both the intestinal epithelial integrity and bone metabolism in children with celiac disease. Clin. Res. Hepatol. Gastroenterol. 45, 101523 (2021).
Acknowledgements
The authors would like to acknowledge Cindy Cohen for linguistic support and for valuable remarks that contributed to the writing of this article.
Author information
Authors and Affiliations
Contributions
Y.L.-S., G.Z.: conception and design of the study and acquisition of data. G.Z., Y.L.-S., I.W., D.M.-M. and R.R.: analysis and interpretation of data. Y.L.-S., G.Z.: drafting the initial manuscript and editing it. All the authors reviewed the manuscript, revised it and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Meuhedet Health Services (number 01-10.06.20). Informed consent was not required, as the data were de-identified.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zacay, G., Weintraub, I., Regev, R. et al. Fracture risk among children and adolescents with celiac disease: a nationwide cohort study. Pediatr Res 95, 386–392 (2024). https://doi.org/10.1038/s41390-023-02826-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02826-5